- Optional Reading
-
Clinically Oriented Anatomy, 8th ed., Axilla section through Brachial plexus block.
Definition and boundaries
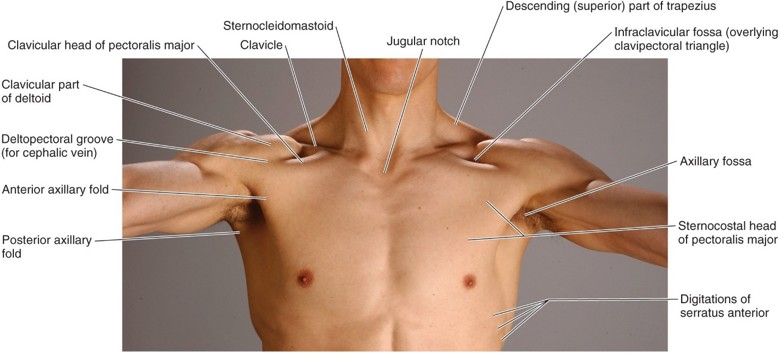
Figure 9.1 CLINICALLY ORIENTED ANATOMY, 7TH ED., FIGURE 6.3.
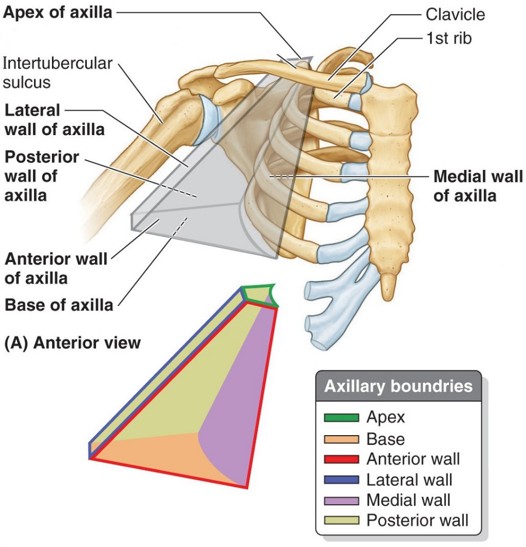
The axilla is the pyramid-shaped region between the lateral wall of the thorax and the medial border of the arm. It is the conduit through which nerves, blood vessels, and lymphatics pass between thorax and neck above and upper limb below. The axilla has an apex, a base, and four walls.
Projects into the root of the neck, between the clavicle and first rib.
Curved—formed by the skin of the armpit.
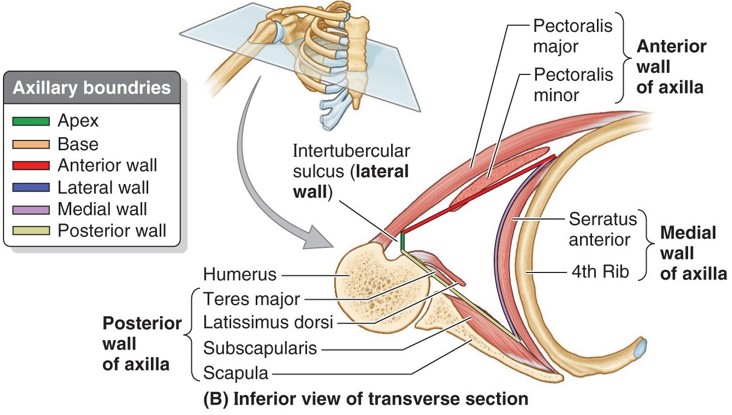
- Anterior wall: Pectoralis major and minor muscles, clavipectoral fascia, and clavicle. The clavipectoral fascia is a thick sheet of deep fascia that passes vertically from the chest wall to the inferior border of the clavicle. It encloses the pectoralis minor and is penetrated by the cephalic vein and the pectoral nerves and vessels.
- Posterior wall: Subscapularis, teres major, and latissimus dorsi muscles.
- Medial wall: Wide—formed by the serratus anterior muscle on the thoracic wall.
