Case adapted from
Khosla A, Singhal S, Jotwani P, Kleyman R. Cerebral Toxoplasmosis As the Initial Presentation of HIV: A Case Series. Cureus. 2022 Mar 21;14(3):e23359. doi: 10.7759/cureus.23359. PMID: 35475054; PMCID: PMC9018902
At home, she has been speaking insensibly and described a constant “knocking” inside her head. Her family notes that she was having similar symptoms in Liberia, before moving to her current home in Fargo, North Dakota, three weeks ago. The siblings are unaware whether any diagnosis or treatment was provided there. Otherwise, her medical history is notable for hypertension, and she has had limited primary care with no prior cancer screenings.
Initial labs were normal except WBC 2.4, Sodium 132, and Potassium 3.2.
Questions for consideration
- What is the most likely pathogen?
- How and when (most likely) did this patient acquire this infection?
- What might have been the symptoms during initial infection with this pathogen?
- What stage/s of the organism is the infectious stage for humans? What stage of the organism is found in the tissue of humans with the disease?
- What are the main risk factors for disease related to this pathogen?
- How do the imaging findings for this disease compare to the imaging findings of another tissue-invasive parasite, Taenia solium?
Read
Micro-ID Dendritics: Leishmania, Toxoplasma, Trichinella, Toxocara, and Schitosoma.
Watch
Toxoplasmosis
- Epidemiology
- Clinical
- Diagnosis
- Treatment
- Prevention
- Key concepts
Transmission to humans
- Ingestion of infected or contaminated food/water.
- Oocysts in soil from cat feces.
- Raw/undercooked meat.
- Transplacental.
- Blood transfusion or organ transplantation.
Tissue cysts remain latent in tissue.
- Can reactivate during immunosuppression.
Adapted from RWJF Slides on Medically Important Protozoa. The predominant mode of transmission for Toxoplasma varies by region. For instance, in France raw/undercooked meat is the predominant mode. In Central America, stray cats shed oocysts that survive in soil. United States prevalence of seropositivity: 22.5%.
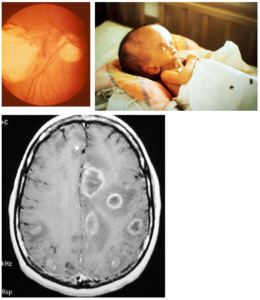
Congenital infection
- Hydrocephalus/intracranial calcification/chorioretinitis
Normal hosts
- Asymptomatic > fever/lymphadenopathy.
- Chorioretinitis.
Immunocompromised (HIV > others)
- Ring-enhancing brain lesions.
- Disseminated infection.
Presumptive Dx
- Neurologic symptoms in patient with low CD4 (AIDS), ring-enhancing lesions in brain on CT scan and + serology.
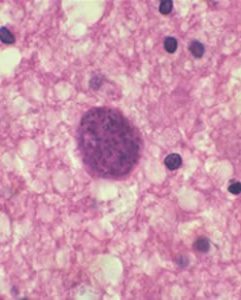
Direct identification of organisms
- Tissue biopsy
Serologic testing
- IgM for primary infection.
- IgG for reactivation.
HIV
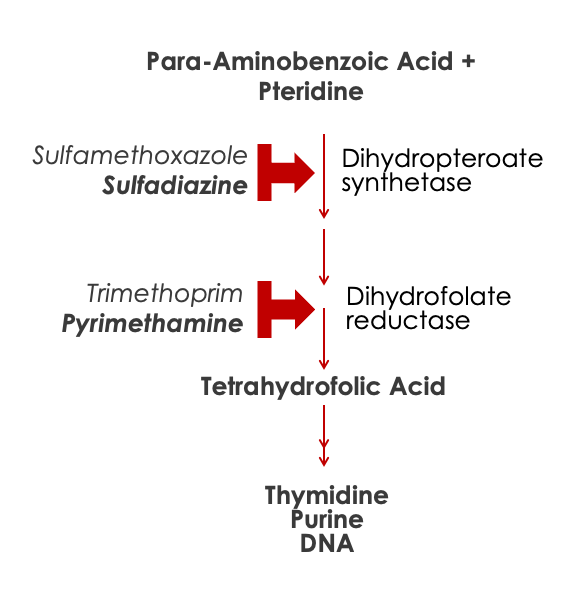
- (CD4 < 100) Prophylaxis with TMP-SMX if IgG+.
Pregnant women
- Avoid cats and raw meat.
Micro: Tissue protozoa; disseminate and encyst.
Epidemiology: Oocysts from cat feces, or undercooked meat.
Clinical:
- Congenital:
- Hydrocephalus.
- CNS calcifications.
- Chorioretinitis
- Normal Immunity:
- Flu-like illness with adenopathy.
- Chorioretinitis.
- Immune Suppressed:
- Seizures.
- Ring-enhancing lesions on head CT.
Diagnosis: Mostly clinical dx; CT imaging; serology
Treatment: Pyrimethamine-Sulfadiazine.
Prevention:
- Cook meat well.
- Take care with cat feces.
- TMP-SMX in AIDS.
Toxoplasma gondii can cause congenital defects and cysts in brain and other tissues that reactivate with immunosuppression.

Test your knowledge
Toxoplasma gondii
Most likely, this patient acquired toxoplasmosis some time ago while in Liberia. Toxoplasmosis is most often acquired through the ingestion of the organism in contaminated soil, water, or food or in undercooked meat from an animal infected with Toxoplasma. Clear infection rates can be difficult to establish since most acute infections are asymptomatic, so seroprevalence is often used as a surrogate. Seroprevalence of Toxoplasmosis is higher in countries outside of the United States, with rates of seropositivity decreasing relative to economic development. Across all countries, seroprevalence increases with age likely correlating with cumulative exposure risk over time.
Acute toxoplasmosis infection is often asymptomatic. When symptomatic, the most common manifestation is regional or generalized lymphadenopathy. When generalize symptoms (fever, malaise, headache) are present, the syndrome can mimic mononucleosis.
There are two infectious stages to humans:
- Oocysts: The product of sexual reproduction, which are excreted in the feces of the definitive host (felines). These structures are highly contagious and may remain viable in the environment for many years in the soil or water.
- Bradyzoites are the structures that form when a mammal is infected with oocysts that invade across the GI lumen and encyst in tissues. When this occurs in animals meant for food, undercooked meat containing bradyzoites infects the human.
- Immunosuppression. In particular, advanced cell-mediated immunodeficiency related to AIDS is the most common risk factor for reactivation disease, manifested as CNS infection.
- Developing fetuses also have limited immune response to Toxoplasmosis, and primary infection in a pregnant woman can lead to congenital toxoplasmosis (T in TORCH).
Image findings of Cerebral Toxoplasmosis and Neurocysticercosis have many overlaps and can manifest as “ring-like lesions” on CT and MRI.
In general, lesions of neurocysticercosis have a clear cystic structure (a “hole”) compared to Toxoplasma, which tends to be more mass-like. The peri-lesional edema (enhancement) is more variable in neurocysticercosis, with very old lesions without active organism having little to no ring-enhancement.
CNS Toxoplasmosis is classically associated with significant edema. Both agents can cause obstructive hydrocephalus. In the case of neurocysticercosis, this is due to a cyst physically obstructing outflow. In CNS toxoplasmosis, hydrocephalus is usually associated with massive edema.