- Optional Reading
- Clinically Oriented Anatomy, 8th ed., Overview of thorax, Pectoral and scapular region, Breasts.
Pectoral region
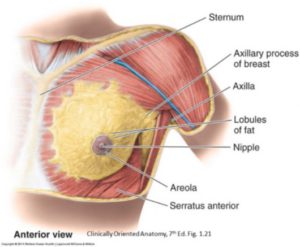
The pectoral region is located in the anterior thorax on each side of the sternum, between the clavicle and axilla (armpit). It links the upper limb to the trunk and supports the breast.
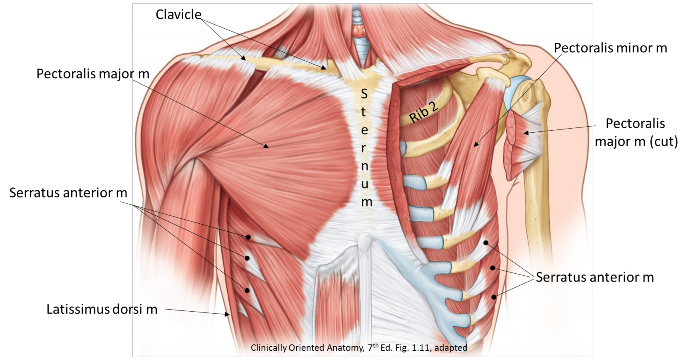
Figure 8.1
Muscles of pectoral region
There are 3 main muscles in this region. Since they move the upper limb, we will also study them in the limb section of the course.
- Attachments:
- Proximal: Clavicle, sternum, and costal cartilages
- Distal: Proximal humerus
- Action: Adducts and internally rotates humerus
- Innervation: Medial and lateral pectoral nerves (from the brachial plexus)
- Blood supply: Pectoral branch of thoraco-acromial trunk
- Other: The breast rests against its anterior deep fascia (pectoral fascia)
- Attachments:
- Proximal: Arises from 3 consecutive ribs, between ribs 2 to 6 (variable)
- Distal: Coracoid process of scapula
- Action: Protracts and depresses scapula
- Innervation: Medial pectoral nerve (from brachial plexus)
- Blood supply: Pectoral branch of thoracoacromial trunk
- Attachments:
- Proximal: Ribs 1–9
- Distal: Medial border of scapula
- Action: Protracts scapula
- Innervation: Long thoracic nerve (from brachial plexus)
- Blood supply: Lateral thoracic artery
Clinical correlation
Damage to the long thoracic nerve can paralyze the serratus anterior muscle. This causes dysfunction in the stabilizing function the muscle has in keeping the scapula flush against the thoracic wall. The consequence is protrusion of the medial border of the scapula (“winging of the scapula”), especially prominent when the palms of the hand are pressed forward against a wall.
The axilla
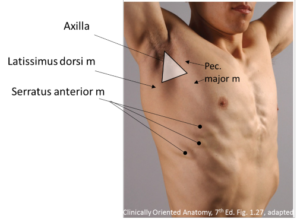
The axilla is the pyramid-shaped space inferior to the shoulder joint, where the arm meets the thorax. It is filled with nerves, vessels, and lymph nodes. Externally, the landmarks of the axilla are the anterior and posterior axillary folds, formed by the underlying pectoralis major and latissimus dorsi muscles, respectively. The depression between the folds is the axillary fossa (armpit). We will consider the axilla in much more detail when we study the upper limb.
Vessels of pectoral region
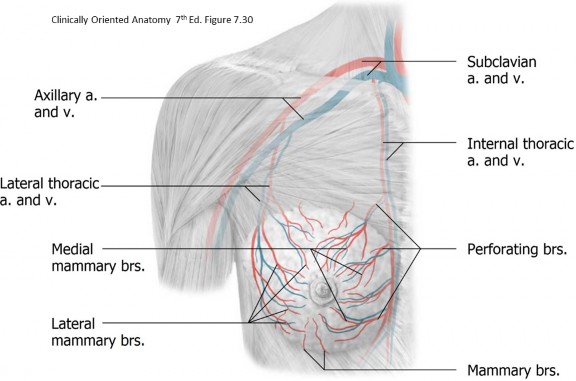
Figure 8.3
- Arteries:
- Axillary artery: This is the continuation of the subclavian artery, distal to the first rib. It courses through the center of the axilla. Anatomists divide it into three parts based on its relationship to the pectoralis minor muscle (1st = proximal to pec minor, 2nd = posterior to pec minor, 3rd = distal to pec minor). Its most important branches to the pectoral region are derived from the 2nd part:
- Thoraco-acromial artery: Its pectoral branches supply the pectoral muscles.
