Disclosures
No conflicts to disclose.
Sam is a 45-year-old who presents to inquire about their breast cancer risk and when to begin mammography. She has no known family history of breast or ovarian cancer. Menarche was at age 13. Her first child was born when she was 27, and she was briefly on hormonal birth control for three years at age 20. She drinks alchohol 2–3 times a week, usually one glass of wine per sitting. She denies radiation exposure. Her BMI is 34.
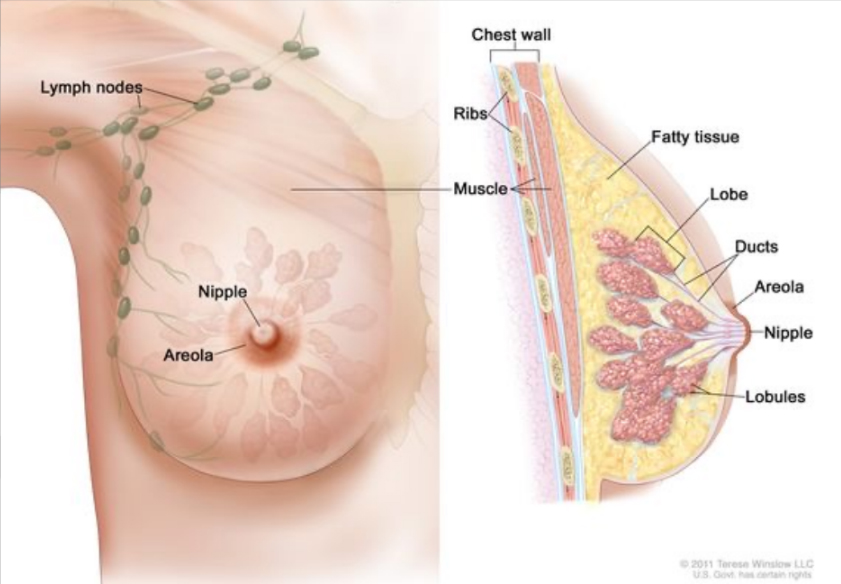
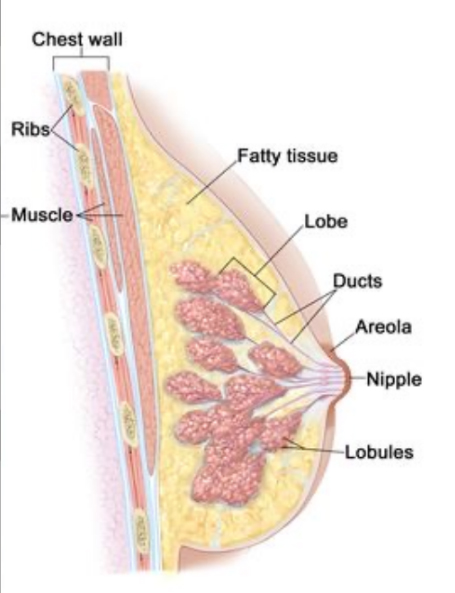
Breast anatomy review
Noncancerous breast disease
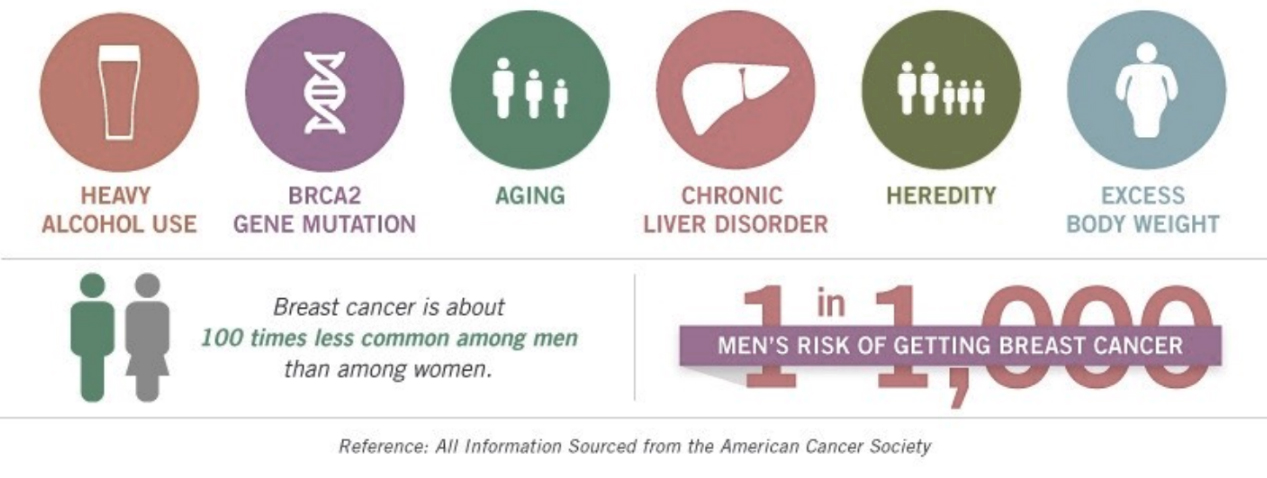
Breast Cancer Risk
Estrogen exposure
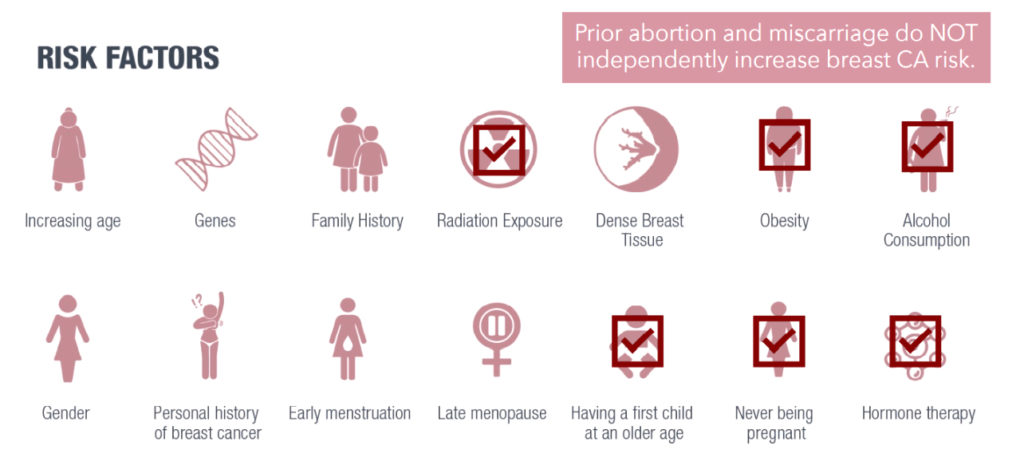
Other breast cancer risk
Motivational interviewing
Sufficient/convincing evidence
Increase Risk
- Alcohol consumption.
