check yourself
Fill in these summary tables to check your learning.
Amoeba
About the size of WBCs, but move by pseudopodia.
Entamoeba histolytica (amebiasis)
Obligate human parasite that are transmitted to humans by ingestion of the cysts shed in asymptomatic carriers’ stool.
Cysts form trophozoites in intestine where they can eat RBCs and invade the colonic mucosa. Clinical disease includes acute dysenteric colitis (fever, blood and mucous in stool) and later liver abscess (hole in liver). Anal and penile disease have been described in MSM patients.
- Dx: Stool wet mount/O&P, or stool or serum E. histolytica Ag test (depending on stage GI or extraintestinal disease).
- Rx: Metronidazole (or tinidazole), etc.
See also in the Micro-ID session guide
Entamoeba coli
One of many non-pathogenic amoeba and may be confused with E. histolytica on wet mount.
Acanthamoeba
Found in freshwater lakes and soil.
Keratitis in contact lens wearers. Also can cause amebic meningoencephalitis which is associated with devastating morbidity/mortality.
Naegleria
Free-living amoeba in pools and freshwater lakes and soil.
Causes acute and usually fatal meningoencephalitis.
Flagellates
Motile.
GI/Vaginal
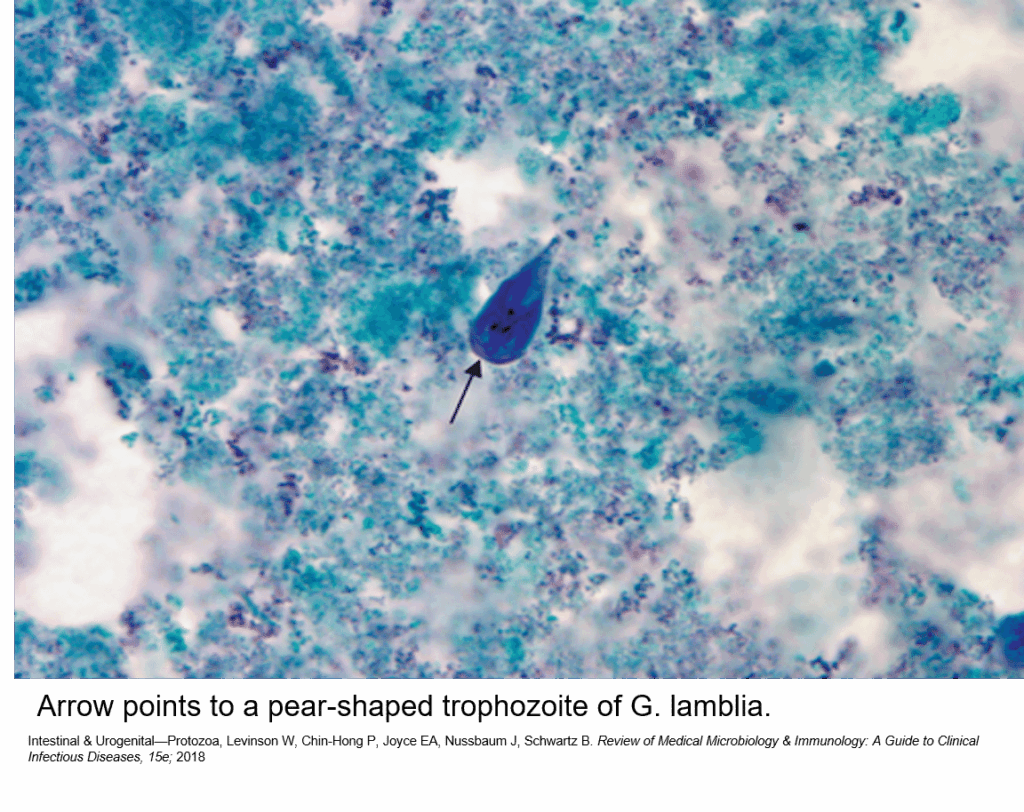
Giardia
Intestinal pear-shaped flagellated protozoan.
Occurs worldwide in humans and animal hosts. Fecal oral spread when cysts are ingested in contaminated water. Organism is harbored by many rodents and beaver, so campers drinking stream water are at special risk. Clinical disease is characterized by watery diarrhea, with bloating and foul smell (malabsorption), without fever. Increased risk in IgA deficiency.
- Dx: Giardia antigen or cysts in stool.
- Prevention:
- Rx: Metronidazole or tinidazole.
