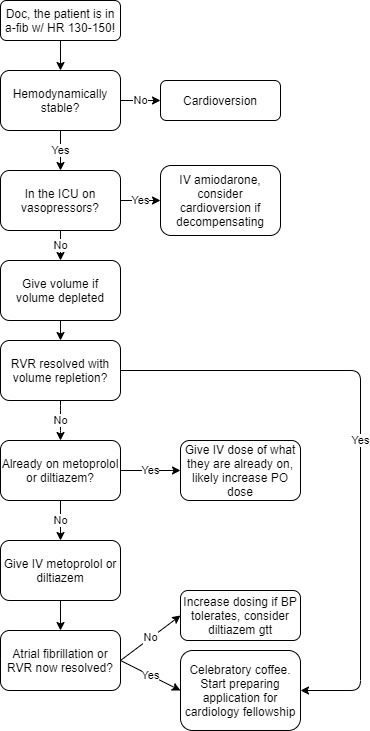
 Atrial fibrillation is a very common arrhythmia in the hospital. Fortunately, it is usually easy to manage. In general, I treat a-fib with RVR in the following way:
Atrial fibrillation is a very common arrhythmia in the hospital. Fortunately, it is usually easy to manage. In general, I treat a-fib with RVR in the following way:
As you start to follow this algorithm, you should simultaneously try to identify the provoking factor for the atrial fibrillation (if new) or RVR.
-
- Is the patient septic?
- Volume depleted?
- Is the magnesium low?
- Do they have a PE?
- Etc.
Patients should have their volume status optimized and electrolytes checked with attention to magnesium and potassium.
More Specifics on the Medications
-
Metoprolol
Preferred in patients with heart failure or MI. Try up to 3 IV doses of 5mg. Esmolol is an IV beta blocker that comes as a titratable infusion, but it can only be used in the ICU and is rarely necessary.
-
Diltiazem
If a couple IV doses (10–20mg) are ineffective, can be given as a titratable IV infusion.
-
Amiodarone
Good for short-term use in critically ill patients, but the many potential toxicities limit long-term use.
-
Digoxin
If you are running into hypotension with metoprolol or diltiazem, a loading dose of digoxin can be a useful adjunct, especially for a patient with systolic heart failure. Not always a great long-term medication.
TSH is often abnormal in hospitalized patients. Only check this if you have a reasonable suspicion for hyperthyroidism. Consider MI, but in general, avoid checking a troponin for isolated a-fib w/ RVR. (However, if the patient is having new chest pain, and needs a work up for ACS independent of their a-fib, then troponin and EKG need to be checked.)
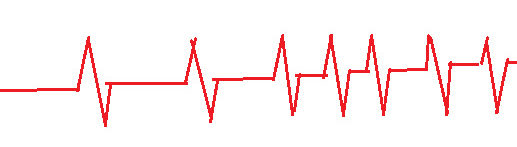
Image credit: Eric Tanenbaum.