Bacterial classification (Phenotypic)
-
Gram Stain: Differentiates based on cell wall structure.
-
Morphology: Cocci, bacilli, curved rods, clusters, chains.
-
Growth Requirements: Oxygen tolerance (aerobes vs anaerobes).
-
Biochemical Reactions: Catalase, coagulase, oxidase, lactose fermentation.
-
Serologic Systems: Group A vs B Strep (based on surface antigens).
Gram stain mechanism
-
Crystal Violet → binds peptidoglycan.
-
Iodine → forms CV-I complex.
-
Alcohol → decolorizes Gram-negatives.
-
Safranin → counterstains Gram-negatives pink.
-
Gram-Positive: Thick peptidoglycan, teichoic acids, no outer membrane → purple.
-
Gram-Negative: Thin peptidoglycan, outer membrane with LPS → pink.
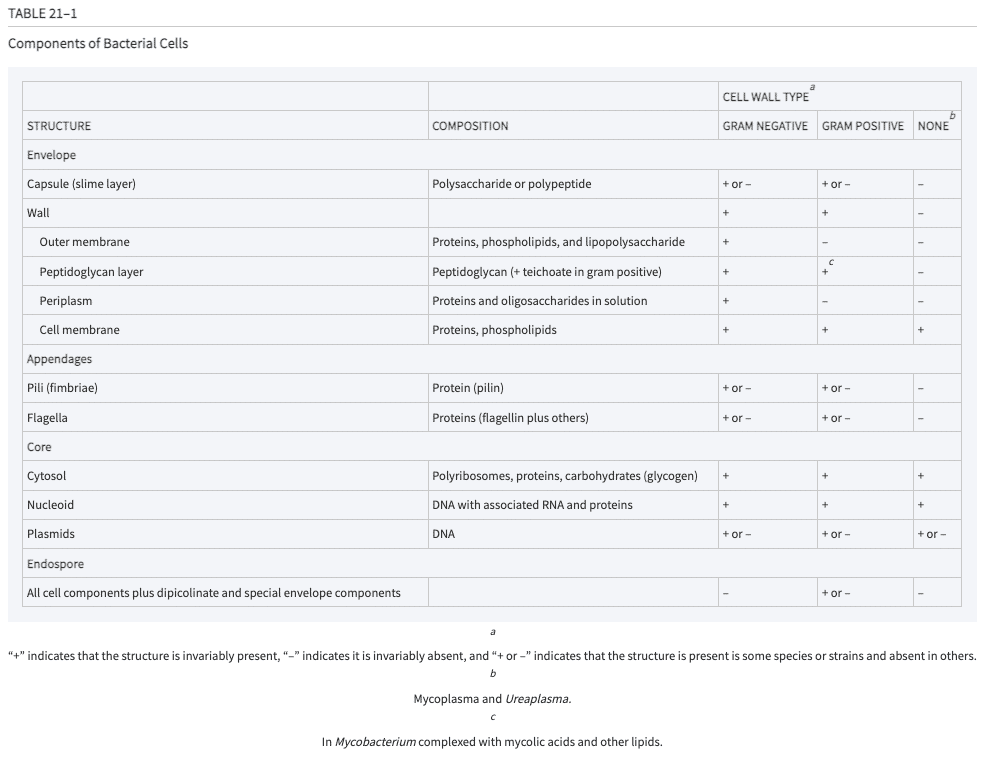
Bacterial cell structure
-
All bacteria/Prokaryotes: No nucleus, no membrane-bound organelles, single circular chromosome, 70S ribosomes, replication via binary fission.
-
All bacteria have a cell wall with peptidoglycan (Mycoplasma is an exception). Structural integrity is provided by peptide cross-linking by transpeptidase (PBP): Target of β-lactams.
-
Additional structural features (some bacteria).
-
Capsule: Polysaccharide; anti-phagocytic (e.g., S. pneumoniae, H. influenzae).
-
Appendages: Pili (adhesion, conjugation), Flagella (motility).
-
Spores: Dormant, resistant forms (e.g., Clostridium, Bacillus).
-
Gram-positive cell wall
-
Thick peptidoglycan layer confers the purple color on gram stain.
-
Teichoic and lipoteichoic acids are G+ specific structural features that are recognized by immune system (pathogen associated molecular pattern, PAMP).
Gram-negative cell wall
-
Thin peptidoglycan layer leads to the pink color on gram stain.
-
Outer membrane with LPS (endotoxin): Lipid A (toxic), O-antigen (serotyping).
-
Porins: Selective permeability.
-
Protein secretion systems: Types I–VI (Type III = injectosome).
Atypical cell walls
-
Mycobacteria: Mycolic acids, acid-fast stain (Ziehl-Neelsen), slow-growing.
-
Mycoplasma/Chlamydia: No peptidoglycan → not visible on Gram stain.
Spores
-
Metabolically inactive, highly resistant.
-
Spore coat: Keratin-like.
-
Examples: Clostridium, Bacillus.
-
Not killed by antibiotics (non-replicating).
Metabolism and growth
-
Obligate aerobes: Only aerobic respiration, no fermentation. (e.g. TB, Pseudomonas.
-
Obligate anaerobes: No aerobic respiration, no catalase or SOD = oxygen is poison (e.g., Clostridium, Bacteroides.)
-
Facultative anaerobes: Can metabolize energy aerobically or anaerobically and small amounts of catalase and SOD protect from ROS (e.g., E. coli, S. aureus).
-
Microaerophilic: Need oxygen for aerobic respiration, but small amounts of catalase and SOD mean they are poisoned by high O2 (e.g., Helicobacter pylori).