- Body fatness (post-menopausal).
- Adult height (post-menopausal).
- Any use of oral contraceptive pills (OCP).
- Age at first child birth.
Decrease risk
- Lactation.
- Body fatness (pre-menopausal).
Insufficient/weak evidence
Increase Risk
- Total dietary fat.
- Greater birth weight (pre-menopausal).
- Tobacco smoking.
- Hormone replacement therapy.
Decrease risk
- Fruits and vegetables.
- Physical activity.
- Consider social determinants of health equity.
- Consider agency.
- I am worried about your breast cancer risk, how do you feel about it?
- What are you already doing to reduce your risk?
What else do you think you could successfully do?
Listen for aligning values, goals, and barriers.
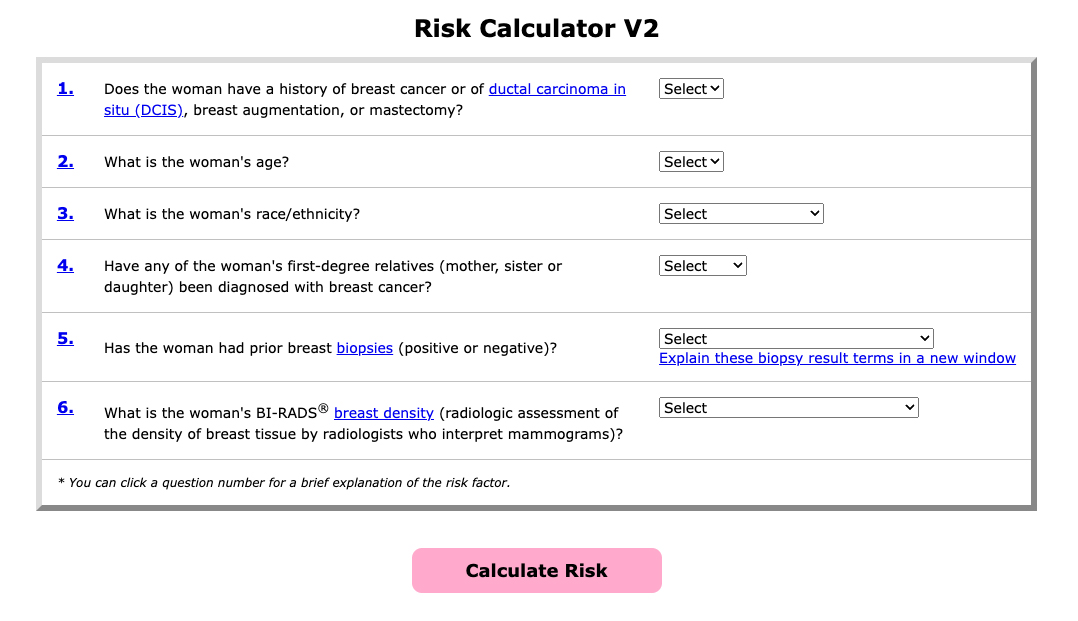
Assessment tools overview
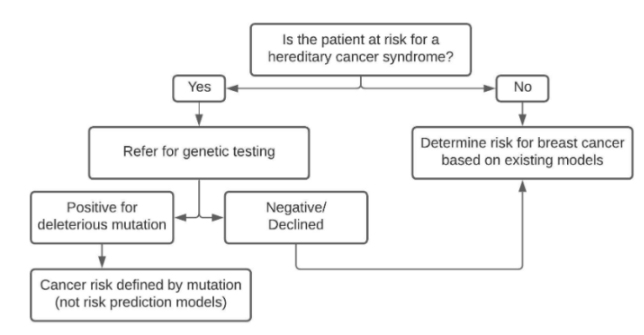
- Use genetic and nongenetic risk factors to calculate risk.
