Superficial
Tinea/Dermatophytes
Molds that use keratin as nutritional source.
Trichophyton, Epidermophyton, Microsporum are the most common genera. They are transmitted to humans from direct contact with infected skin scales. They infect keratinized layer of cells (skin and nails) and do not invade underlying tissue. Clinical manifestations are due to inflammatory response and named for the area involved: Tinea capitus (head), tinea corporis (body, ring-worm), tinea pedis (foot), tinea manus (hand), and onychomycosis (nail). Diagnosis is made from KOH prep on skin scrapings. Microsporum shows green florescence with UV lamp. Treatment with topical antifungal creams. Steroids sometimes included with antifungal cream to decrease inflammation, but may prolong disease course. Toenail infection (onychomycosis) is difficult to treat.
Malassezia furfur
Common components of normal skin microbiome, but can cause infection in overgrowth.
These fungi require lipids for growth and are found more abundantly in sebaceous areas of the body, with torso most common. Infection is called pityriasis or tinea versicolor and presents with hypo or hyper pigmented patches. KOH prep shows ‘spaghetti and meatball’ of the budding yeast and filamentous or noodle hyphae.
Subcutaneous
Sporothrix schenckii
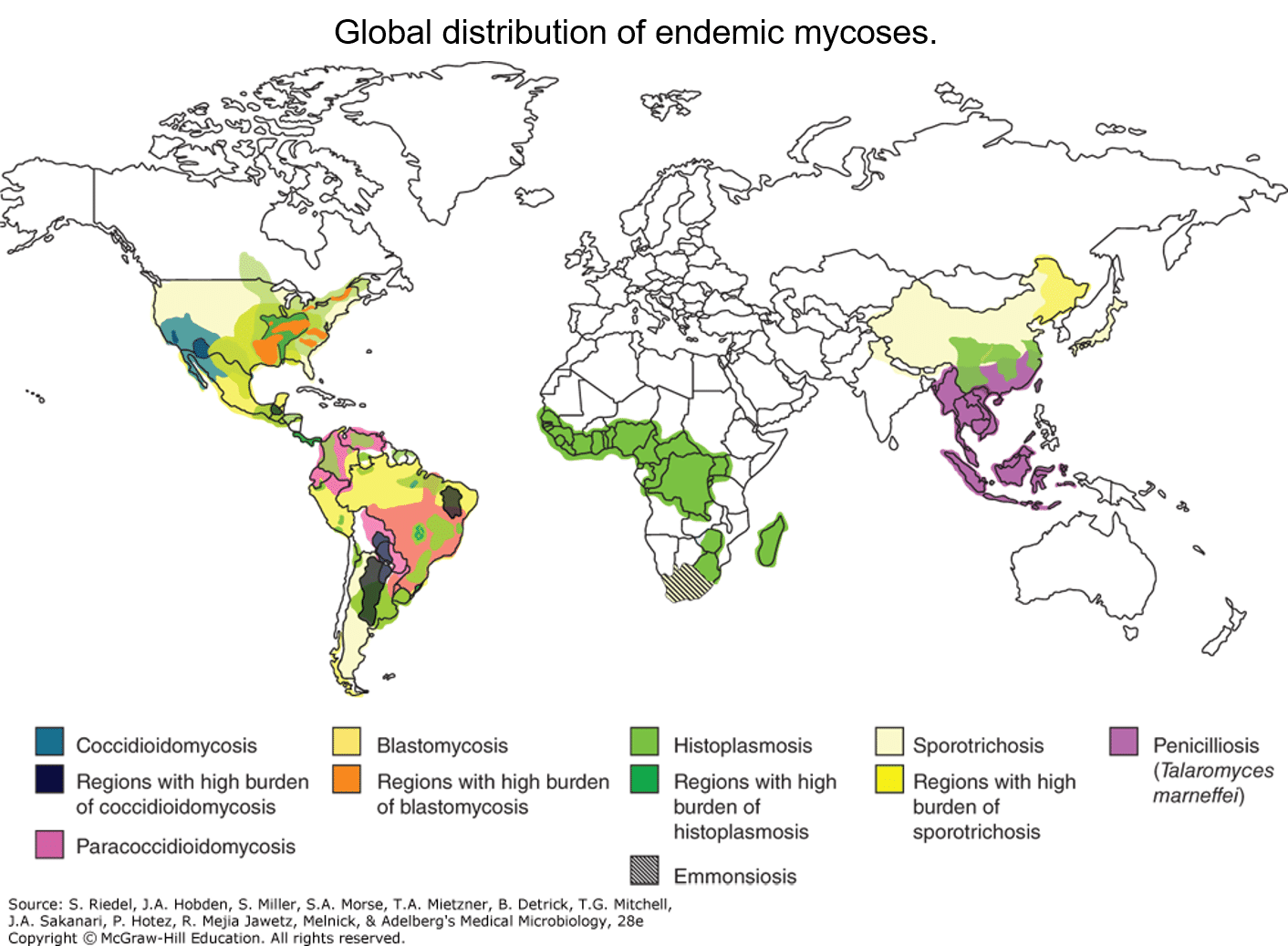
Thermally dimorphic (mold in soil, yeast in body temps) and is found naturally in the soil or vegetation.