- Lateral wall: Narrow—formed by the portion of the proximal humerus containing the intertubercular sulcus. This is where the bulky muscles of the anterior and posterior axillary walls converge and attach to the humerus.
The axillary fossa (armpit) is the hair-covered, dome-shaped external feature visible when the upper limb is fully abducted. It is the floor of the axilla, bordered by two bulky, easily palpable axillary folds composed of skin, fascia, and large muscles that move the upper limb.
The anterior axillary fold contains the pectoralis major muscle.
The posterior axillary fold contains the latissimus dorsi and teres major muscles.

Apertures in the posterior wall of the axilla allow structures arising in the axilla to enter other regions (scapular region, posterior compartment of arm). Geometry buffs will appreciate their shapes and names = Quadrangular and triangular spaces. We will examine them in lab. Study Figure 9.2 to determine their boundaries and contents.
Contents of the axilla
Axillary artery

The continuation of the subclavian artery distal to the first rib. The axillary artery itself becomes the brachial artery distal to the teres major muscle. Anatomists and clinicians separate the axillary artery into three parts based on its relationship to the pectoralis minor muscle. Conveniently, each part gives off a number of branches equal to its numeric name.
- Part 1
- Part 2
- Part 3
Part 1 is proximal to the pectoralis minor—it gives off one branch:
-
- Superior thoracic artery: A minor vessel supplying the first couple of intercostal spaces.
Part 2 is posterior to the pectoralis minor—it gives off two branches:
-
- Thoraco-acromial trunk: Supplies the pectoral and deltoid muscles and the AC joint.
- Lateral thoracic artery: Supplies the serratus anterior muscle and the lateral breast quadrants.
Part 3 is distal to the pectoralis major—it gives off three branches:
-
- Anterior and posterior circumflex humeral arteries: Supply the deltoid muscle and the GH joint.
- Subscapular artery: The largest branch of the axillary artery. Divides into circumflex scapular and thoracodorsal arteries. These supply the scapula, scapular muscles, and latissimus dorsi. They were discussed in the shoulder region.
Axillary vein
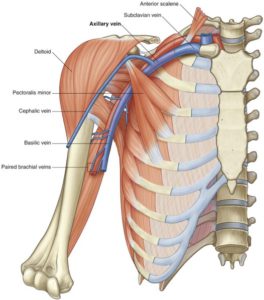
Formed by the union of the basilic vein (the superficial vein along the postaxial border of the upper limb) and the two brachial veins (the venae comitantes of the brachial artery). The axillary vein is normally formed at the inferior border of the teres major muscle. Tributaries of the axillary vein include:
-
- Cephalic vein: The superficial vein on the preaxial border of the upper limb (“body builder’s vein”).
- Veins that correspond to the branches of the axillary artery. The most important is probably the lateral thoracic vein since it communicates with superficial veins in the abdominal wall. This venous connection between abdominal wall and axilla can enlarge if the flow of blood through the inferior vena cava were impeded, providing a collateral route for venous blood to return to the heart.
Draw it
See if you can draw out a flowchart to illustrate this.
Axillary lymph nodes
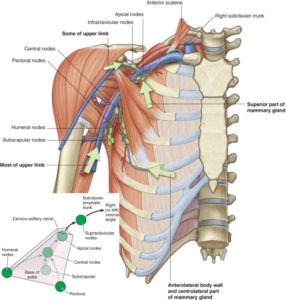
Anywhere from 12–30 nodes, they form an interconnected chain situated around the vessels in the axilla. Lymph from the upper limb, breast, and the superficial tissues (skin and fascia) of the anterior and posterior trunk walls as far south as the umbilicus percolate through axillary nodes. They are often described in groups:
-
- Humeral, subscapular, and pectoral nodes are the more peripheral nodes that receive lymph from the upper limb, scapular region, and chest wall, respectively.
- Lymph from the above three groups of nodes drains to apical axillary nodes, located at the apex of the axilla (of course they are). From here, the subclavian lymph trunk transmits lymph to the right lymph duct on the right side of the body and the thoracic duct on the left side. You will recall that these ducts empty in the right and left jugulosubclavian (venous) angles.
