- Suggested reading
- Reading guide
- Need to Know
There is one chapter for suggested reading from Lippincott, Chapter 21: Amino Acids: Conversion to Specialized Products. This chapter will become very relevant in FMS 502 during Heme. However, it fits in nicely here since we are discussing the biochemistry of nitrogen metabolism. The short descriptions listed below are some of the big-picture, high-yield points. The reading and the class session will go into more depth and detail. The reading guides are also posted.
As I have said in other modules, this reading guide is for people who need help focusing on these chapters. Most students DO NOT need to use the guide.
Read Chapter 21.
Porphyrins and the metabolism of heme
-
Big picture
-
What are porphyrins, and what is the prevalent one in humans?
-
What is heme?
-
Heme is found in which proteins?
-
How much heme is turned over (synthesized and broken down) each day?
-
What are the main sites of heme synthesis?
-
-
Structure of porphyrins (Fig. 21.4, 21.5)
-
What is the basic structure of a porphyrin?
-
There are four types of porphyrins (I-IV). Which kind is important in humans?
-
-
Biosynthesis of heme
-
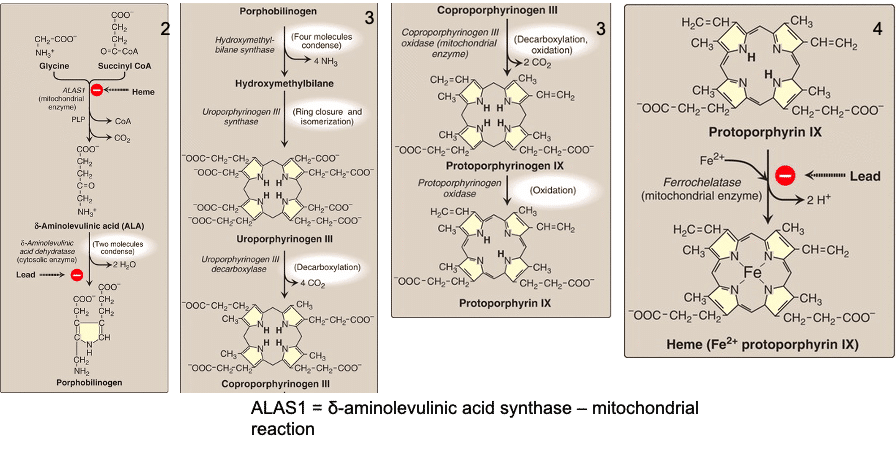
If you can pencil out the basic pathway to the formation of heme, you will be able to easily answer the following questions. It will also help you to organize the various porphyrias and their causes. (Fig. 21.8 is a very nice summary of this pathway.) I find this helpful for getting the flow of protoporphyrin IX (heme) synthesis (included in the slides for this topic).
-
What are the two initial building blocks (the starting material) of protoporphyrin IX and heme, and what do they combine to form?
-
What is the immediate precursor to porphobilinogen, the primary subunit of the heme structure?
-
What color is uroporphyrinogen?
-
What is the rate controlling step in porphyrin synthesis and what is the primary regulator?
-
Note that many drugs are metabolized by the cytochrome P450 monooxygenase system and consequently up-regulate the synthesis of these heme-containing proteins. This increase consumes available heme, decreasing end-product inhibition, and in turn up-regulates ALA synthase activity.
-
-
Porphyrias and other problems associated with heme biosynthesis
-
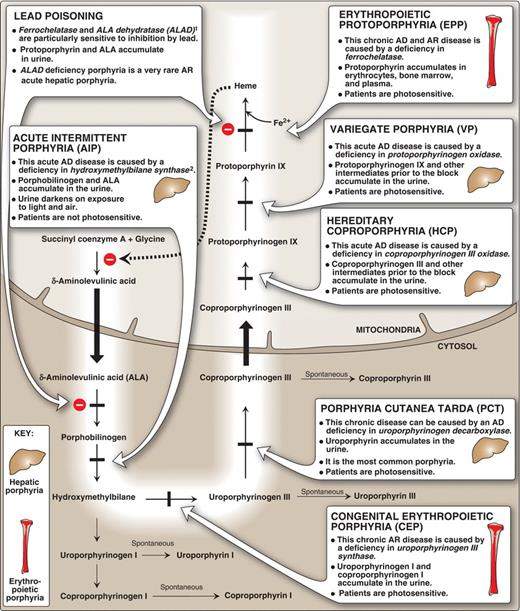
The porphyrias are defects in heme biosynthesis. Many are inherited and all are rare. If untreated, they result in accumulation of porphyrin intermediates to toxic levels. There is a porphyria associated with an enzyme deficiency at every step of porphyrin synthesis downstream of porphobilinogen (Fig. 21.8).