- Not universal for all populations.
- BRCA 1, 2 family hx breast, ovarian CA.
- Populations: Ashkenazi Jew, Black.
- Gail Model 1 (only white women).
- Modified Gail (more inclusive).
- Care Model (black women).
- BCSC (adds density risk).
BRCA 1, 2 Assessment Tools
- 7-Question Family History Screening Tool.
- Ontario Family History Assessment Tool.
- Pedigree Assessment Tool.
- Referral Screening Tool.
- Manchester Scoring System.
- Tyrer-Cuzick (IBIS) model.
- Brief versions of the BRCAPRO model.
Regression model calculators
- Gail Model 1 (only white women).
- Modified Gail (more inclusive).
- Care Model (black women).
- BCSC (adds density risk).
- Personal history.
- Age.
- Ethnicity.
- Family History.
- Biopsy history.
- BI-RADS category (on prior mammogram).
Breast cancer screening
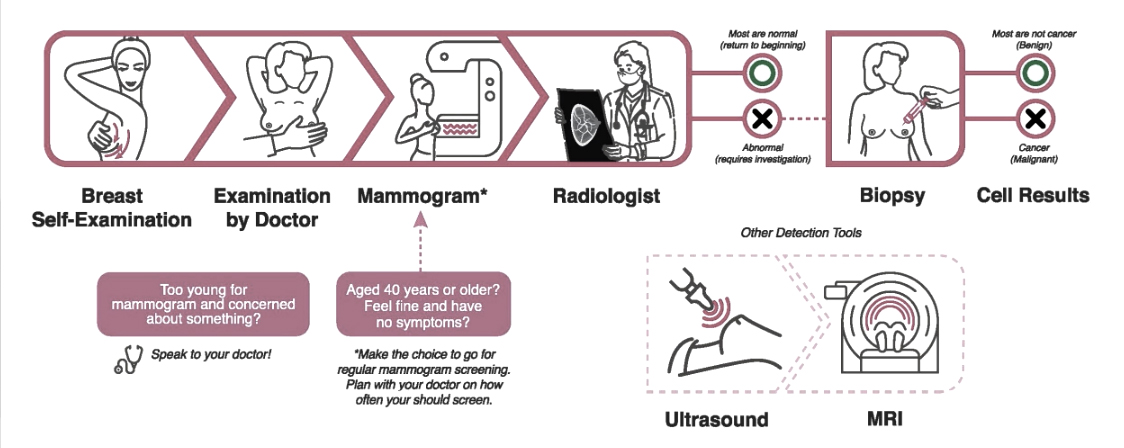
Tools for screening
Breast Self Exam
No evidence that self-exams reduce death from cancer.
Clinical Breast Exam
Contributes little to early detection where mammography screening is available; may increase the rate of false positives.
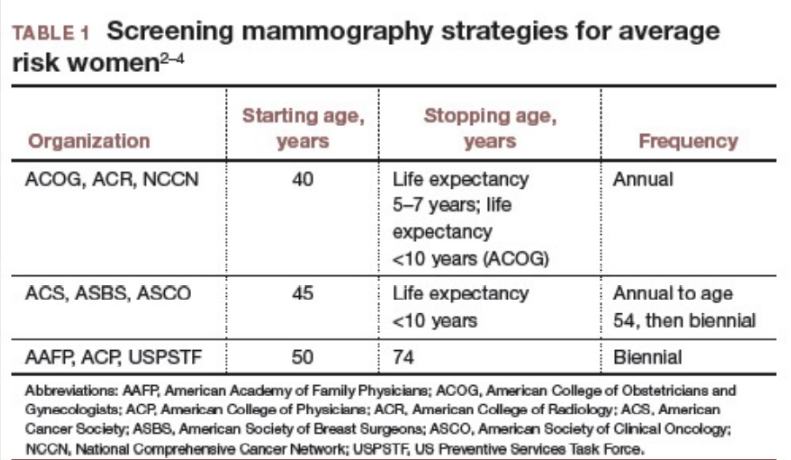
Mammography
Initiates between ages 40 and 50 depending on risk, annual to biannual until 50, annual until 74 or < 10 years of life expected.
