- Optional Reading
- Clinically Oriented Anatomy, 8th ed., chapter 5, Innervation of abdominal viscera section.
Abdominal Viscera
The principal viscera of the abdomen are the esophagus (terminal part), stomach, intestines, spleen, pancreas, liver, gallbladder, kidneys, and suprarenal glands. The esophagus, stomach, and intestines form the digestive (alimentary) tract. The kidneys and suprarenal glands will be discussed in the Urinary System section.
Food passes from the mouth and pharynx via the esophagus to the stomach.
Digestion mostly occurs in the stomach (physical) and duodenum (chemical).
Peristalsis begins in the esophagus and continues to the rectum. In the stomach, the waves move slowly toward the pylorus, and are responsible for mixing of the masticated food mass with gastric juices and for emptying the contents of the stomach into the duodenum.
Alimentary Tract
The abdominal esophagus extends ~3cm from the esophageal hiatus of the diaphragm, at about T10. Where it passes through the esophageal hiatus, it can become constricted and cause dysphagia (difficulty in swallowing).
Can vary a lot in people of different body types. In the supine position, it commonly lies in the RUQ and LUQ (or epigastric, umbilical, and left hypochondrium regions). When erect, the stomach moves inferiorly. For some, a very full stomach can extend into the pelvis!
Relationships with other organs:
-
- Anteriorly: Diaphragm, left lobe of liver, AAW
- Posteriorly: Omental bursa, pancreas, spleen, left kidney, and left suprarenal gland
- Inferolaterally: Transverse colon
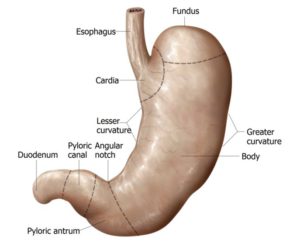
Parts:
-
- Cardia: A narrow ring around the esophageal opening
- No sphincter, but has a physiological “cardiac orifice”: Thick muscular wall that can be tightly closed to prevent stomach reflux
- Fundus: Dome of the stomach
- Can be dilated by gas, fluid, food, or any combination; can be seen in a
radiograph
- Can be dilated by gas, fluid, food, or any combination; can be seen in a
- Body: Most of the stomach, between fundus and pyloric antrum; mechanical digestion
- Pylorus: Outflow portion that regulates the passage of food from stomach into duodenum
- Lies at the level of the transpyloric plane; in an erect patient the location varies from L2 thru L4
- Cardia: A narrow ring around the esophageal opening
Two curvatures:
-
- Lesser curvature: Short concave right border of the stomach
- Attachment site of lesser omentum
- Greater curvature: Long convex left border of the stomach
- Greater omentum is suspended from this curvature
- Lesser curvature: Short concave right border of the stomach
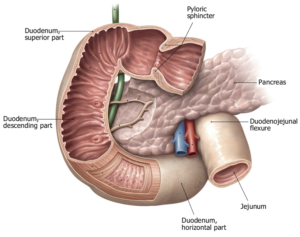
The duodenum leaves the pylorus of the stomach, and is the first section of the small intestine. It has 2 different embryological origins (foregut and midgut) and so has split vascular and neural supply (discussed later).
-
- Begins at the pylorus on the right, its four parts encircle the head of the pancreas, and ends at the duodenojejunal flexure/junction on the left side at ~L2, 2-3 cm to the left of the midline.
- Mostly retroperitoneal
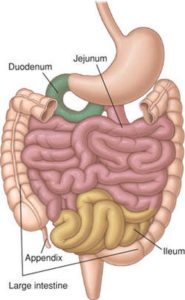
Together: 6–7 m long, with the jejunum being 2/5 of the length
-
- Jejunum: Mostly located in the LUQ (left upper quadrant)
- Ileum: Mostly located in the LRQ (lower right quadrant) at the ileocecal junction.