-
Porphyria cutanea tarda is the most common porphyria. Remember this one.
-
The other hepatic porphyrias are all acute and occur in alphabetical order; acute intermittent porphyria – hereditary coproporphyria—variegate porphyria. These porphyrias tend to produce neurologic, gastrointestinal, and cardiovascular symptoms.
-
The two erythropoietic porphyrias are also in alphabetical order and both have erythropoietic in the name; congenital erythropoietic porphyria and erythropoietic protoporphyria. These are characterized by skin rashes and are sometimes referred to as cutaneous porphyrias.
-
The porphyrias that produce accumulation of tetrapyrrole rings cause photosensitivity (which is all of them except acute intermittent porphyria). Why do you suppose that is?
-
-
All the porphyrias are inherited as autosomal dominant except congenital erythropoietic porphyria (the first erythropoietic one). This one is recessive and the rarest porphyria.
-
-
To summarize
-
Hepatic, acute = non-cutaneous presentation (neurologic, gastrointestinal, and cardiovascular)
-
Hepatic, chronic = most common, cutaneous symptoms later in life
-
Erythropoietic = cutaneous symptoms in early childhood
-
If you’ve committed the heme biosynthetic pathway to memory (at least for the moment), you’ll be able to place these porphyrias on the synthetic pathway and to predict some of the precursor accumulations and symptoms. Don’t forget the steps of heme synthesis that are inhibited by lead. Not really a porphyria but a complication of lead poisoning.
-
All the porphyrias result in decreased heme synthesis and consequently an activation (derepression) of ALA synthase. Given this fact, how would you treat a porphyria?
-
-
Degradation of heme
-
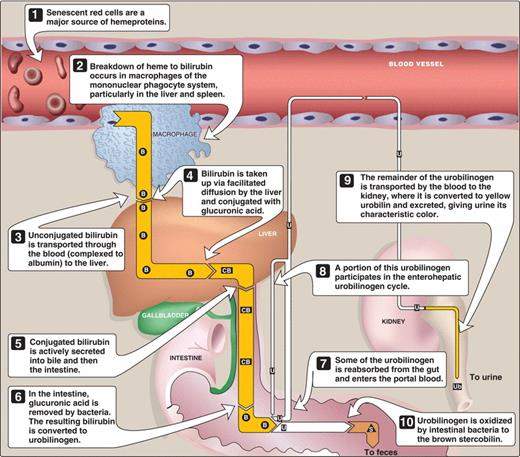
How long does a red blood cell routinely last in circulation before being turned over?
-
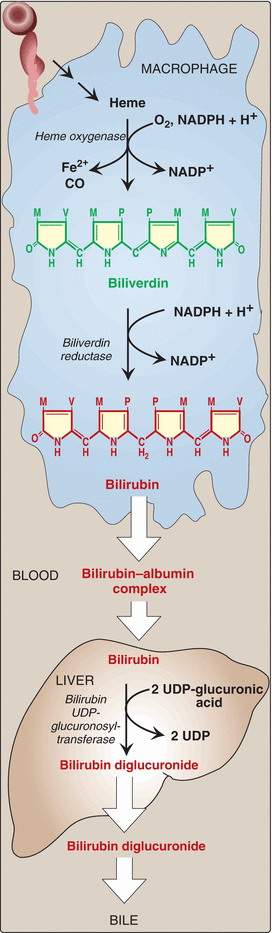
The degradation of heme and its transport to the liver is straight forward. If you know the major steps you will be able to answer the following questions. (Fig. 21.9, 21.10)
-
How is biliverdin formed from heme?
-
How is bilirubin produced from biliverdin?
-
How do you tell biliverdin from bilirubin?
-
How is bilirubin transported to the liver?
-
What happens to bilirubin once in the liver?
-
What happens to conjugated bilirubin in the gut?
-
What makes feces brown?
-
What happens to urobilinogen that gets taken back up into the blood stream?
-
-
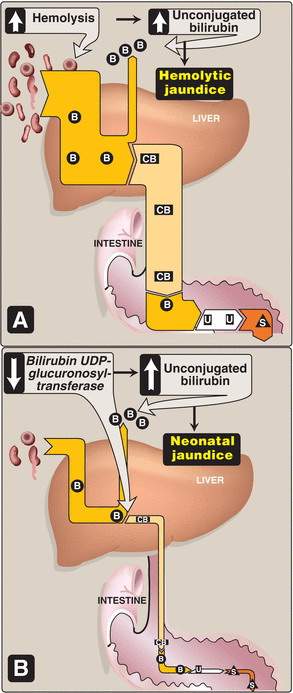
Jaundice (Fig. 21.12, 21.13)
-
What is jaundice?
-
Describe the 3 main types of jaundice.
-
Which basic type of jaundice does the jaundice that occurs in newborns resemble?