- Lateral thoracic artery: It passes inferiorly along the surface of the serratus anterior muscle. It courses with the long thoracic nerve (which comes from the brachial plexus in the neck).
- Internal thoracic artery: A branch of the subclavian artery, it descends vertically inside the ribcage, just lateral to the sternum. Its branches perforate the chest wall to supply the pectoral region.
- Axillary artery: This is the continuation of the subclavian artery, distal to the first rib. It courses through the center of the axilla. Anatomists divide it into three parts based on its relationship to the pectoralis minor muscle (1st = proximal to pec minor, 2nd = posterior to pec minor, 3rd = distal to pec minor). Its most important branches to the pectoral region are derived from the 2nd part:
- Veins:
- Axillary vein: Formed by the union of the basilic and brachial veins from the arm, it courses through the axilla, becoming the subclavian vein after it crosses the first rib. It receives venous tributaries from the pectoral region.
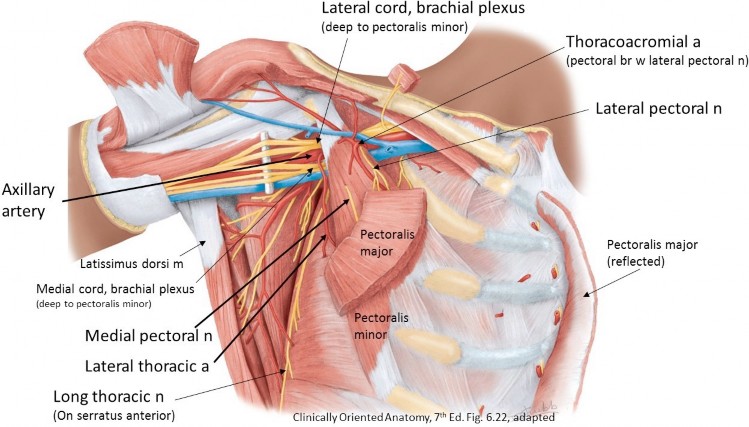
Figure 8.4
Nerves of pectoral region
- The brachial plexus fills the axilla. It is formed in the neck from spinal nerves C-5 to T-1 and innervates the entire upper extremity, which includes the muscles of the pectoral region (which move the limb).
- Lateral pectoral nerve: Arises from the lateral cord of the brachial plexus (hence its name), courses superior to the pectoralis minor, then dives into the deep surface of the pectoralis major.
- Medial pectoral nerve: Arises from the medial cord of the brachial plexus (thus its name) and usually penetrates and innervates the pectoralis minor first; then it passes into the pectoralis major.
- Long thoracic nerve: Arises from the roots of the brachial plexus (C-5, C-6, and C-7) in the neck, then passes down medial wall of the axilla to supply the serratus anterior.
- Intercostal nerves: These segmental nerves run along the inferior borders of the ribs, encircling the chest wall. They give off lateral cutaneous branches (sensory to skin) in the mid-axillary line, that emerge between the “serrations” of the serratus anterior muscle, and anterior cutaneous branches (sensory) just lateral to the sternum that perforate the pectoralis major in order to reach the skin. See the thoracic wall section for more details (not shown in Figure 8.4).
Gross anatomy of the breast
- Females
- Males
The base of the breast usually extends from the lateral sternal border to the mid-axillary line, and vertically from the 2nd–6th ribs. Their size and shapes are determined by the quantity and arrangement of adipose tissue. Growth of the breasts is a secondary sex characteristic that involves accumulation of both superficial fascia and glandular tissue. The breast extends under the pectoralis major into the axilla. This lateral extension is called the axillary tail.
Male breasts are rudimentary throughout life and have no function, but they are landmarks on the chest. The nipple is usually located at the level of the 4th intercostal space, just lateral to the midclavicular line. Some undeveloped glandular tissue is present in the male breast. This tissue may enlarge during puberty or later in life due to hormonal imbalance or medications—a condition called gynecomastia. Men, too, can get breast cancer, although it is quite rare, accounting for less than 1% of cases.
