The ICU (From a Hospitalist Perspective)
This section can be used as a reference for caring for your critically ill patient until they have been safely transferred to the care of an intensivist.
These are huge, complicated topics, the details of which are outside the scope of this rotation. Below is a basic framework to help you when things are not going well.
Shock and Vasopressors
Your patient is persistently hypotensive, and their condition is immediately life threatening:
-
Categorize the type of shock:
Septic
Hypovolemic
Cardiogenic
Obstructive
Neurogenic -
Unless clearly cardiogenic shock, the first step is volume resuscitation.
Hypovolemic shock should rapidly improve with fluids.
Hemorrhagic shock should rapidly improve with blood or fluids. -
If the patient is still hypotensive after volume resuscitation
(for example, standard 30cc/kg crystalloid bolus), start vasopressors. Sometimes you can either clinically—or with the help of special techniques (NICOM device, pulse pressure variation, etc.)—determine that the patient should get more volume instead of starting pressors, but pressors are generally indicated at this point, to get the MAP above 65 (conventional goal) or 60 (maybe equivalent outcomes to 65).
The initial pressor of choice is almost always norepinehprine (brand name Levophed). -
For cardiogenic shock, add dobutamine 2.5–5.0 mcg/minute.
-
If the patient needs a moderate dose
(8–10 mcg/minute and worsening) of norepinephrine for septic shock, add vasopressin at a fixed dose (0.03 or 0.04 units/minute).
-
If escalating doses of norepinephine and fixed-dose vasopressin are not enough
Consider adding epinephrine—but at this point, you should have input from the intensivist.
-
If the shock is caused by a bradyarrhythmia
You can try atropine. After that, your options are transcutaneous pacing, dopamine, or epinephrine.
-
Bonus tip
If you REALLY need pressors but don't have immediate access to a bag of norepinephrine, you can open the code cart and mix 1cc of an amp of code dose epinephrine with 9cc of saline from a flush to make "push dose epinephrine," which can then be given 1cc q3–5 minutes until norepinephrine arrives.
The other "push dose" pressor is phenylephrine, which can be given in similar volumes and intervals if this is available in your code cart.
Respiratory Failure
- For patients without cardiogenic pulmonary edema, escalation of oxygen therapy should be as follows: nasal cannula high flow nasal cannula (HFNC, may need a non-rebreather mask until HFNC is in place) intubation.
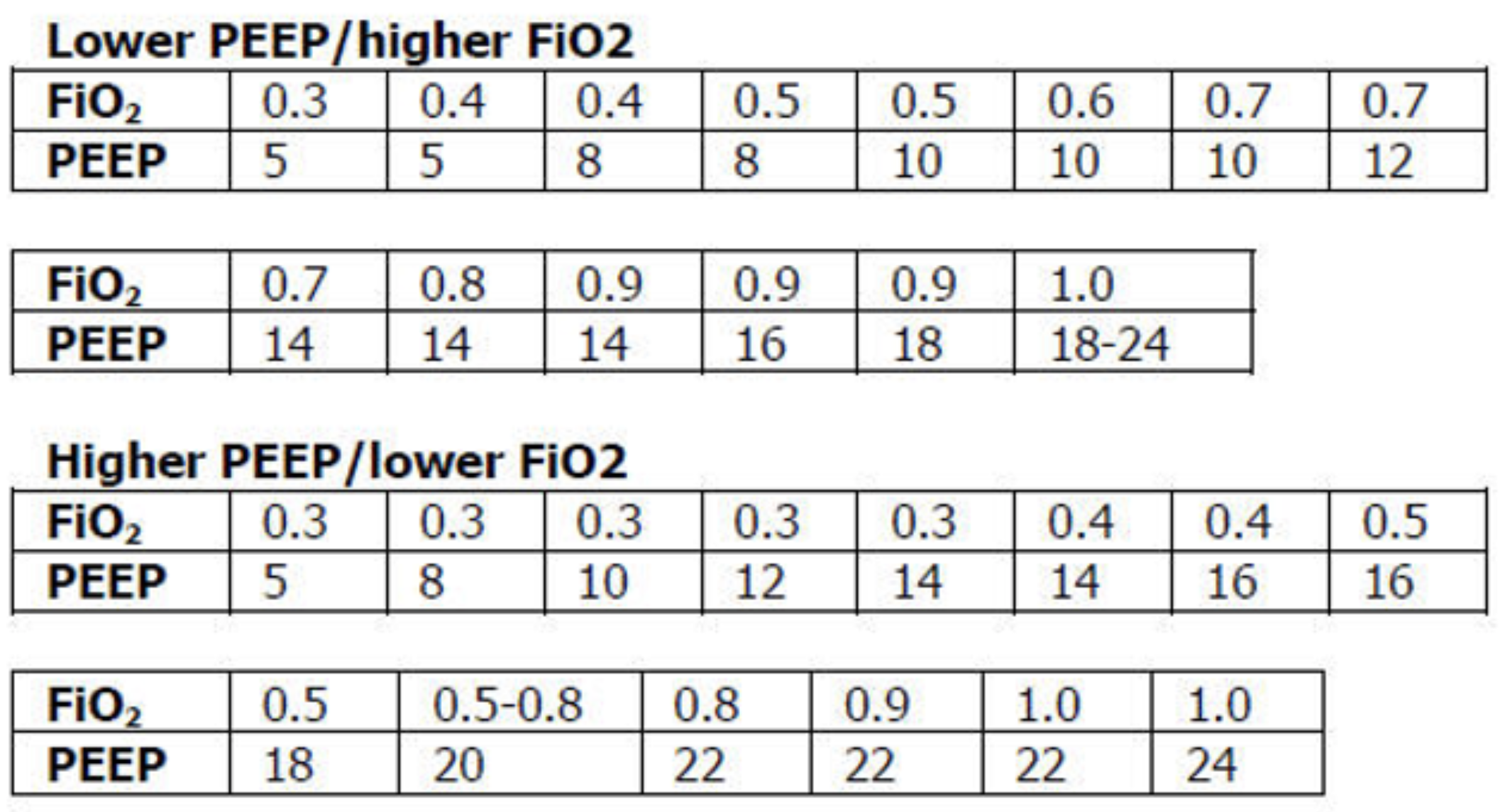
- If your patient needs to be intubated for ARDS and they are persistently hypoxemic, escalate their PEEP and oxygen using the “PEEP ladder” (below), and consider prone positioning and neuromuscular blockade if they have severe ARDS or refractory hypoxemia.
- For patients with cardiogenic pulmonary edema, escalation of oxygen therapy should be nasal cannula CPAP intubation.
- Don’t over-oxygenate the patient. Keep the oxygen level above >92% and <98% in most cases.
- To improve hypercarbia, the patient needs to breathe a greater total volume of air per minute to “blow off” their CO2. This can be done with BiPAP or mechanical ventilation.
- If BiPAP is not lowering the CO2, try troubleshooting by increasing the driving pressure (inspiratory pressure minus expiratory pressure, this is often done by increasing the inspiratory pressure), respiratory rate, or improving mask fit. Work with the RT on this.