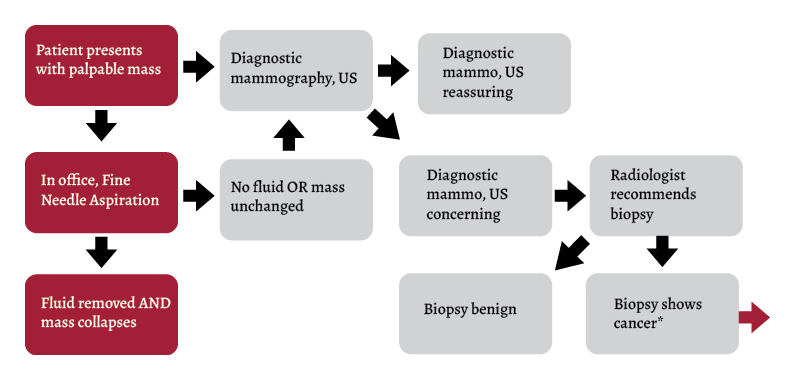
Breast cancer detection

Ultrasound Distinguishes fluid from solid masses.
Diagnostic Mammography
- Thinner slices.
- Higher resolution.
- Adjusted planes.
PET/CT/MRI
Additional imaging at discretion of radiologist, often to improve imaging very dense breasts or for those at high risk.
Biopsy
Histopathology is diagnostic.
- Fine needle aspiration.
- Core biopsy.
- Tumor resection (nodal dissection).
Source: Science Direct.
Breast screening communication
Interprofessional team challenges
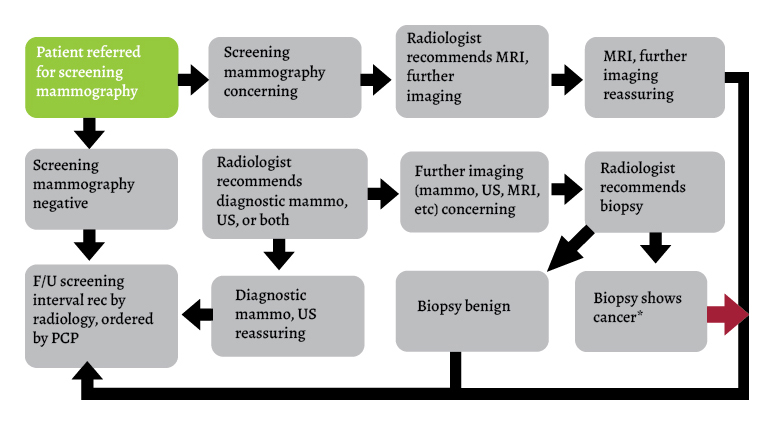
Primary care provider
Radiologist
-
Calculate breast cancer risk.
-
Shared decision with patient on initiating screening.
-
Refer for screening.
-
Communicate normal findings and follow-up intervals.
-
Communicate abnormal findings, answer questions, recommend next steps.
-
Communicate biopsy results, recommend next steps.
-
Refer to surgery, oncology, specialists.
-
Calculate breast cancer risk.
-
Read screening images.
-
Communicate normal findings and follow-up intervals.
-
Communicate abnormal findings, answer questions, recommend next steps.
-
Perform follow-up/additional imaging.
-
Perform biopsy.
-
Communicate biopsy results, recommend next steps.
-
Set screening intervals.
Sam is a 45-year-old who presents to inquire about their breast cancer risk and when to begin mammography. She has no known family history of breast or ovarian cancer. Menarche was at age 13. Her first child was born when she was 27, and she was briefly on hormonal birth control for three years at age 20. She drinks alchohol 2–3 times a week, usually one glass of wine per sitting. She denies radiation exposure. Her BMI is 34.
References
- Geunwon Kim, MD, PhD, manisha Bahl, MD, MPH, Assessing Risk of Breast Cancer: A Review of Risk Prediction Models, Journal of Breast Imaging, Volume 3, Issue 2, March/April 2021, Pages 144–155.
- Breast Cancer in Men. CDC. Accessed November 2023.
- de Blok C J M, Wiepjes C M, Nota N M, van Engelen K, Adank M A, Dreijerink K M A et al. Breast cancer risk in transgender people receiving hormone treatment: nationwide cohort study in the Netherlands. BMJ 2019; 365 :l1652 doi:10.1136/bmj.l1652.
- What Are the Risk Factors for Breast Cancer? CDC. Accessed November 2023.