See also in the Micro-ID session guide
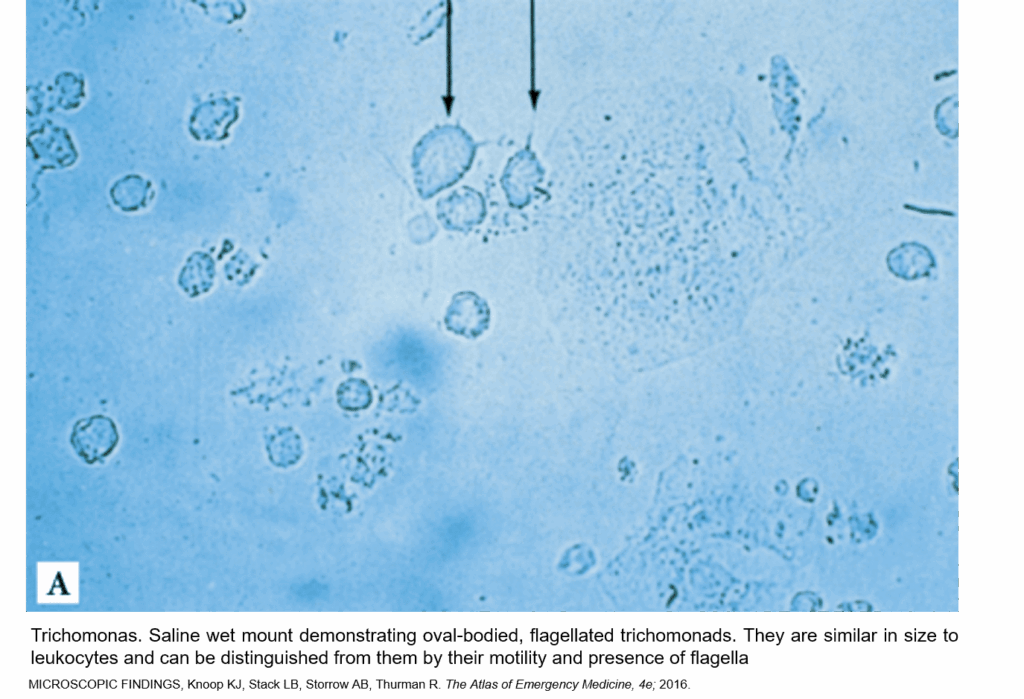
Trichomonas
Urogenital pear-shaped flagellated protozoan.
Trophozoites attach to mucosa of female genital tract and cause inflammation. Clinical disease characterized by homogeneous watery discharge and strawberry cervix. Urethritis in men is usually asymptomatic. Sexual transmission.
- Dx: High vaginal pH=5–6 (normal vaginal pH=3.8–4.5) and highly motile cells about the size of WBCs but with flagellum on wet mount.
- Rx Metronidazole (or tinidazole).
Blood and tissue
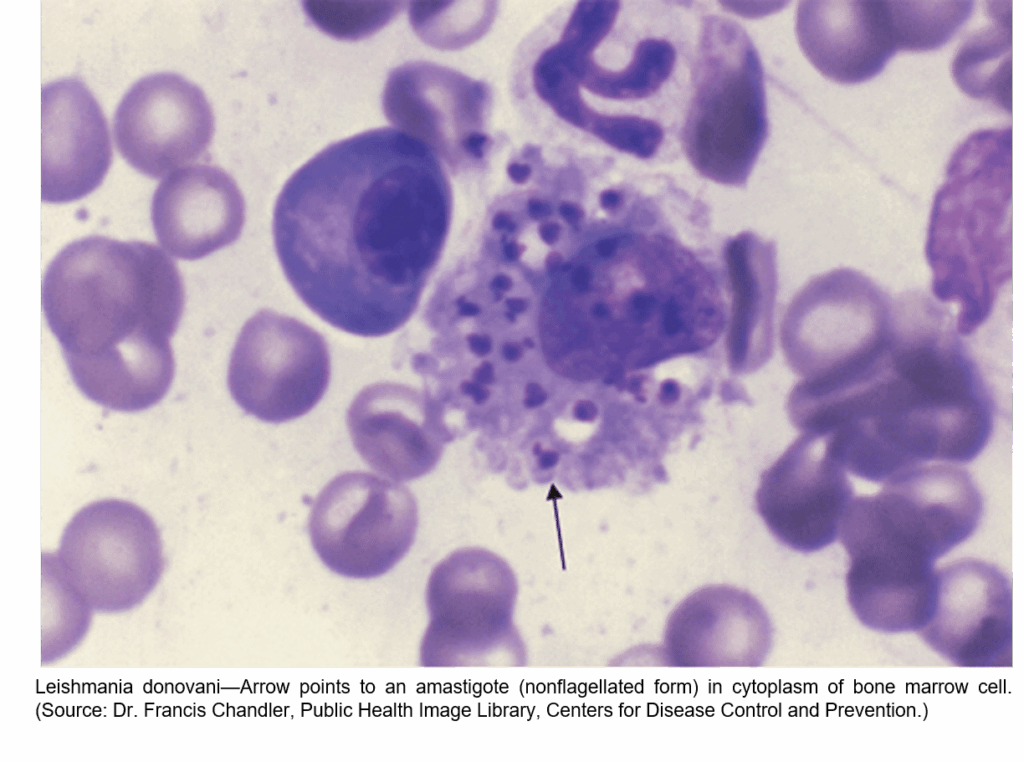
Leishmaniasis
Blood and tissue protozoan.