Biochemical tests used in differentiation of organisms
-
Catalase: H₂O₂ → H₂O + O₂ (Staph +, Strep –).
-
Coagulase: Fibrinogen → fibrin (S. aureus +).
-
Lactose fermentation: MacConkey agar (E. coli +).
-
Oxidase: Cytochrome c oxidase (Pseudomonas +).
Board tips and mnemonics
-
No Cell Wall = No Gram Stain → Mycoplasma, Chlamydia.
-
Spores = Survival → Think Clostridium difficile in hospitals.
-
Positive = Purple → Gram-positive retains crystal violet.
-
Lipid A = Lethal A → Endotoxin effects: fever, shock, DIC.
Infection process overview
-
Steps in Infection:
Attach → Persist → Invade → Adapt → Replicate → Exit/Spread
-
Virulence: Ability to cause disease; not all colonizing bacteria cause infection.
-
Host Factors: Skin integrity, immune status, social determinants, environment.
Attachment and persistence
-
Adhesins (bacterial) bind receptors (host).
-
Pili often enhance adhesion.
-
Site-specific colonization: e.g., Strep pyogenes → pharyngitis.
-
Biofilms:
-
Aggregates of bacteria in a matrix.
-
Resist immune clearance and antibiotics.
-
Common in prosthetics, CF lungs, ischemic wounds.
-
-
Mechanisms used.
-
Nutrient acquisition:
-
Siderophores: High-affinity iron chelators.
-
Nutritional Immunity: Host sequesters nutrients (e.g., iron via transferrin/lactoferrin).
-
Bacteria evolve mechanisms to extract metals, amino acids, sugars, vitamins.
-
-
Intracellular survival or transition
-
Example: Listeria monocytogenes uses actin polymerization to move between cells.
-
Virulence factors: Toxins
- Endotoxins (LPS)
-
Found in Gram-negative outer membrane.
-
Lipid A activates TLR4 → cytokine storm (TNF, IL-1).
-
Causes fever, shock, complement activation.
-
- Exotoxins (Secreted Proteins)
- Mechanisms:
-
-
-
Membrane damage (pore-forming):
-
S. aureus α-toxin.
-
Strep pyogenes: Streptolysin O.
-
C. perfringens- phospholipase.
-
-
Immune Activation:
-
Superantigens (e.g., TSS toxins) → massive cytokine release.
-
-
Neurotoxins:
-
Prevention of release of neurotransmitters at neuromuscular junction = contraction or paralysis depending on which cell is targeted.
-
-
Cellular Signaling Interference:
-
ADP-ribosylation (e.g., Cholera, Pertussis, C. difficile).
-
-
Protein Synthesis Inhibition:
-
Inhibition of Elongation Factor 2 (EF2).
-
Diphtheria toxin, Shiga toxin.
-
-
Extracellular Matrix Damage:
-
Collagenase, hyaluronidase = tissue damage.
-
IgA protease = immune evasion(e.g., Neisseri, Strep pneumo).
-
-
-
Genetic adaptability and resistance
- Horizontal Gene Transfer
-
Transformation: Uptake of naked DNA.
-
Conjugation: Plasmid transfer via sex pilus.
-
Transduction: Phage-mediated DNA transfer.
-
Transposition: Mobile genetic elements (“jumping genes”).
-
- Specialized Transduction
- Example: Corynebacterium diphtheriae acquires toxin gene via β-phage.
Board tips and mnemonics
-
Biofilms = Bacterial bunkers → immune evasion + antibiotic resistance.
-
Superantigens = Cytokine storm → shock.
-
ADP-ribosylation = Signal hijack.
-
Horizontal gene transfer = Resistance spread.
Learning goals
Introduction to bacteria: Classification and structure
- Demonstrate the different ways of cataloguing bacteria by shape, staining characteristics, and metabolic strategies
- Describe the content, structure, and function of key bacterial features: capsule, cell wall, cell membrane, spores, and appendages
- Compare and contrast the components and structure of gram-negative and gram-positive cell walls
Introduction to bacteria: Virulence and pathogenicity
- Describe different strategies used by bacteria for invasion and persistence, including evasion of host immunity, extraction of key nutrients for metabolic needs, and intracellular survival
- Explain how toxins work as virulence factors in bacterial infections and describe the six most common mechanisms of bacterial toxins
- Explain four mechanisms of genetic transfer among bacteria as it relates to virulence and antimicrobial resistance
Required pre-class preparation
-
Robert Wood Johnson Microbiology, Immunology, and Infectious Diseases
Introduction to Microbiology: Evolve Bacteria
Study materials
These materials are not required; they are supplementary to large group session. They are intended as a curated guide to content focused on the learning objectives. There are both textbook and video resources for this session for students to use per their preference. For each reference, I have designated in superscript the learning objective addressed.
Click the book icons below to go to the library resources listed.
-
Sherris Medical Microbiology, 8e
Chapter 21: Bacteria—Basic Concepts
1 2 Section on Bacteria Structure
6 Section on Bacterial Genetics, focus on Genetic exchange
3 Table 21-1: Components of Bacterial Cells: Table summarizing bacterial structural elements, composition, and whether they are found in gram-, gram+, or non-gram-stainable bacteria
-
Sherris Medical Microbiology, 8e
Chapter 22: Bacteria—Pathogenesis of Bacterial Infection
4 5 Section on Attributes of bacterial pathogenicity -
Levinson's Review of Medical Microbiology & Immunology: A Guide to Clinical Infectious Diseases, 17e
6 Chapter 4: Genetics
This textbook tends to present more ‘bite-sized’ amounts of information and more often in bulleted format that some students might find more accessible compared with Sherris. Equally accurate resources.