- Thinner walls, is paler pink, and has more fat in its mesentery (“creeps” onto the tube)
Both contain the same permanent circular mucosal folds, though they are abundant in the jejunum and become fewer until absent at the end of the ileum.
Peristalsis is not forceful in the jejunum and ileum unless an obstruction is present.
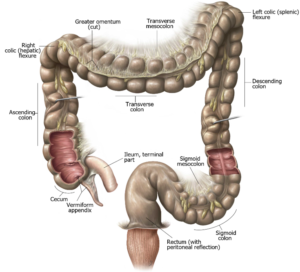
Main function: Water absorption
-
- Most reabsorption of water occurs in the ascending colon. Feces (stools) are formed in the descending and sigmoid colon and accumulate in the rectum before defecation
Parts:
-
- Cecum: Lies in the right iliac fossa in the LRQ, inferior to the ileocecal junction, within 2.5cm of the inguinal ligament
- Appendix: Blind diverticulum containing masses of lymphoid tissue, on the posteromedial side of the cecum, usually tucked into the retrocecal pouch
- Ascending colon: Begins at the cecum, and ends at the right colic flexure
- Secondarily retroperitoneal
- Right paracolic gutter lies between its lateral aspect and the abdominal wall
- Transverse colon: Most mobile of the large intestine and extends from right to left colic flexures.
- Variable position: It’s not uncommon for it to hang to the level of the umbilicus (L3)
- Descending colon: Passes anterior to the lateral border of the left kidney
- Secondarily retroperitoneal
- Forms left paracolic gutter
- Sigmoid colon: S-shaped loop of variable length extending from the iliac fossa to the S2 vertebra (in the true pelvis)
- Intraperitoneal: Connected via sigmoid mesocolon
- Rectum and anal canal: The rectum is fixed, and is continuous with the sigmoid colon at S3; the rest will be discussed in the pelvis section
Accessory Organs
Like the duodenum, it has two embryological origins, therefore two different neurovascular supplies.
-
- 99% exocrine in structure and function; it produces and secretes pancreatic enzymes for chemical digestion. Its endocrine function it to produce and secrete the hormones important for glucose regulation: insulin and glucagon.
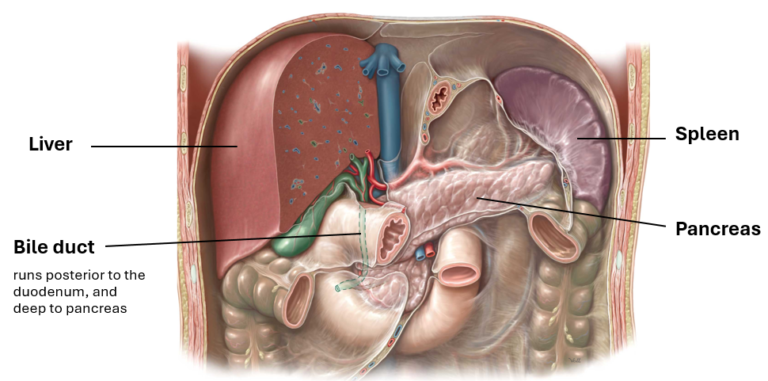
- Retroperitoneal organ overlying and transversely crossing L1–2 (transpyloric plane). It lies posterior to the stomach between the duodenum on the right and the spleen on the left.
- Functions: Every substance absorbed by the small intestine, except fat, goes to the liver. The liver performs many metabolic activities (e.g., glycogen storage and bile secretion).
- Develops from a diverticulum off the foregut, and is the largest internal organ.
- Lies deep to ribs 7–11 on the right, and crosses the midline toward the left nipple. The sharp inferior border between the superior and visceral/inferior surfaces follows the right costal margin.
- Spaces associated with the liver: Subphrenic and hepatorenal recesses
- Sac-like organ inferior to the liver that stores and concentrates the bile produced by the liver.
- Its bile ducts merge with those from the liver and eventually empty into the duodenum.