Causes lymphocutaneous syndrome “marching up the arm” after mold spores enter a puncture wound or small cracks in skin. Rose growers, Christmas tree growers, and gardeners at risk. Nocardia, non-tuberculous Mycobacteria (M. marinum), and cutaneous leishmaniasis can cause this syndrome. Can disseminate in immunocompromised. Itraconazole is preferred treatment.
Opportunistic
Candida
Part of normal human flora in mucous membranes and skin.
Candida albicans is certainly the most common, but C. glabrata, C. krusei, and more recently C. auris species are emerging as important human pathogens that are difficult to treat. Candida cause invasive infection opportunistically when normal defenses are broken or microbiome disrupted with antibiotics.
Mild clinical infections include thrush in the oropharyngeal or esophageal mucosa, vaginal candidiasis (yeast infection), and cutaneous candidiasis (diaper dermatitis).
Serious disseminated infections can be seen in immunosuppressed persons, particularly under pressure of broad-spectrum antibacterials. Blood stream infections, hepatosplenic infiltration, and endocarditis are feared complications. Chronic mucocutaneous candidiasis occurs in children with primary T-cell immunodeficiency.
Microscopic examination of involved tissue usually demonstrates yeasts with pseudohyphae. In its benign colonizing state, only yeasts are seen. It is easily grown on Sabouraud’s agar. The germ tube test distinguishes C. albicans from other species.
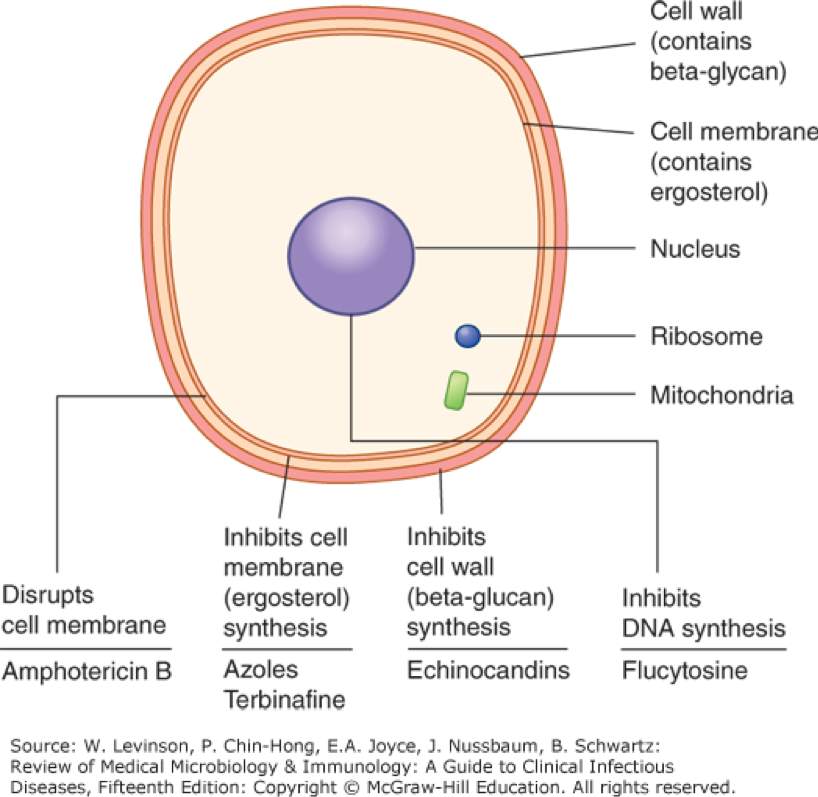
Treatment of mild infections can be topical with nystatin or azole. Serious infections can be treated with fluconazole (albicans only), echinocandins, or amphotericin.