External features of the breast
Internal anatomy of the breast
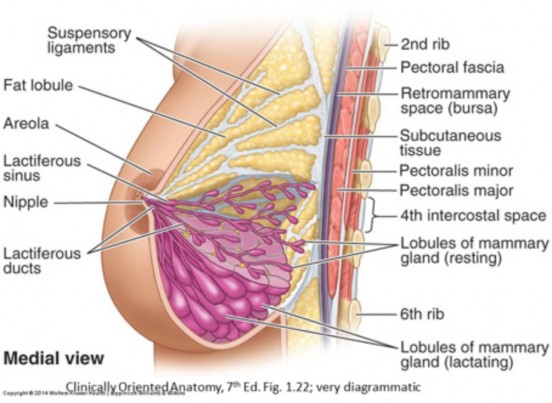
Figure 8.6 Breast location and internal anatomy.
The fully formed breast consists of:
The glandular tissue of the breast is arranged into 15–20 lobes (sometimes also called lobules). Each lobe is drained by a lactiferous duct. These open independently on the surface of the nipple. Each duct is dilated just below the nipple, producing a lactiferous sinus. Beginning at the nipple and proceeding into the breast, lactiferous ducts branch and rebranch until they reach “dead ends” called terminal ductules—in the non-pregnant state. These enlarge and acquire secretory units during pregnancy. It should be noted that the lobes of the breast can’t be seen during dissection since they are quite diffuse, rather than being cone-shaped as they are often depicted. They are however the functional units (parenchyma) of the breast.
The fibrous connective tissue in the center of the breast in which the glandular tissue is embedded sends extensions outward to connect to the dermis of the overlying skin. These bands of connective tissue are called suspensory ligaments (Cooper’s ligaments). They are best developed in the upper quadrants of the breast. Their function is to support the breast on the chest wall. The suspensory ligaments degrade with age, producing sagging of the breasts.
The fatty tissue of the breast is condensed into a more robust layer of superficial fascia along its base, where the breast abuts the pectoralis major. This so called retromammary fascia is separated from the underlying pectoral (deep) fascia by a potential space, the retromammary space. This allows the two layers of fascia to glide on one another, giving the breast mobility on the chest wall.
Blood supply and innervation of the breast
- Arteries
- Medial half: Branches of the internal thoracic artery
- Lateral half: Lateral thoracic artery
- Venous drainage
- Tributaries of the internal thoracic veins (medial breast) and axillary vein (lateral breast).
- Nerves
- Medial and lateral cutaneous branches of the first 6 intercostal nerves.
Clinical correlation
Lack of breast mobility is a sign of pathologic changes to the retromammary space (carcinoma invasion, for example). The retromammary space was at one time a popular location for the placement of implants for breast augmentation. Placement of implants partially under the pectoralis major is now the preferred procedure.
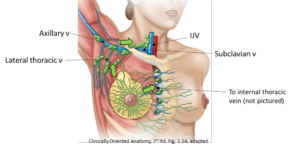
Lymphatic drainage of the breast
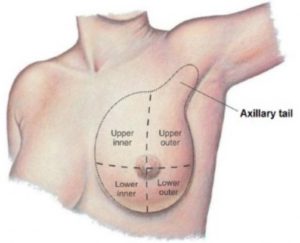
Deep plexuses of lymph vessels are formed around the glandular tissue and ducts. From here, drainage is into two sets of lymph nodes: parasternal and axillary. For descriptive and clinical purposes, the breast is subdivided into quadrants, using the nipple as the center of the clock face. The upper lateral quadrant contains more breast tissue than the other quadrants. Therefore, it is the most common site of breast cancer.
-
- The medial (inner) quadrants of the breast drain to parasternal nodes, located along the internal thoracic vessels on the internal surface of the anterior chest wall.
- The lateral (outer) quadrants of the breast drain to axillary nodes. These are 12 to 30 nodes forming a connected chain around the veins of the axilla. Since the lateral quadrants are larger, about 75% of the breast’s lymph percolates through the axillary lymph nodes. Besides the breast, axillary nodes receive lymph from the upper limb and the superficial tissues of the trunk wall as far inferiorly as the umbilicus.
Clinical correlation
The lymphatic drainage of the breast has important clinical relevance since the breast is prone to neoplastic disease and the main route for metastasis of breast carcinoma is through lymphatic vessels. The concept of “sentinel” lymph nodes applies to the axillary nodes, since they receive most of the breast’s lymph. Sentinel nodes are defined as the first nodes to receive lymph from a cancerous organ. Axillary lymph nodes are arranged in groups within the axilla—some are at its base near the pectoral muscles and others at its apex above the clavicle. Lymph from the breast typically flows through the groups of nodes in the axilla in sequence, from base to apex. The “TNM” (tumor, node, metastasis) system used by clinicians to stage breast cancer takes in to consideration the number and location of axillary nodes involved.
- Tying it all together with Acland