Oral exams are a core component of the surgical education journey. We call it the practice of medicine for a reason. We believe that running through scenarios and algorithms aloud will help you be a better provider. When we practice, especially with good habits in a safe space, we allow responses to become ingrained, authentic, second nature.
The concept for this oral exam format was inspired by the plastic surgery qualifying and certifying exams. In plastic surgery, one cannot sit for their board examinations without completing at least one year of cases. Candidates prepare a binder of every case they did in that first year, along with photography of the outcomes. The examiners choose cases at random from this binder to conduct their examinations.
In 2020, Dr. Jamie Litvack and I came up with this modification to level-set the oral exam for the fourth-year student who enrolls in a four-week surgery rotation. We ask you to provide your course directors write-ups of three authentic cases. Samples and examples of such cases are listed in E.Flo MD. If it may help your examiners understand your case, please provide a de-identified photo or radiograph of the condition.
The examiners will write a script based off several Core Entrustable Professional Activities for Entering Residency. These typically follow a predictable format, although we may change the order of your submitted cases:
- Case 1: Presentation on morning rounds, informed consent.
- Case 2: Recognition of urgency or instability, transition, and handoff of care.
- Case 3: Calling a consult, informed consent for administration of blood products.
This will be followed by medical knowledge and clinical reasoning questions. A feedback session will be offered after a transcript is generated and assessed.
Students universally acclaim the exam as a valuable learning experience. Most even go as far as stating the exam was fun!
We wish you the best in your preparations. If you need any further assistance, please email surgery@wsu.edu.
Entrustable Professional Activities (EPAs) for entering residency

Oral presentation

Form clinical questions and retrieve evidence to advance patient care

Hand-offs and transitions of care

Recognition of patients with urgent or emergent needs

Informed consent

Consultations and referrals
Oral examination of fourth-year medical students on surgery rotations allows faculty to assess Core Entrustable Professional Activities for entering Residency (CEPAR): Proof-of-concept and analysis of student submissions. By Tamir Bresler, Erik Stiles, Shaina Schaeztel, Christopher Freeman, Ben Chia, Anjali Kumar. The American Journal of Surgery, Volume 225, Issue 5, 2023, Pages 841–846, ISSN 0002-9610, https://doi.org/10.1016/j.amjsurg.2023.01.020.
The Core Entrustable Professional Activities (EPAs) for Entering Residency. Association of American Medical Colleges.
Surgical rounds presentation
Preferred format for surgical rounds (surgical one-sentence summary)
Name, Age, Sex, POD # from X for Y, complicated by Z. Today the patient is XX (vitals, focused exam). Discharge plan is YY (describe anticipated barriers to discharge and follow-up plan).
An example of how a student typically presents:
This is a 71-year-old male who was admitted for acute appendicitis and underwent laparoscopic or exploratory laparotomy, revealing a ruptured appendix secondary to acute appendicitis. The removal was completed successfully, and a surgical drain was left in place, connected to bulb suction. The patient was started on IV Zosyn. Post-operatively, he has been doing well, with a return of bowel function, passing gas and stool, and tolerating diet without any concerns. He is anticipated to be discharged later today on oral antibiotics and will be seen in the clinic in about a week for the removal of the drain, which has continued low output.
A model example of what the examiners are looking for instead:
Mr./Ms. X is a 71 yo M POD #2 from laparoscopic appendectomy for ruptured appendicitis with (describe extent of purulence—localized / walled-off, or peritonitis?) necessitating intraoperative drain placement near the appendiceal stump and postoperative IV Abx. On exam, his vitals are stable, abdomen soft, wounds clean and drain output clear. He is eating, walking and has been transitioned to oral antibiotics with a resolution of his prior leukocytosis to X. He’s ready for discharge today after drain care teaching with follow up in a week for drain removal
Form clinical questions and retrieve evidence to advance patient care
- Review the surgical anatomy.
- Know the most common complications of the procedure you are discussing.
- Familiarize yourself with the top diagnostic (how to pare down the ddx) and management tricks for each complication.