- Large lymphoid organ about the size of your fist that rests on the left colic flexure in the LUQ
- Associated with ribs 9–11 posteriorly
- Doesn’t extend past the left costal margin, so it is not palpable, unless it is enlarged
- Functions: Lymphocyte proliferation and immune surveillance and response organ. After birth, it removes senescent red blood cells and platelets, recycles iron and globin, and is an RBC reservoir, though not an essential organ.
Neurovascular supply to the gut
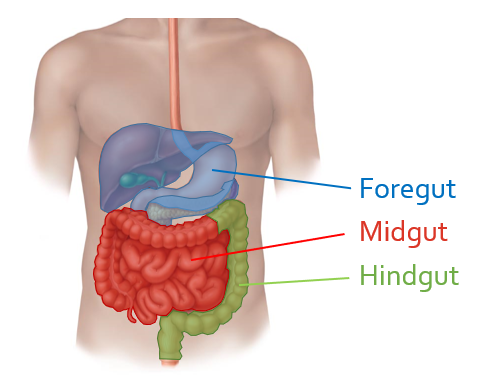
The innervation, blood supply, and lymphatic drainage of the abdominal organs are grouped based on the embryological origin of each organs. To help you understand blood vessel, nerve, and lymphatic distribution to the GI tract and accessory structures, you need to know the derivatives of the primitive gut:
Esophagus (distal part), stomach, duodenum (proximal half), liver, gallbladder, and pancreas (superior portion)
Duodenum (distal half), pancreas (inferior portion), jejunum and ileum, cecum and appendix, ascending colon, right colic flexure, and transverse (proximal 2/3) colon
Transverse colon (distal 1/3), left colic flexure, descending colon, sigmoid colon, rectum, and upper anal canal
Arterial supply
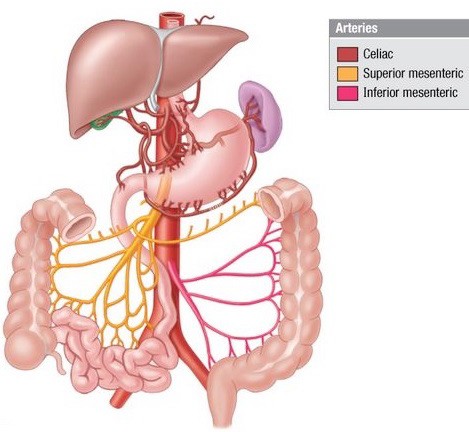
Arteries to all the organs in the abdomen are derived from the abdominal aorta. This is the portion of the descending aorta inferior to the diaphragm. After entering the abdominopelvic cavity via the aortic hiatus in the diaphragm, the abdominal aorta descends anterior to the vertebral column, behind the peritoneum (= retroperitoneal). The abdominal aorta terminates at the level of L-4 vertebra where it bifurcates into left and right common iliac arteries.
Three unpaired arteries arise from the ventral side of the abdominal aorta—these supply the digestive organs derived from the embryonic foregut, midgut and hindgut.
The celiac trunk and its branches supply foregut organs.
Organs in the supracolic region are derived from the foregut, so our focus in this section is on the celiac trunk (we will discuss the superior and inferior mesenteric arteries in detail in the infracolic section). The celiac trunk sprouts from the abdominal aorta immediately after it emerges from the diaphragm, at the level of T-12 vertebra. Although it is somewhat variable, the celiac trunk is very short: three large arteries typically arise from it behind the peritoneum:

- The left gastric artery curls on to the left side of the lesser curvature of the stomach—it passes along the lesser curvature within the lesser omentum, meeting up and anastomosing with the right gastric artery.
- The splenic artery, highly tortuous (twisty), passes to the left along the upper border of the pancreas, behind the peritoneum. It reaches the hilum of the spleen within the splenorenal ligament. It gives off short gastric arteries to the stomach (within the gastrosplenic ligament) and the left gastro-omental artery which passes along the greater curvature of the stomach, within the gastrocolic ligament, where it anastomoses with the right gastro-omental artery.
