Tap the arrow to view the case.
Ms. Xiu, a 37-year-old nurse from Walla Walla, lives in Tanzania, where she works as a manager and volunteer coordinator for a pediatric health non-governmental organization (NGO). During her recent fundraising trip to Washington state, she developed a low-grade fever that she dismissed initially. Then she developed dull upper-right quadrant pain. At this point, she presents to her primary care clinic.
During her evaluation, she reports that the pain is relatively constant, and not associated with food intake. Her medical history is relatively unremarkable. She notes that she is very cautious about mosquito avoidance and hasn’t yet had any vector-borne illnesses. She did have an episode of diarrhea several months ago. She notes that it was worse than typical traveler’s diarrhea, with more mucous. But by the time she made arrangements to get to a medical center in Tanzania, the symptoms had improved.
Questions for consideration
Think about these questions as you watch the video and review the pre-class material.
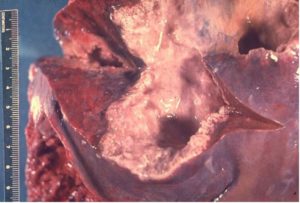
- What are the liver findings, and what is contained in the abnormality (i.e., what might you find on aspirate)?
- What is the likely pathogen?
- How did she acquire this pathogen?
- What relation, if any, does this presentation have to the prior episode of diarrhea?
- How does the approach to making a diagnosis now differ from making a diagnosis earlier?
Acute GI: Protozoa
Watch these two videos.
Amebiasis: Entamoeba histolytica
- Epidemiology
- Clinical
- Life Cycle
- Diagnosis
- Treatment
- Fecal-oral spread of cysts.
- Resource-limited areas (i.e., Mexico, Africa, India, Central and South America).
- Male-male sex (Japan, Taiwan).
- Bloody or mucous diarrhea.
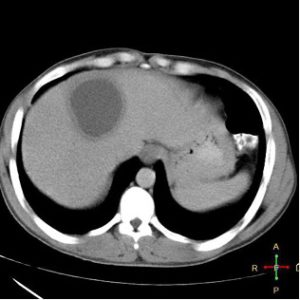
- Liver abscess in some cases.


- Cysts are the infectious form.
- Note: Various non-pathogenic mimics: E. dispar, E. coli.
- Dysentery:
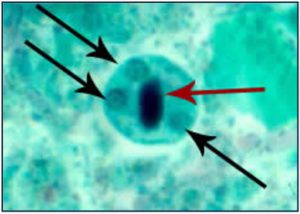
- O&P (trophozoites with ingested RBCs).
- Stool Ag.
- PCR.
- Colonoscopy.

- Liver abscess: Ultrasound or CT imaging plus serology (99% sensitive).
Metronidazole followed by paromomycin (or other GI intraluminal agent).
Test your knowledge
Anchovy paste—acellular proteinacous debris and brown-like fluid. Organisms are rarely seen but, when present, are trophozoites at edges of the abscess, invading nearby tissues.
Entamoeba histolytica.
Transmission is fecal-oral.
The prior episode of diarrhea was likely acute amebic dysentery, when she was first infected. Trophozoites travel across the lumen of the gut and through the bloodstream to portal blood supply where the liver abscess forms.
- Diagnosis during the acute diarrheal stage is made by visualization of the organism on Stool O&P (x3 to increase yield), stool antigen testing, or stool PCR.
- Organisms must be distinguished from non-pathogenic Entamoeba species.
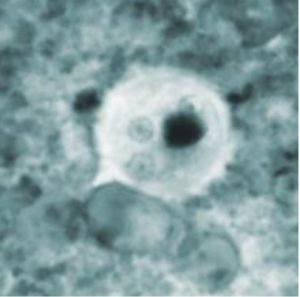
- The number of nuclei (4) can be helpful.
- Pathognomonic findings of pathogenic E. histolytica would be visualizing ingested RBCs within the trophozoite.
- Stool antigen and stool PCR, where available, distinguish between species.
- Extraintestinal Amebiasis, like amebic liver abscess is typically made by the combination of imaging findings, risk profile, and serology for E. histolytica.
- Stool testing is frequently negative.
- Organisms must be distinguished from non-pathogenic Entamoeba species.