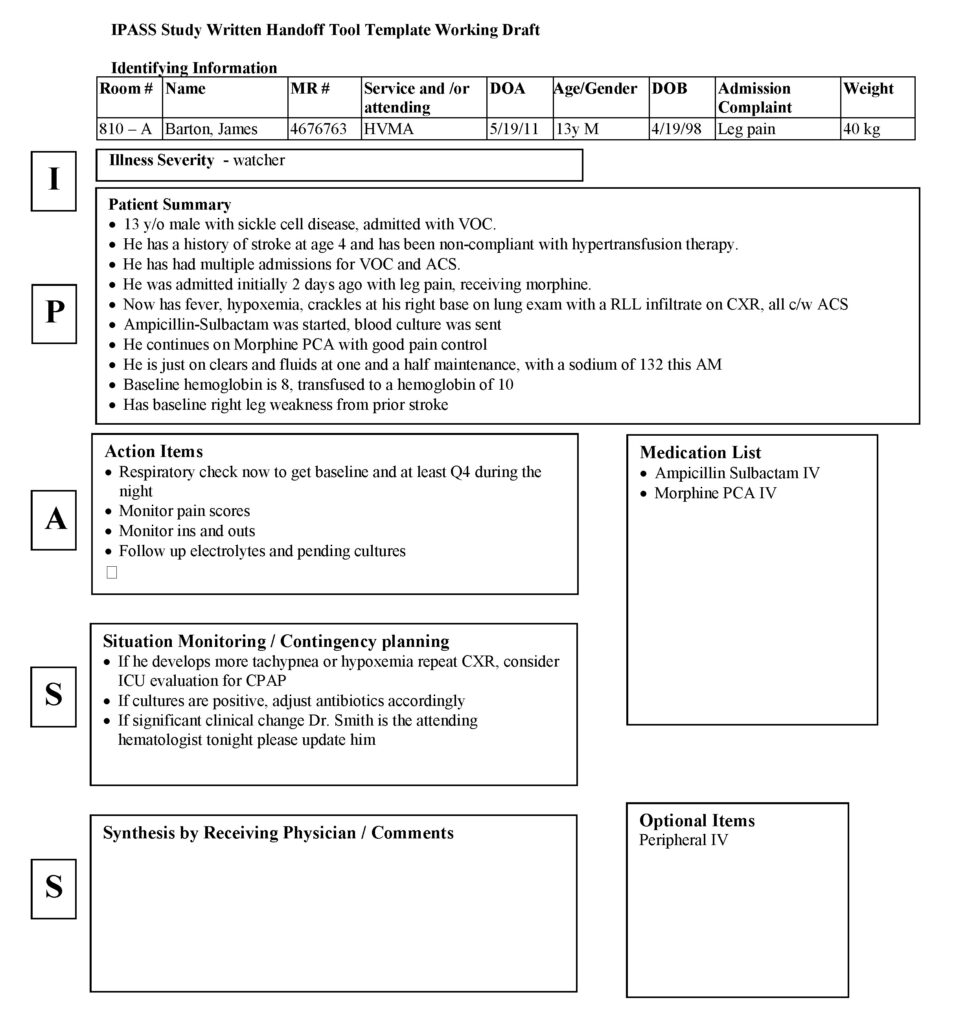
Transitions and hand-offs of care
IPASS handoff
- I
Illness severity
- Stable, “watcher,” unstable
- P
Patient summary
- Summary statement
- Events leading up to admission
- Hospital course
- Ongoing assessment
- Plan
- A
Action list
- To-do list
- Timeline and ownership
- S
Situation awareness and contingency planning
- Know what’s going on
- Plan for what might happen
- S
Synthesis by receiver
- Receiver summarizes what was heard
- Asks questions
- Restates key action/to-do items
Sample verbal handoff
- I
Illness severity
Ok, this is our sickest patient, and he’s full code.
- P
Patient summary
AJ is a 4-year-old boy with a history of ex 26-week gestation admitted with hypoxia and respiratory distress secondary to a left lower lobe pneumonia. He presented with cough and high fevers for 2 days before admission, and on the day he presented to the emergency department, he had worsening respiratory distress. In the emergency department, he was found to have an Na of 130, likely secondary to volume depletion versus syndrome of inappropriate secretion of antidiuretic hormone. He received a fluid bolus and was started on O2 at 2.5L. He is on Ceftriaxone.