Transmitted by phlebotomine sandfly bite. After bite, promastigotes enter blood macrophages and form amastigotes that infect other cells within reticuloendothelial system. Association with travel to many tropical countries and the Middle East but found widely.
Leishmania braziliensis, etc.
Nonhealing nodules and skin ulcers after travel. Diagnosis is based on seeing amastigotes in macrophages from skin smear at edge of lesion.
Treatment: Sodium stibogluconate.
Usually L. donovani.
Fever, weight loss, hepatosplenomegaly and pancytopenia. Spleen aspirate shows macrophages filled with organisms (reproducing intracellularly).
Other forms like diffuse cutaneous leishmaniasis (less common).
Treatment: Pentavalent antimony, Amphotericin B
See also in the Micro-ID session guide
Trypanosomiasis
African sleeping sickness is blood and tissue protozoan with East African and West African form.
Transmission is from bite of Tsetse fly, when trypomastigotes enter blood stream. Repeated variation of surface antigens (like borrelia) allow immune evasion. Clinical disease is characterized first by painful chancre at bite site, then enlarged nodes. Progression to encephalitis and coma is part of late manifestations and is 100% fatal.
Dx by finding flagellated protozoa in blood smear (NOT inside RBCs like malaria and Babesia, but in serum like Borrelia)
Rx: Pentamidine, suramin, eflornithine, nifurtimox.
Blood and tissue protozoan that is transmitted by the bite of reduviid/triatome bug Geographically more prevalent in central and south America. Insects feed at night and the face/eyes are common available locations. Localized inflammation occurs (Romaña’s sign on the eye). Transmission by reduviid bug (triatomine/kissing bug) bites at night causing swollen lesion especially around eye (Romaña’s sign). Acute infection may be asymptomatic. Chronic infection leads to late manifestations: megacolon, megaesophagus, and megacardia (megacardia is not a real clinical term, but useful here to describe cardiomyopathy/CHF/arrhythmia).
Dx with serology in appropriate clinical setting. Flagellated protozoa in blood smear (similar to other trypanosomes but somewhat more C-shaped) are rare and hard to find. Classical xenodiagnosis by infecting reduviid bugs after biting patient with suspected Chagas.
Rx: Nifurtimox, Benznidazole. Late manifestations are often irreversible.
Ciliates
Few of medical significance to humans.
Balantidium coli
Colitis and watery diarrhea, especially in AIDS patients.
Sporozoa
Non-motile protozoa.
