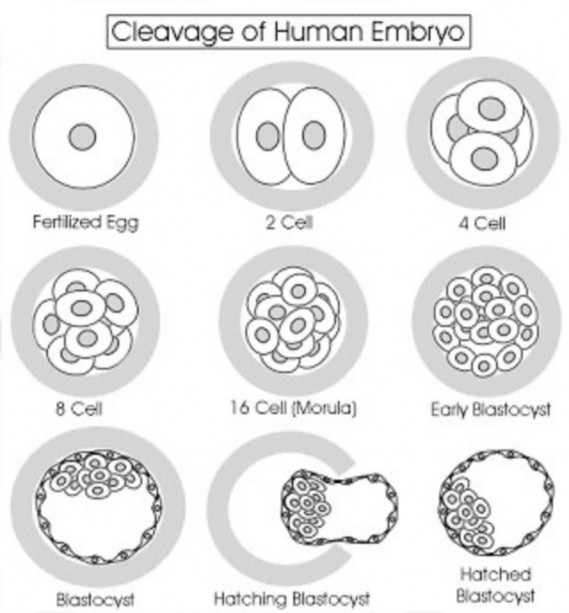
The zygote undergoes mitotic divisions
- About 24 hours after fertilization, the zygote begins to move down the uterine tube toward the uterine cavity while undergoing a series of mitotic cell divisions called cleavage. Each division produces daughter cells called blastomeres. No cell growth occurs during early cleavage, so each mitotic division produces smaller and smaller cells. Blastomeres are pleuripotent cells capable of forming all the cells needed for human development!
- As cleavage continues and the embryo reaches the 8-cell stage, the spherical, loosely joined blastomeres become flattened, to maximize cell-to-cell contact, and snugly joined together. This is called compaction.
- Days 3–4: The embryo reaches the 16-cell stage and is termed a morula (Latin = mulberry), resembling a soccer ball. The morula enters the uterine cavity. At this point, two populations of cells can be recognized:
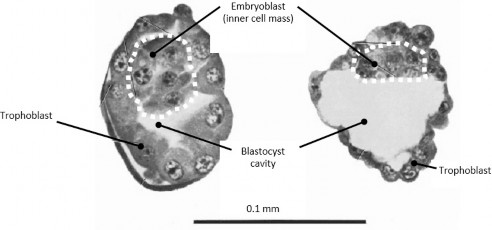
- The single layer of cells around the periphery of the morula is called the trophoblast. Cells are flattened and firmly joined together by tight junctions. These cells will form the fetal membranes of the placenta.
- The inner cells of the morula are known as the embryoblast (a.k.a. inner cell mass). These cells are pluripotent and will give rise to the entire embryo proper. Because they have the potential to develop into all cell types and tissues, these are embryonic stem cells.
Formation of the blastocyst
- Day 5: Fluid accumulates within the morula, ultimately forming a cavity in its center. The embryo now is known as a blastocyst. The trophoblast (future placenta and fetal membranes) surrounds the blastocyst cavity. The embryoblast cells (future embryo) are pushed to one end, giving the blastocyst polarity. This end is known as the embryonic pole. The blastocyst, like the morula, is surrounded by the zona pellucida, a glycoprotein layer. The zona pellucida surrounds the female oocyte when it is ovulated and the sperm must penetrate it in order for fertilization to occur.
Functions of the zona pellucida
- Blocks polyspermy.
- Keeps blastomeres together, facilitating compaction.
- Prevents premature implantation.
- Allows only species-specific fertilization.
- As the blastocyst develops further, the zona pellucida thins and an enzymatic reaction opens a hole. In order for the blastocyst to implant in the uterine wall, it must escape the zona. This process occurs at the end of Week 1 and is known as hatching of the blastocyst. The blastocyst is now “naked” and can interact with the endometrium, the inner lining of the uterus.
Implantation of the Blastocyst
- Day 6: The embryonic pole of the blastocyst adheres to the endometrium and begins implantation. This process involves teamwork = mutual interaction of trophoblast and endometrial cells. The endometrium becomes more vascular and edematous and its glands enlarge. Endometrial cells adjacent to the implantation site grow, increase their metabolic activity, and become laden with lipids and glycogen. These “uber-cells” are called decidual cells. The hormone progesterone induces normal endometrial cells to become decidual cells.
- The endometrium is maintained in its “ready-for-pregnancy state” and is kept from sloughing by progesterone secreted by a corpus luteum in the ovary. When the blastocyst implants, its trophoblast cells produce human chorionic gonadotrophin (hCG), a hormone that prevents the degeneration of the corpus luteum, thus maintaining the supply of progesterone. hCG enters the maternal blood and can be detected in the urine about 10 days after fertilization. This is the basis of early pregnancy testing.
- Normal implantation occurs in the endometrium on either the anterior or posterior wall of the uterus. Ectopic pregnancies occur when a blastocyst implants somewhere besides the endometrium. The most common location is in the uterine tube wall (tubal pregnancy). Other possible sites are the ovaries, the cervix of the uterus, and in the abdominal cavity, adjacent to the uterus and its adnexa (its connected parts = uterine tubes and ovaries).
Clinical correlation
Ectopic pregnancies are serious business, since blood vessels enlarge around the implantation site and are apt to burst and bleed. Abdominal pain and vaginal bleeding accompanied by rising hCG levels are indicators. Ultrasound examination is used to locate the site. Ectopic pregnancies can’t survive, so they must be surgically or chemically removed. Women with a history of pelvic inflammatory disease (PID) are said to be 6 to 10 times more at risk for ectopic pregnancies than are those with no history of PID.