Cryptococcus neoformans
Ubiquitous environmental fungus (strongly linked with pigeon droppings) and is the only yeast form with thick polysaccharide capsule.
Transmission is through inhalation of airborne yeast cells. Clinical disease is most often seen in persons with cell-mediated immunodeficiency. Flu-like illness and pulmonary disease/fungal pneumonia can occur. Crytpococcal meningitis is important cause of meningitis in persons with AIDS; it has been reported in immunocompetent persons with significant exposure to the fungus. CNS disease is characterized as a subacute or chronic meningitis. Very elevated opening pressures are typical and are often the cause of neurologic impairment.
Organisms can be visualized in the CSF with India ink smear where small yeasts with thick capsules are seen. The cryptococcal antigen test is an agglutination test that can be rapidly done on CSF or serum. Cryptococcus may grow in standard blood cultures. Treatment is with Amphotericin and fluconazole, often with flucytosine.
Aspergillus fumigatus
Ubiquitous mold in environment.
It is not dimorphic. Microscopically, it appears as mold with septate hyphae that branch at V-shaped angles, invasion with angioinvasion is seen on pathologic specimens in invasive disease. Transmission is usually through inhalation of airborne spores. It is an opportunistic pathogen and poses greatest risk of invasive disease in immunosuppressed persons, especially those with hematologic malignancies, stem cell transplant, and myeloablative chemotherapy.
There are three distinct clinical forms of aspergillus disease:
Mucormycosis/Zygomycosis
Molds with non-septate broad hyphae that branch at 90-degree angle.
They are not dimorphic and are found ubiquitously in the soil. Transmission is through inhalation of airborne spores. They cause invasive and necrotic mucosal disease in the nasal and sinus tissue that can invade into CNS/brain. Disease mostly found in patients with ketoacidosis and leukemic patients. Surgical debridement if possible is required, systemic amphotericin B is used, but very high mortality associated with this disease.
Pneumocystis jiroveci (formerly carinii) (PCP)
Yeast with many protozoan qualities.
It is transmitted by inhalation where it can cause respiratory infection. Humans are the reservoir and most infections are asymptomatic. Immunosuppression, especially HIV/AIDS, is major risk factor for clinical disease. It is the most common opportunistic infection among persons with CD4 < 200 in the US. PCP pneumonia is indolent in onset and causes interstitial pneumonia that can progress to respiratory failure. Hypoxia is often out of proportion to physical examination findings and serum LDH markedly elevated. Diagnosis is usually accomplished with bronchial secretion silver stain or PCP antigen stain.
Treatment is Trimethoprim-sulfamethoxazole (TMP/SMX). Prophylaxis with TMP/SMX is recommended for persons with HIV and CD4 <200.
