Computed Tomography (CT) is the marriage of computers and X-rays. In modern machines, a rotating gantry holds a specialized X-ray tube, which generates a highly contoured X-ray beam in opposition to a detector array surrounding the patient. The patient moves through the gantry.
Gantries weigh around 6,000 kilograms and can achieve speeds of 300 milliseconds per rotation, operating at the limits of material strength engineering. This speed is generally fast enough to stop cardiac motion if the patient is not tachycardic.
Here is a typical CT gantry in motion without the cowling.
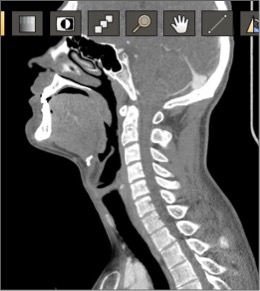
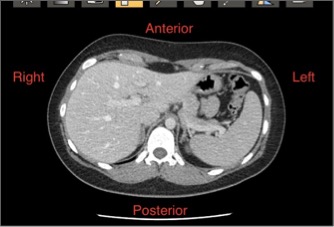
CT and MRI image orientation
Density measuring
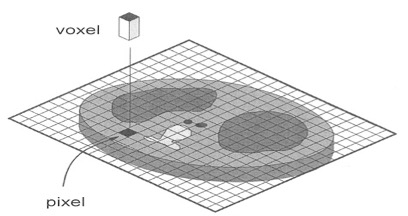
The image is made of an array of pixels (picture elements), typically in a 1024×1024 matrix. Each pixel represents the X-ray volume density of tissue or voxel.
A typical pixel is about 1×1 mm. The volume of tissue it represents depends on the slice thickness. Both parameters are controlled by the CT radiology technician, who can affect resolution.
Hounsfield scale
The Hounsfield scale is an arbitrary scale of X-ray density where water is assigned a Hounsfield Unit (HU) of 0, Air −1000 HU, Bone/metal + 1000HU. This scale may be expanded or contracted. Fat is negative HU. In general, the HU is translated into an optical density for display on film or a computer screen, so values are relative. On occasion, the absolute value in Hu can be informative, such as proving fat or calcium content of a finding.
Density of tissues on CT
Air < Fat < Fluid < Soft tissue < Bone < Metal
A way to remember this: Fat floats on water, so it is less dense than fluid; soft tissue is mostly intracellular fluid with some connective tissue.
Air: −1000 HU.
Lung: −500 HU (partially air, partially soft tissue).
Fat: −50 HU (slightly less dense than simple fluid).
Water: 0 HU.
Soft tissue (and blood): +50 HU (slightly more dense than simple fluid).
Bone: +1000 HU (much more dense).
A note on resolution
Resolution is the ability to separate two adjacent objects. There are two components to resolution: Spatial and Contrast.
Spatial resolution refers to how close (or small) two objects can be in space and still be separated visually.
Contrast resolution refers to how similar two adjacent structures X-ray density can be and still be detected as different objects.
There is interplay between the two. Two objects with marked different densities (e.g., a fracture where there is bone/fat/bone interface) can achieve sub-millimeter spatial resolution. On the other hand, liver metastasis may only have a 20 Hu difference between normal liver and the metastasis, so the growths would have to be large to be seen as separate from the normal liver tissue.
Before an imaging test is requested, consider:
Contrast and spatial resolution can be greatly affected by decisions made by the imager in selecting scanning parameters and use of contrast materials.
Radiographic contrast agents
Intravenous and oral contrast can be utilized to improve resolution, but this can be a double-edged sword. A typical metastasis in the liver will become less dense than normal liver after injection of intravenous contrast. However, this effect may only last two minutes when the metastasis may become isodense to liver tissue, and therefore, undetectable. High-density oral contrast can obscure a stone in the bile duct.
Windows and levels
It turns out that the human visual system can only work with about 32 shades of gray without fatigue and loss of perception, so CT images are limited to 32 shades of gray (color is too distracting for standard use). Therefore, data must be excluded from the image using a Window defining how many CT numbers to display centered on a particular Level. All data below the negative end of the window is assigned black; all density data above the upper-positive end is assigned white. Bone has a very wide range of CT densities from fat (−1000) to bone (+1000), so a wide window is necessary. The Liver has a narrow range of densities, so a narrow window is used to increase conspicuity of metastasis, which may vary little from normal liver density. Window and level settings are chosen for final image presentation to best display anatomy and pathology, but can be altered later on PACS systems.
You can see this in action on a PACS system.
Patient preparation

Patient preparation varies with the exam and what information is sought. Too often, a generic exam is performed, as the imaging professional does not have all the necessary clinical data to do a targeted exam. Most of the time, a generic exam is all that is needed, but in special circumstances consultation with your imaging team can yield a superior exam.
Intravenous contrast is frequently used to increase lesion detection. Liver metastasis detection increases on the order of 10–20% with intravenous contrast. Knowledge of the type of tumor may alter contrast injection and timing. Oral contrast is an option to evaluate the bowel. Because of gut transit time, a patient may have to drink and wait 1–2 hours to opacify the bowel. Having the patient pick up contrast the day prior to the exam can mitigate this. Oral contrast is being used less frequently with advances in imaging machines.
Modern CT scanners can scan a patient in under two minutes, so patients can be added on top of a busy day.
Cautions with intravenous contrast agents
Intravenous contrast can interact with Metformin (a commonly used drug in diabetes control), rarely inciting lactic acidosis. Patients with low GFR (glomerular filtration rate, a determinate of renal function) may have exacerbation of renal impairment, particularly if diabetic or dehydrated. This is an evolving issue, and imaging partners should be consulted either in person or by their website. The patient normally should be well hydrated. Some labs will check eGFR and hydrate patients prior to the exam, causing increase in total exam time.
Allergic-like reactions to IV contrast occur infrequently with nonionic contrast agents, and fatal reactions are now rare.
Patients may need to be NPO, as contrast injection can induce vomiting and food within the stomach can mimic masses.
There is usually detailed information on your imaging colleague’s website.
CT exams
Rapid assessment with CT, but brain MRI is much more sensitive.
- Trauma.
- Stroke (does your institution have stroke protocol?).
- Tumor.
- Subarachnoid and Subdural hemorrhage.
- Perfusion.
- High spatial resolution.
- Rapid and reliable.
- Best for evaluating the bones of the spine.
- MRI of the spine necessary to evaluate the spinal cord and visualize the ligaments and intervertebral discs of the spine.
- CT of the spine best in the trauma setting to evaluate for fracture or mal-alignment.
- Tumors.
- Solitary Pulmonary Nodule.
- Lung Cancer Screening.
- Aortic dissection/aneurysm.
- Gallbladder (80–90% stones).
- Liver Mets (>90%).
- Hepatoma (?80%).
- Appendix (95%).
- Pancreas targeted exam.
- Kidney Stones (100%).
- Tumor.
- Female Pelvis (special circumstances) US and MRI are superior.
- High spatial resolution ideal for fractures.
- Poor for tumors MRI superior.
- 3-D rendering Rx planning.
Competitive/complimentary to MR Angiography (MRA), Catheter angiography.
- Diverticulitis.
- Crohn’s.
- Obstruction.
- Becoming go-to tool for bowel evaluation but limited mucosal detail.
- Rapid assessment.
Image credits
Unless otherwise noted, images are from Adobe Stock.