GI
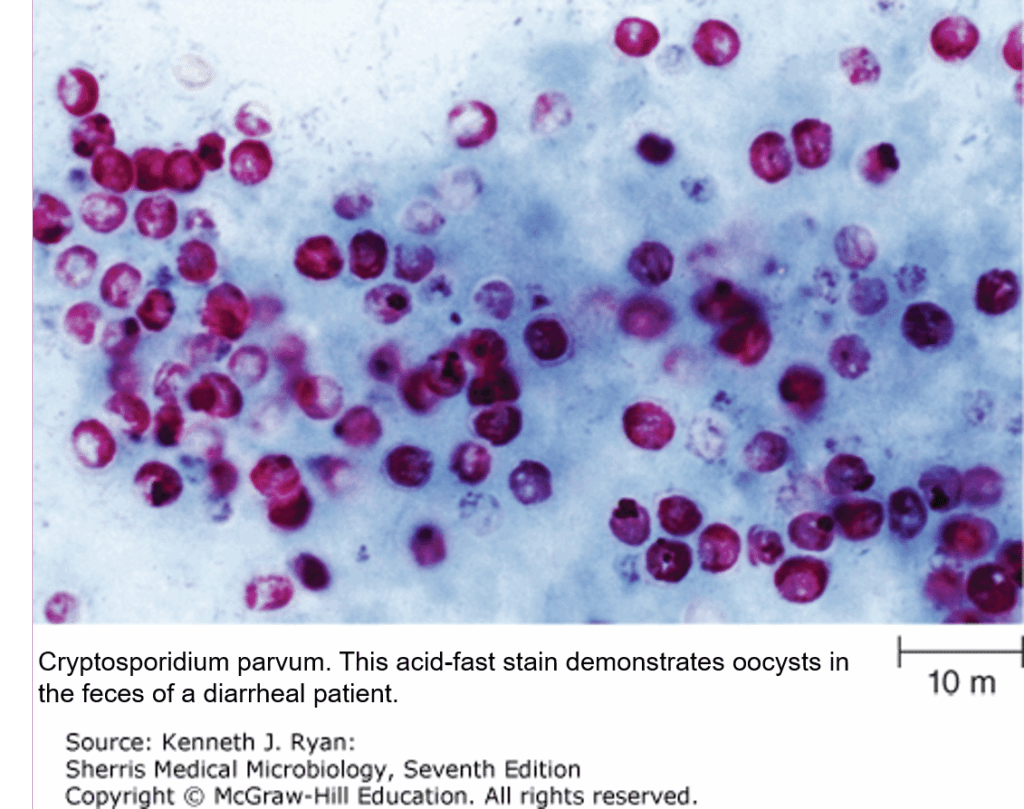
Cryptosporidium
Obligate intracellular parasite of intestinal epithelial cells.
Causes watery diarrhea, worse in AIDS patients where it can cause chronic wasting and malnutrition. Fecal oral spread (person to person or animal to person) especially from public swimming areas.
- Dx: Not seen on regular O&P study, but stains with modified acid-fast stain.
- Tx: Supportive, immune reconstitution, paromomycin
See also in the Micro-ID session guide
Blood and tissue
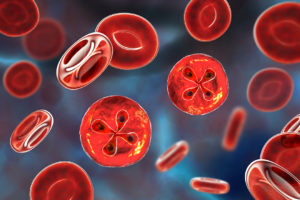
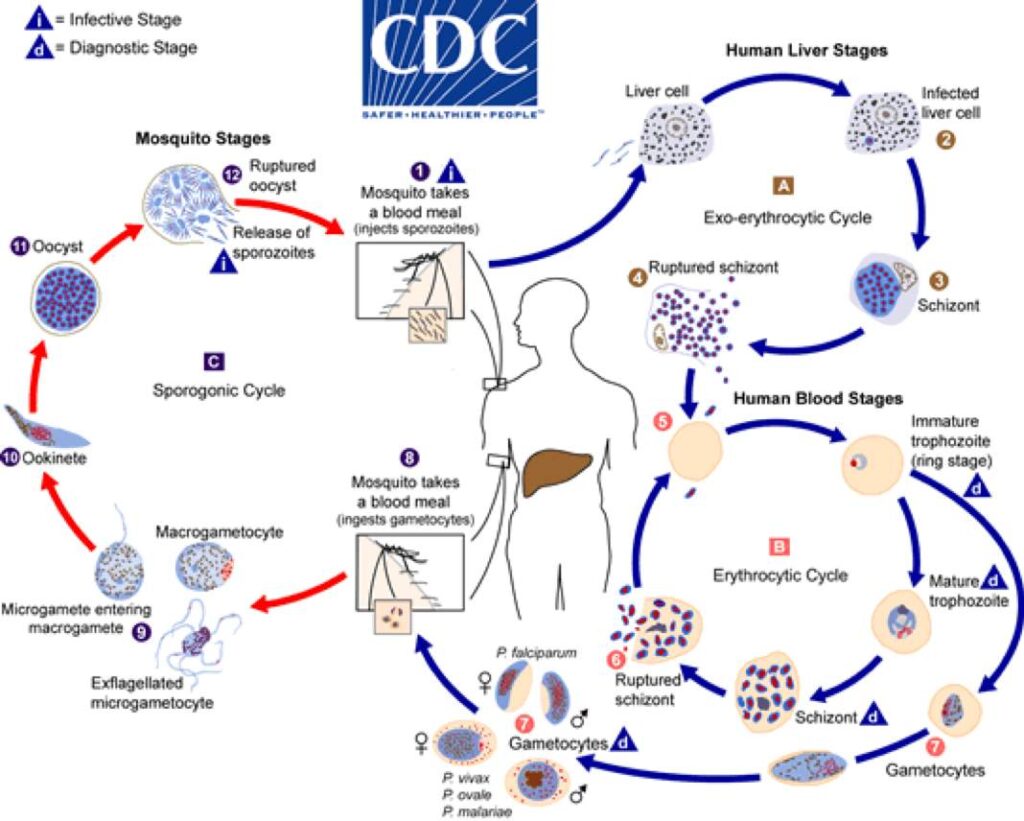
Malaria/Plasmodium
One of the major causes of mortality due to infectious diseases worldwide.