-
Why do you need to extract blood with methanol to measure all the bilirubin?
-
Other nitrogen containing derivatives of amino acids
-
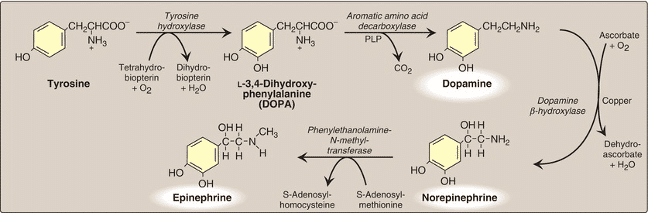
Catecholamines (Fig. 21.5)
-
What are the primary three catecholamines and from what amino acid are they derived?
-
Which of these catecholamines is produced only outside the nervous system?
-
How are catecholamines inactivated? (Fig. 21.6)
-
-
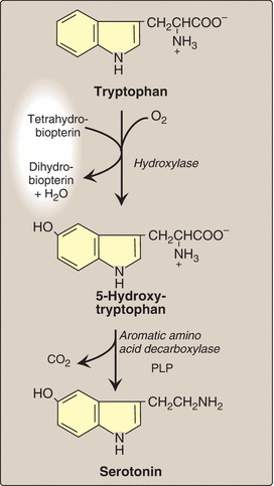
Serotonin (Fig. 21.18)
-
How is serotonin synthesized?
-
How is serotonin degraded?
-
-
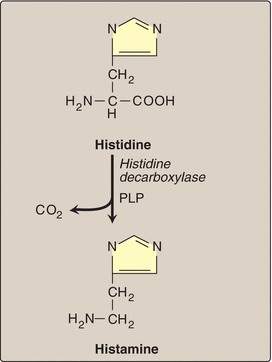
Histamine (Fig. 21.17)
-
How is histamine synthesized?
-
-
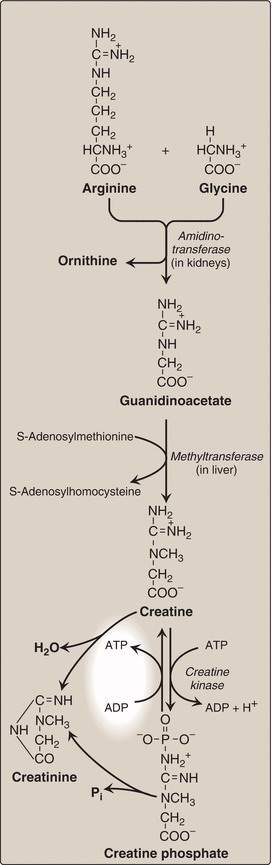
Creatine (Fig. 21.19)
-
What does creatine do?
-
Why is creatine clinically important and useful?
-
How is creatine synthesized?
-
Diagram and describe the synthesis of heme and other porphyrins, and explain the molecular basis of disorders resulting from defects in this pathway
-
δ-aminolevulinic acid synthase (ALAS1)
-
δ-aminolevulinic acid dehydratase
-
Ferrochelatase
-
Porphyrin synthesis (general, not the specifics, i.e. where and how)
Describe disorders of heme biosynthesis at the molecular level
-
Porphyrias (Porphyria cutena tarda and acute intermittent porphyria)
-
Lead poisoning
Diagram and describe the metabolism of bilirubin and the disorders related to bilirubin metabolism
-
Glucuronosyltransferase (bilirubin UGT)
-
Jaundice (three types that were discussed)
-
Bilirubin metabolism
Describe the pathways by which catecholamines, histamine, serotonin, and creatine are synthesized and degraded
-
Catecholamine metabolism
-
Serotonin metabolism
-
Histamine synthesis
-
Creatine synthesis
-
Porphyrin breakdown
Diagram and describe the synthesis of heme and other porphyrins, and explain the molecular basis of disorders resulting from defects in this pathway
Describe disorders of heme biosynthesis at the molecular level
Two of the more high-yield porphyrias to remember are acute intermediate porphyria and porphyria cutena tarda.
Diagram and describe the metabolism of bilirubin and the disorders related to bilirubin metabolism
This is another very high-yield concept to know and understand. Bilirubin metabolism is the process by which heme is broken down.
Diagram and describe the metabolism of bilirubin and the disorders related to bilirubin metabolism
Jaundice refers to the yellow color of skin, nail beds, and sclerae caused by bilirubin deposition, secondary to increased bilirubin levels in the blood (hyperbilirubinemia). Although not a disease, jaundice is usually a symptom of an underlying disorder. Osmosis does have a few videos on jaundice. Not all of them are appropriate at this time in your journey through medical school (although they are interesting!). You will hear about jaundice over the next few years.
I’d like you to be familiar with three types of jaundice.