Regional
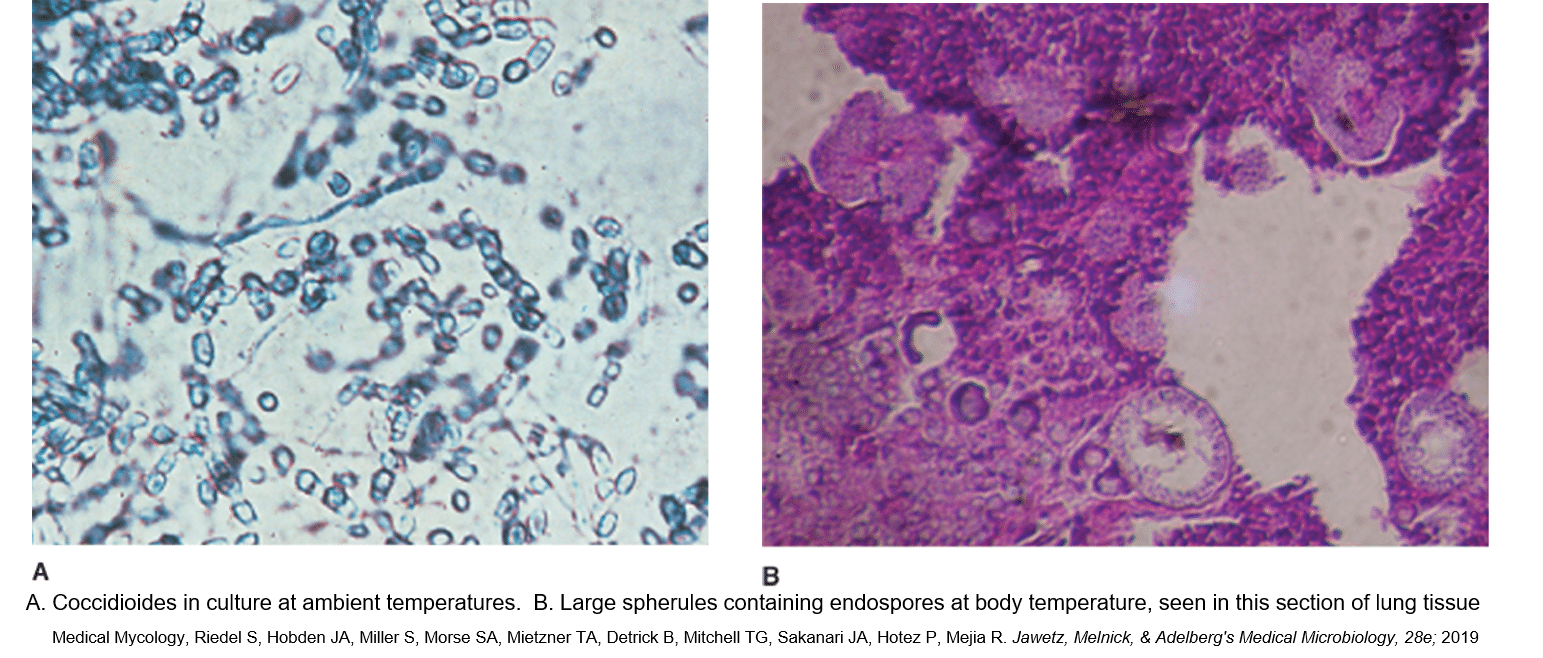
Coccidioides immitis
Thermally dimorphic (mold in cold, yeast in heat).
It is found in arid regions and in western hemisphere is found in the arid climates of the SW US and central America. It is hyperendemic in areas of Arizona. Transmission is from inhalation of airborne arthrospores. Differentiation occurs in the lungs, forming endospores that release spherules that disseminate within the body. Histologically tiny spores within larger endospore is characteristic. C. immitis has tropism for CNS.
Symptoms of acute infection can range from asymptomatic to acute “valley fever” which is characterized by fever, dry cough, inflammatory arthralgias and may have erythema nodosum. Pulmonary infiltrates and symptoms of pneumonia can occur. Coccidioides should be considered in differential for persons with community-acquired pneumonia in hyperendemic areas. Pulmonary lesions may evolve into thin-walled cavities. Disseminated infection is more common in setting of defects in cell-mediated immunity and children where meningoencephalitis can occur.