- A
Action list
Please look in on him at approximately midnight and make sure his vitals are unchanged and his oxygen saturation is stable. Check to determine if his blood culture is positive tonight.
- S
Situation awareness and contingency planning
If his respiratory status worsens, please get another chest radiograph to determine if he is developing an effusion.
- S
Synthesis by receiver
Ok, so AJ is a 4-year-old ex-premie admitted with hypoxia and respiratory distress secondary to a left lower lobe pneumonia on Ceftriaxone, O2, and fluids. You want me to check on him at midnight to make sure he’s stable and check his blood culture. If his respiratory status worsens, I will repeat a radiograph to look for an effusion. I think I have it.
ICU-PAUSE components
- I
Illness severity
- C
Code status
- U
Uncertainty in diagnosis
- P
Patient summary
- A
Action list
- U
Urgency and follow-up
- S
Situational awareness and contingency planning
- E
Expected disposition
Recognition of urgency and instability
Example algorithm:
Vital Signs: Check blood pressure, respiratory rate, oxygen saturation, and temperature.
Physical Examination: Assess for signs of distress, pain, bleeding, or infection. Listen to heart and lung sounds.
Review Medical History: Look for any history of similar issues, medications, or recent events that could contribute to issue.
Ensure vital signs.
Suggest therapeutics.
Planning for future (i.e., type and cross for blood transfusion, call the OR to expect reoperation).
Calling for consultation
Informed consent
- R
Rationale
What the diagnosis is, why you’re having a discussion to obtain consent. If possible, compliment them. Thank them for coming in.
- P
Procedure (in lay terms)
If you use scientific jargon, make sure to explain what it means. For example, if a particular procedure is written on the consent, describe what that means anatomically. To put them at ease, let them know about how long the operation typically takes.
- A
Alternatives
The first is to opt out of surgery. That is their choice. Just because you are there to get their consent doesn’t mean they have to give it.
- B
Benefits
Now explain why you and your team think the procedure is best for them. Focus on safety in the short and long term.
- R
Risks
List the most common (perhaps three). Focus on the risks of surgery, since the anesthesiologist will talk to them about the risks of anesthesia. Reassure them that you do everything you can to keep those risks to a minimum.
- Q
Questions
Show empathy. “That was a lot of information, and although I went through it quickly, I have lots of time to explain anything you wish in more detail. What questions do you have?”
Sample informed consent
Scenario is a 20 yo F with acute appendicitis. By the CT scan, it is early (not ruptured) and is intraperitoneal.
- R
Rationale
Miss X, my name is ____, and I’m the intern on the surgery service. I’d like to take a few minutes to talk with you about this consent form I have here. From the CT scan, my team sees that the cause of your discomfort is most likely due to your appendix. It’s an organ on the right side of your colon (large intestine) that commonly causes problems like this. Fortunately, it’s an organ we can live without. In your case, it is inflamed, but thanks to your awareness and your efficiency getting here, we’ve been able to catch it so early that it hasn’t ruptured.
- P
Procedure (in lay terms)
We believe that the best thing to do is a small surgery to remove the appendix. That surgery is called a “laparoscopic appendectomy.” I know surgery may sound scary and risky, but I want to reassure you that this particular surgery is very straightforward. It takes us around 30 minutes. What we propose to do is insert a camera and small instruments into the abdomen to view the appendix, then isolate it and divide it. We put it in a bag to remove it out of your belly button incision and send it to pathology for them to look at it under a microscope.
- A
Alternatives
One alternative is that you opt not to have surgery. In that case, we’d treat you with antibiotics alone: some we’d give in the hospital—like what you’re getting now through your IV—plus a two-week course at home. The team recommends surgery because in 20–30% of cases, those treated with antibiotics will recur within the year and need emergency surgery. But it’s definitely your choice and your preference.