Brachial plexus
The brachial plexus is the “Big Kahuna” of the upper limb = the somatic nerve plexus supplying sensory and motor innervation to the upper limb. It arises from the ventral rami of spinal nerves C-5 to T-1. Nerve fibers within the roots contain:
-
- Somatic efferent fibers that supply skeletal muscles in the upper limb. The cell bodies of these neurons are in the ventral horns of gray in spinal cord segments C-5 to T-1.
- Somatic afferent fibers that convey general sensations of touch, pain, pressure, and temperature from the skin and proprioception from muscles and joints in the upper limb. The cell bodies of these pseudo-unipolar neurons are in the C-5 to T-1 dorsal root ganglia.
- Preganglionic sympathetic fibers that serve the upper limb have cell bodies in the intermediolateral cell column of the upper thoracic spinal cord of (T-1 and T-2). Preganglionic sympathetic axons synapse on postganglionic cell bodies in cervical and upper thoracic chain ganglia. From here, postganglionic axons pass into the brachial plexus via gray rami communicantes.
Question
Which structures in the upper limb receive sympathetic innervation?
Parts of the brachial plexus
Contemplate this
Run To Drink Cold Beer.
- Roots
- Trunks
- Divisions
- Cords
The ventral rami of C-5 to T-1 spinal nerves are the roots of the brachial plexus. They arise in the neck, emerging between the anterior and middle scalene muscles. Here they are posterior to the subclavian vein and artery.
Roots unite to form the trunks. C-5 and C-6 form the upper trunk, C-7 continues alone as the middle trunk, and C-8 and T-1 form the lower trunk.
Each trunk splits into an anterior and a posterior division. Anterior divisions supply the anterior compartments of the upper limb (arm, forearm, and palm of hand), while posterior divisions supply the posterior side (arm, forearm, and dorsum of the hand).
Cords contain fibers from the divisions. The cords are named for their relationship to the axillary artery.
The anterior divisions give rise to the lateral and medial cords. The lateral cord contains fibers from the anterior divisions of the upper and middle trunks = C-5, C-6, and C-7. The medial cord contains fibers from the anterior division of the lower trunk = C-8 and T-1. Together the lateral and medial cords supply the anterior compartments of the upper limbs.
All three posterior divisions unite to form the posterior cord. The posterior cord therefore contains nerve fibers from C-5 to T-1 that are heading for the posterior compartments of the limb.
Terminal branches
Advice
Learn these big dudes first. After you master them, then learn the smaller side branches of the brachial plexus.
The largest nerves in the upper limb are the so-called terminal branches of the cords. There are five of them.
- Musculocutaneous nerve (C-5 and C-6): Innervates the muscles in the anterior compartment of the arm, then passes distal to the elbow to become the lateral cutaneous nerve of the forearm, supplying the skin there.
- Take home: Musculocutaneous nerve = elbow flexion.
- Lateral root of the median nerve: Joins the medial root from the medial cord to form the median nerve.
- Ulnar nerve (C-8 and T-1): Supplies a few muscles in the forearm, and skin along the medial border of the forearm, but its main job is to supply the majority of intrinsic muscles of the hand.
- Take home: Ulnar nerve = hand grip.
- Medial root of the median nerve
- Axillary nerve (C-5 and C-6): Supplies the deltoid and teres minor muscles and skin of the deltoid region.
- Take home: Axillary nerve = shoulder abduction.
- Radial nerve (C-5 to T-1): Supplies muscles in the posterior (extensor) compartments of the arm and forearm, as well as skin on the posterior surfaces of the arm,forearm, and hand.
- Take home: Radial nerve = elbow and wrist extension.
The median nerve (C-6, C-7, C-8, and T-1), one of the terminal branches, is formed by the union of roots from the medial and lateral cords.
-
- It supplies all of the muscles in the anterior compartment of the forearm (except for 1 and ½ muscles) and most of the muscles that move the thumb in the hand—specifically those located in the thenar eminence.