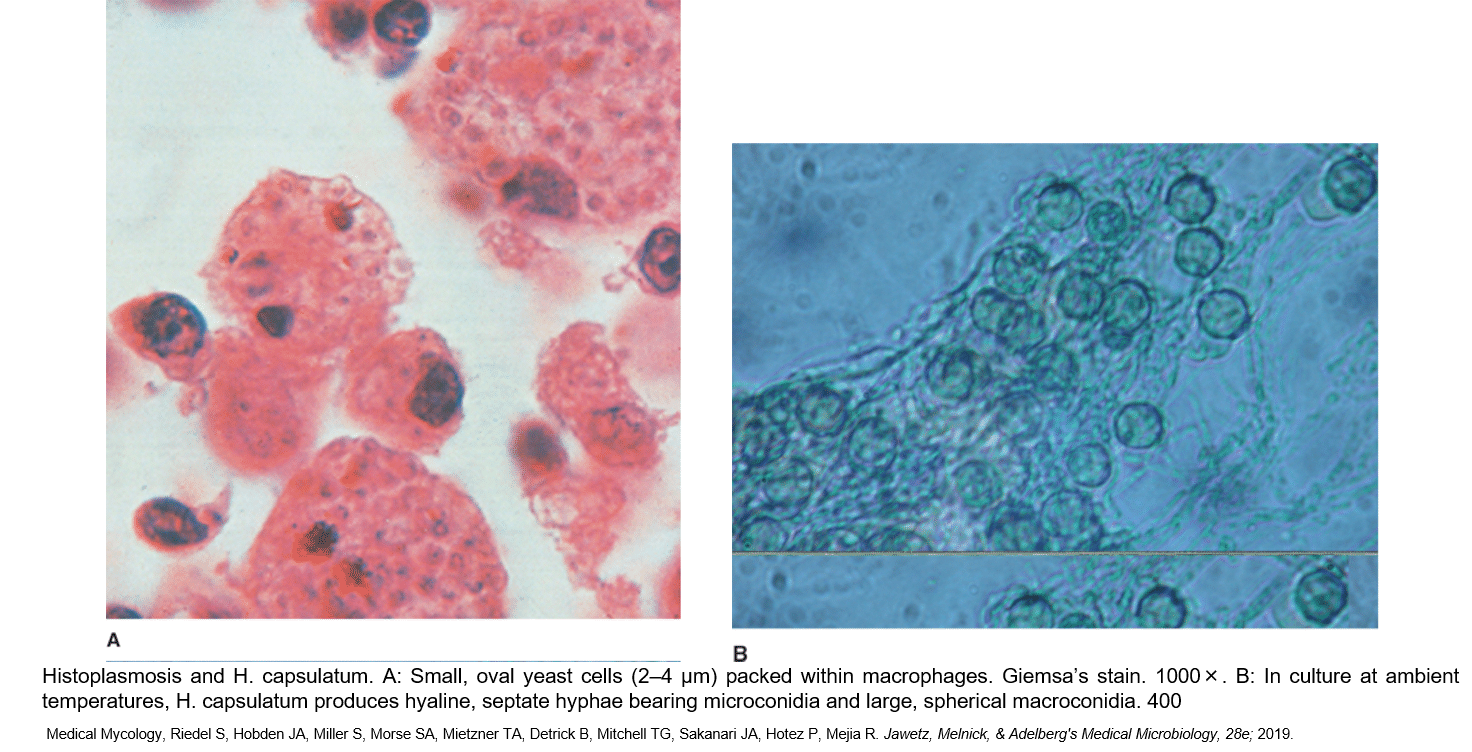
Histoplasmosis capsulatum
Thermally dimorphic (mold in cold, yeast in heat).
The mold grows preferentially in soil enriched with nitrogen from bat and bird droppings. The fungus is endemic in the Ohio and Mississippi river valleys. Transmission is from inhalation of microconidia. Microscopically small yeast forms are seen within macrophages. The pathogenesis is similar to pulmonary tuberculosis and granulomatous response is mounted. Most infections are contained within granulomas, but disseminated disease can occur in setting of depressed cell-mediated immunity. Disseminated disease may mimic military TB with fevers, night sweats, and reticuloendothelial involvement. Diagnosis of disseminated disease can be made with urinary test for Histoplasma Antigen (US only), or identification of yeast forms in tissue biopsy, or bone marrow aspirate smear and culture. Treatment is with Amphotericin or Itraconazole.