- B
Benefits
The benefits of surgery is that you’re here already, and it’s a definitive solution to your condition.
- R
Risks
There are risks with surgery, including bleeding, infection, and damage to surrounding structures. We do everything we can to keep those risks to a minimum.
- Q
Questions
I realize was a lot of information, and although I went through it quickly, I have lots of time to explain anything you wish in more detail. What questions do you have?
More reading about informed consent
Best Practices: PARQ in Clinical Record Keeping
Frequently asked questions: Surgery oral exams
Who grades the exam?
A minimum of two board certified surgeons. One is usually the course director. One is usually someone who specializes in the discreet field.
How can I view the transcript of my exam?
The transcript is uploaded to E.Flo MD in the Course Director Handback Response field. The VCC and the course director will upload this within 3 business days after your exam.
How can I view the video from my exam?
The video is uploaded to your SimCapture account. This is the same account as you use to see your OSCE performance.
How is the exam graded?
- The graders review the transcript, and sometimes they view the video.
- The examiner’s script for each case covers two skills. The graders use a rubric for a score (0–5) in each skill. The informed consent skill usually has two opportunities to perform. The score is averaged.
How do I get my scores for each of the skills?
The graders use a form which summarizes your transcript, gives a score and the rationale for that score. Typically, the rationale will explain what was / would have been expected to receive a higher score.
How is the professionalism/teachability/engagement component graded?
- Punctuality and politeness are important to the graders.
- Accepting the calendar invitation without prompting is appreciated.
- Appearance and poise are also judged. This is done to prepare students for interview season. Surgery program directors and faculty at residency training programs will expect a certain formality.
- Center your face in the top 1/3 of your computer screen. Make sure your face is well-lit. Use a simple virtual background if your ambient background is dark or distracting. Make sure your device is charged and that there is stable wifi. Make sure you are in a quiet environment, and that your audio is optimized so examiners can hear. Make sure you speak clearly so the transcription software can work optimally.
- Slouching, slang, disheveled hair, wearing scrubs without a white coat, and wearing a hat are all discouraged. You should aim to appear at least as put together as your surgeon proctors.
Can I use resources during the exam?
You can have your cases in front of you. If you need to, you can take notes. We don’t mind if the mnemonics are in front of you (if you need to glance at them). However, reading pre-prepared materials out loud or use of AI during the exam is strictly prohibited. Examiners may ask to view your workspace or your hands during an exam to ensure academic integrity.
What if I have tech difficulties during the exam?
Each exam is allotted 30 mins. If your tech issue can be solved and we can accomplish a full exam within that time, then there will be no need for reattempt. If the exam is compromised by tech, it will be rescheduled.
When will my grade for the exam be posted?
We aim to have the exam grade posted within 10 business days of the exam. The grade will appear in E.Flo MD.
How is the course graded?
A grading panel meets within 2 weeks of the last date of your rotation. If the grading panel has adequate data to determine your grade, they will. That grade is then posted to E.Flo MD.
What if I fail my oral exam?
- Especially for first-time takers, failing the exam is a possibility. If you fail, you will be offered coaching before your reattempt. Those students who fail the oral exam on the first attempt will not be honors-eligible at the second attempt.
- Those who fail the exam twice will require significant coaching before the third attempt, because failure on the third attempt equates to failure of the course.
What if I get a Satisfactory score on the oral exam?
If you are a first-time oral exam taker and you wish to reattempt, you may request this in writing to surgery@wsu.edu within 2 weeks of the posting of your exam grade. You must view your original exam video before your reattempt. At least one coaching session is required before your reattempt. Your two attempts will be averaged to determine the final grade.
What is the timing of exam coaching and reattempts?
Grades need to be finalized within 6 weeks of the course ending. In exceptional cases, if a grade change is warranted, it can be requested via the formal appeals process.
How do I get cases to the examiners for my oral exam reattempt?
The course directors will provide you with a variety of cases which have been written up by other students. You can pick which three you wish to use for your oral exam retake. You will need to compile them into a single PDF and submit them to the examiners at least 72 hrs before your reattempt.
Image credits
Unless otherwise noted, images are from Adobe Stock.