Transmitted by female anopheles mosquitoes (or blood transfusion). There is geographic distribution of species types and geographic variation in pharmacologic susceptibilities. In United States, persons who travel to visit friends and family are highest risk group. Clinical disease is typically manifested by high fever usually related to international travel. Paroxysmal episodes of fevers are classically described and represent the blood phase of parasitic replication. In ‘real world’ paroxysms are not always well defined. Complications of malaria occur from species that have chronic/latent forms and from P. falciparum which has potential to cause severe multisystem.
- Diagnosis is made on thick and thin smears where parasite morphology and quantity can be distinguished. Molecular and rapid tests are of increasing importance in regions with limited resources and/or limited experience (i.e., United States).
Causes most fatal cases, cerebral malaria; parasites inside RBCs cause hemolysis.
Banana gametocytes. Increased resistance to chloroquine and other antiparasitic drugs except in Central America and Caribbean areas (such as Haiti). No hepatic latent stage, so no relapsing form.
Prevention with atovaquone-proguanil (expensive), mefloquine (side effects psychiatric and cardiac), or doxycycline.
Therapy with artemether combination drugs (e.g., artemether-lumefantrine), especially for severe malaria. Other options atovaquone-proguanil, quinine, mefloquine. Chloroquine rarely appropriate.
Relapsing forms due to hypnozoites in the liver.
P. vivax infects younger RBCs (larger size). P. ovale is only in West Africa.
Erythrocyte stage is usually sensitive to chloroquine, but liver stage for these two species requires primaquine Rx after treatment of the erythrocytic stage. Check for G6PD deficiency, especially before using primaquine.
Infects older RBCs (smaller size).
Malaria variant seen in South Pacific region (from monkeys).
check yourself
Fill in this summary table to check your learning.
See also in the Micro-ID session guide
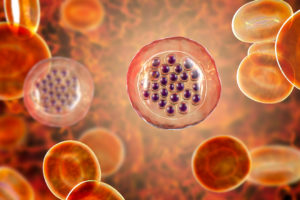
Babesiosis
Looks like malaria with trophozoites in RBCS, but transmitted by ticks and regional disease (esp. N.E. USA, Minnesota, Wisconsin). “Maltese cross” in RBCs.
See also in the Micro-ID session guide
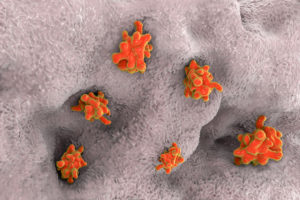
Toxoplasmosis
Transmitted by cysts from cat feces and poorly cooked meat.
Primary infection in a pregnant woman is a major risk for the fetus (congenital toxoplasmosis), causing mental retardation, chorioretinitis, and other birth defects. In normal host, it causes fever and mononucleosis-like syndrome, adenopathy, hepatosplenomegaly. Retinitis (blindness that can flair in second and third decade or in immune suppressed). Toxoplasmosis is a common cause of encephalitis with brain cysts especially in AIDS patients. Presents as confusion or seizures, and CT/MRI show ring-shaped brain lesions that enhance with contrast.
- Dx: Serology helpful in dx.
- Bx: Shows crescent-shaped trophozoites in macrophages.
- Rx: Sulfadiazine/pyrimethamine.
See also in the Micro-ID session guide
Pneumocystitis
P. jirovecii (previously P. carinii) now classified as fungus (previously protozoan).
Classic cause of pneumonia (PCP) in opportunistic host, especially AIDS patients. Presents with fever, SOB, and severe hypoxia. No person-to-person transmission. Early in clinical course may have minimal infiltrates on CXR.
- Dx: Biopsy of lung tissue or occasionally sputum may show the oval shaped organism seen with silver stain or immunofluorescent stain.
- Rx: Trimethoprim-sulfamethoxazole or pentamidine. Give prophylaxis for AIDS patients with CD4<200.

See also in the Micro-ID compendium