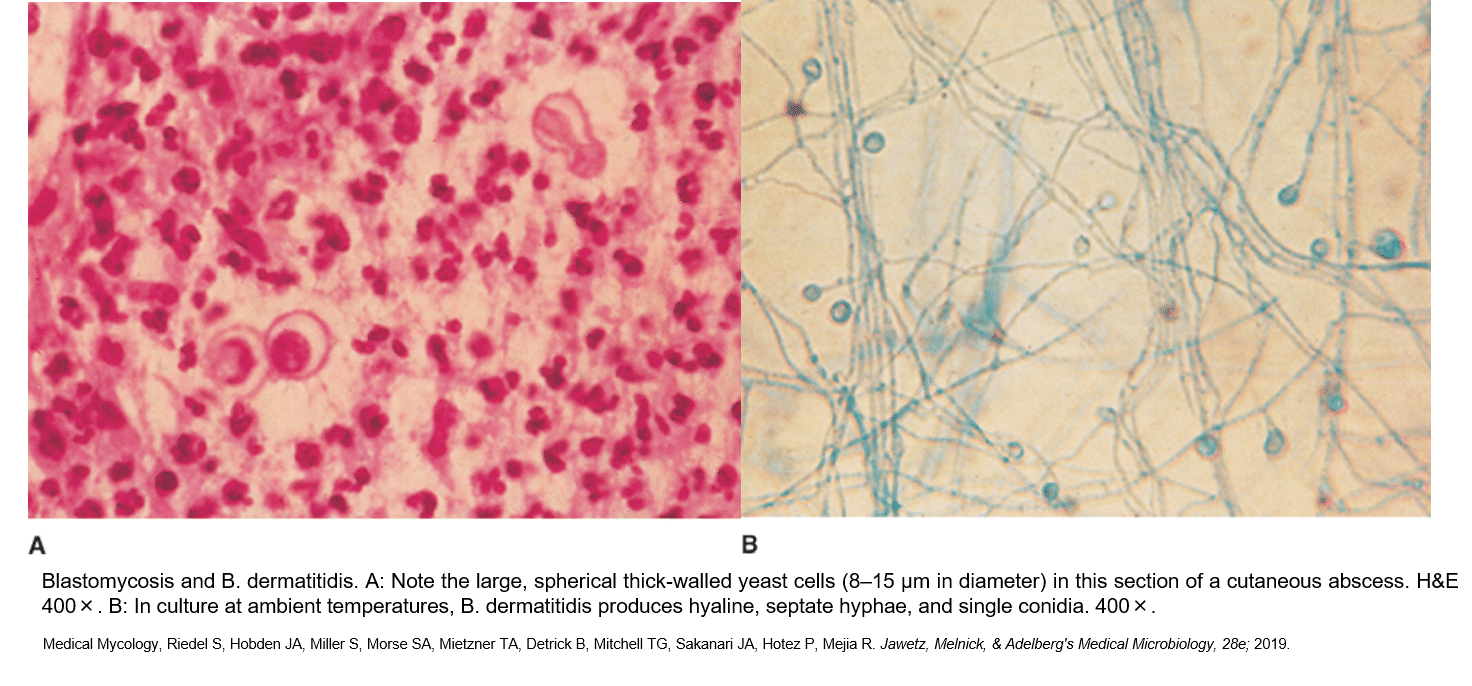
Blastomycosis dermatitidis
Thermally dimorphic (mold in cold, yeast in heat).
The yeast form is a single, broad-based bud with thick refractile wall. It is endemic in the upper Midwest US. Transmission is through inhalation of airborne spores. Primary infection in the lung is similar to Histoplasma and granulomatous inflammation generally limits the disease. Dissemination is rare, but when it occurs, seeding and abscess formation in the skin, bones, and brain are characteristic. Itraconazole is treatment of choice.