- It is the main nerve of forearm pronation, flexion of the wrist, flexion of the digits, and movements of the thumb.
- It supplies sensation to the pulpy tips of the first 3 fingers.
- Take home: Median nerve = wrist flexion and thumb movements.
Clinical correlation
When treating brachial plexus injuries, clinicians often distinguish between supraclavicular and infraclavicular parts of the plexus. The roots, trunks and divisions are located superior to the clavicle = these constitute the supraclavicular part. The cords and terminal branches make up the infraclavicular part of the plexus.
A supraclavicular nerve block is administered to the proximal parts of the plexus—therefore, it affects a wider region of the upper limb. Since it provides fast acting and profound anesthesia, it is known as a “spinal of the upper limb.” One drawback is proximity to the axillary artery and cervical pleura means there is danger of entering an artery or pleural cavity (pneumothorax) with the injection. Ultrasound guidance of the needle helps avoid this.
Lost in Lab?
Look for the letter “M” surrounding the axillary artery. “M” means Merging of the terminal branches of the lateral and medial cords. The Median nerve is at the center of the “M.” Look at Figure 9.9—do you see the “M”?
Figure 9.9 GRAY’S ANATOMY FOR STUDENTS, 3RD ED., FIGURE 7.53.
Side branches of the brachial plexus
The side branches are numerous and arise from roots, trunks, and cords. There are no side branches from the divisions of the brachial plexus, thank heavens!
- Dorsal scapular nerve (C-5): Supplies the rhomboid muscles and the levator scapulae muscle.
- Long thoracic nerve (C-5, C-6, and C-7 roots): An old friend here, it supplies the serratus anterior.
(Both of these are from the upper trunk = C-5 and C-6.)
-
- Suprascapular nerve—supplies the supraspinatus and infraspinatus muscles.
- Nerve to subclavius muscle
- Lateral pectoral nerve: Supplies the pectoralis major.
- Medial pectoral nerve: To pectoralis major and minor.
- Medial cutaneous nerve of arm: Supplies skin of the medial arm. NOTE: these nerve fibers intermingle in the arm with fibers from the intercostobrachial nerve (= the lateral cutaneous branch of the 2nd intercostal nerve). Thus, T-2 fibers figure in the innervation of the medial arm skin.
- Medial cutaneous nerve of forearm: To medial forearm skin.
- Upper and lower subscapular nerves: Both supply the subscapularis muscle; the lower subscapular nerve also supplies the teres major muscle.
- Thoracodorsal nerve: Supplies latissimus dorsi. In old-fashioned anatomy books, this nerve was called the “middle subscapular nerve,” since it branches from the posterior cord between the upper and lower subscapular nerves.
Mnemonic
If you dig mnemonics, here’s one for remembering all the branches from the posterior cord (terminal branches + side branches):
ULTRA:
Upper subscapular
Lower subscapular
Thoracodorsal
Radial, and
Axillary.
The unfortunate thing here is that they are not listed in the correct topographic order. Oh well.
Learn it by drawing it
In lab, we will practice drawing the brachial plexus in three steps:
-
- First, the basic scaffold of the plexus = roots, trunks, divisions, and cords.
- Next, add the five terminal branches.
- Complete the masterpiece by adding all the side branches. To do this, we will use a scheme that adds three nerves to the base drawing—repeated four times (this makes 12 strokes of the pen or pencil). This is the “FOUR 3s.”
- The procedure is outlined at this link: Learn the brachial plexus in five minutes or less (or download a PDF). We will practice drawing the brachial plexus using this procedure in lab as well.
Clinical correlation
To effectively diagnose musculoskeletal and neurological problems in the upper limb, clinicians and students need to be able to distinguish between pathologies caused by damage to nerve roots proximally as they emerge to form the brachial plexus, and those caused by injuries to or impingement of peripheral nerves distally.
A thorough understanding of brachial plexus architecture is the key, including both terminal and side branches arising from the plexus, and the spinal nerve segments they contain. The brachial plexus should be a big ticket item when studying for Boards!
- Tying it all together with Acland