Overview
 Heart failure is a huge topic. This is a brief overview of the basics with a focus on initial management. Going forward, let’s assume that your patients are not in cardiogenic shock, which is outside the scope of this website and is more of a critical-care topic.
Heart failure is a huge topic. This is a brief overview of the basics with a focus on initial management. Going forward, let’s assume that your patients are not in cardiogenic shock, which is outside the scope of this website and is more of a critical-care topic.
First, make the diagnosis. There are many things that suggest a diagnosis of heart failure. After a thorough history, physical, indicated lab testing, and imaging, all the data should be interpreted together. Some of the most important things to look for:
- History: Shortness of breath, paroxysmal nocturnal dyspnea, orthopnea, leg swelling, and weight gain
- Physical exam: Low or low-ish BP with narrow pulse pressure, edema, elevated JVP, and weight gain per review of EMR data
- Lab testing: Elevated BNP, especially if significantly elevated compared to prior values
- Imaging: Pulmonary edema, cardiomegaly
The initial management depends on whether or not this is a new diagnosis of heart failure.
New Diagnosis of Heart Failure
For a new diagnosis of heart failure, the patient needs a TTE (transthoracic echocardiogram), which will guide further workup and management:
- What is the ejection fraction?
- Is there a valvular problem?
For new systolic heart failure or significant valvular disease, a cardiologist should be consulted. The patient will need diuresis for volume overload as explained below.
For an Exacerbation of Existing Heart Failure
-
Try to figure out what caused it. Is the patient having an MI? Are they taking their medications? Eating tons of salt? Is their existing cardiomyopathy worsening?
-
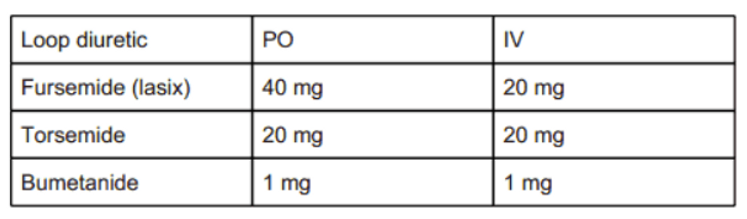
Remove fluid with diuresis. A good rule of thumb is to start with double their existing dose of outpatient diuretics. Generally, I start with IV furosemide, look up loop diuretic conversion charts to determine the correct dose or see an example below. Although this is not 100% accurate, we usually say that PO furosemide is 50% as potent as IV furosemide. If you take the patient's PO dose and give it IV that is a good place to start. If the patient is not having significant urine output in an hour or two, try to double the dose again. Once you have an effective dose, schedule it twice a day to start.
-
If the patient is not on a diuretic, a good place to start is multiplying the creatinine by 20 and giving about that much IV lasix.
-
Have the patient on telemetry, monitor daily weights, intake and output, low-salt diet. (Interestingly, the low-salt diet is controversial, but it is the standard of care for now.)
-
At least at first, monitor BMP and Mg twice a day. Keep the potassium 4 or above and the magnesium 2 or above. Keep an eye on the creatinine.
-
What is the goal daily net negative volume balance? Different cardiologists say different things, but essentially get the fluid off as fast as the patient can tolerate without them developing hypotension, renal injury, or significant electrolyte abnormalities.
There is a difference in how patients with preserved versus reduced ejection fraction are managed. For patients with preserved ejection fraction, diuresis and cardiac risk factor modification are the goals.
For patients with reduced ejection fraction, (< 40% – 50%), there are multiple medications that have been shown to improve important outcomes such as mortality. If your patient is not on the below medications, figure out why not and if they need to be started. These medications are referred too broadly as “guideline directed medical therapy.”
-
ACE Inhibitors/ARBs/ARNI
These are great because they often make the patient feel better by decreasing the afterload. If everything else is optimized and the patient is still symptomatic and/or having frequent admissions, sacubitril/valsartan is often considered, which is the only ARNI.
-
Beta Blockers
Interestingly, there are three seemingly magic beta blockers with better outcome data than the others. These are carvedilol, metoprolol succinate, and bisoprolol (rarely used in the United States). Carvedilol is dosed twice a day and has more of an effect on BP, which is good for patients who are hypertensive. Metoprolol succinate is dosed once a day and is more BP neutral, so it is useful in patients with borderline low BP or those who have issues with medication adherence.
-
Aldosterone Antagonists
Spironolactone and eplerenone. Usually spironolactone is used first as it is cheaper. However, if gynecomastia is developing switch to eplerenone.
-
SGLT-2 inhibitors
These improve cardiac outcomes and can also have a beneficial effect on weight, glycemic control, and renal function.
For patients with heart failure leading to significant respiratory failure from pulmonary edema, CPAP can be very helpful, as the PEEP (positive end-expiratory pressure), it provides decreases in both cardiac preload and afterload.
Finally, “flash pulmonary edema,” also known as S.C.A.P.E. (sympathetic crashing acute pulmonary edema), is managed a little bit differently. These patients present very hypertensive in acute respiratory distress. The initial management should actually be CPAP and rapid BP lowering, usually with a nitroglycerin bolus and drip. These patients may require diuresis as well, but sometimes they are not significantly volume overloaded. The cornerstone of initial management is PEEP via CPAP or BiPAP and BP control.
Image credit: Jehan de Grise and his workshop, “The Heart Offering,” 1338–1344. Illustration from The Romance of Alexander, Bodleian Library, Oxford, England.
