 The kidneys tend to be innocent bystanders that suffer secondary to systemic illness or failure from another organ system. Acute kidney injury is extremely common in the hospital.
The kidneys tend to be innocent bystanders that suffer secondary to systemic illness or failure from another organ system. Acute kidney injury is extremely common in the hospital.
The first question to ask yourself is whether or not the patient needs emergent dialysis. The answer is almost always No. Here is a helpful mnemonic to help you decide if a patient needs emergent dialysis.
Does the Patient Need Emergent Dialysis?
A: Acidemia Refractory to supplemental sodium bicarbonate. If you can't get the pH to 7.1 the patient probably needs emergent dialysis. Between 7.1 and 7.2 is somewhat of a gray area.
E: Electrolyte Abnormalities. Generally hyperkalemia that cannot be satisfactorily lowered without dialysis. For example, despite treatment the potassium remains above 6, and the EKG shows persistent abnormalities.
I: Intoxication. For example, severe salicylate, ethylene glycol, or lithium toxicity.
O: Overload. Volume overload not controlled with diuretics, for example pulmonary edema and impending respiratory failure or refractory hypoxemia despite mechanical ventilation,
U: Severe Uremic Complications. For example, severe encephalopathy that puts the patient into a coma.
No matter what the creatinine number, unless they need emergent dialysis, or we need nephrology’s input for some other reason, nephrology doesn’t usually need to see the patient until the morning.
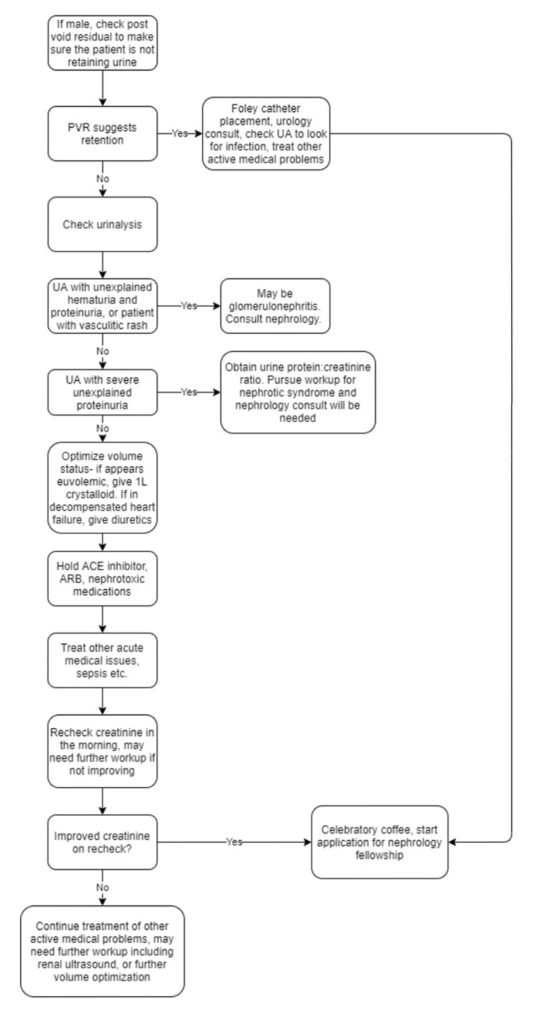
The next step is to figure out what is causing the renal failure. In general, I use the following strategy.
Image credit: Eric Tanenbaum.