- The common hepatic artery passes to the right behind the peritoneum. Upon reaching the first part of the duodenum it divides into the gastroduodenal artery and the hepatic
artery proper.-
- The gastroduodenal artery descends behind the duodenum, giving rise to the right gastro-omental artery (passes to the left along the greater curvature of the stomach) and then ending below as the superior pancreaticoduodenal arteries.
- The hepatic artery proper ascends to the liver in the hepatoduodenal ligament, joining the portal vein and common bile duct as part of the portal triad. Upon
reaching the liver, the hepatic artery proper typically divides into right and left hepatic arteries.
• The right gastric artery (sometimes quite small, travels to the left along the lesser curvature of the stomach to meet up with the left gastric artery) has a variable origin—it arises from either the common hepatic artery or hepatic artery proper.
-
Venous drainage
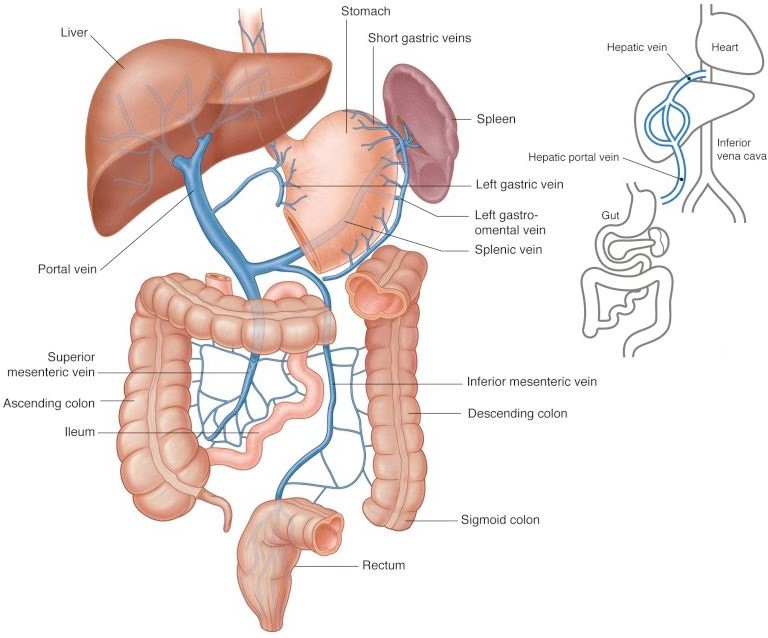
Venous drainage of digestive organs, as well as the spleen, is via the portal vein. The portal vein is formed posterior to the pancreas by the union of the splenic vein and superior mesenteric vein. The inferior mesenteric vein typically is a tributary of the splenic vein. The superior and inferior mesenteric veins drain midgut and hindgut organs, respectively. The splenic vein drains the spleen and parts of the stomach and pancreas. There is no celiac vein. The veins that correspond to arterial branches of the celiac trunk drain directly into the portal vein.
Blood from the portal vein enters the liver for processing, where it percolates through hepatic sinusoids within the liver. From here, venous blood drains into the inferior vena cava via two or three hepatic veins. These enter the IVC just below the diaphragm.
Editor’s note
Don’t make your anatomy instructors sad by confusing the hepatic portal vein and the hepatic veins—they are different vessels!
Note
A portal vein is defined as a vein that lies between two capillary beds. In this case, bed #1 is in the walls of digestive organs and bed #2 is the sinusoids within the liver—the portal vein is situated between these two capillary beds. Do you see this?
Venous blood from non-digestive abdominal organs in the retroperitoneum (e.g., kidney, suprarenal glands) drains into the inferior vena cava, not the portal vein. This blood does not pass through the liver. The IVC is formed by the union of the left and right common iliac veins at the level of L-5. The IVC ascends anterior to the vertebral column, behind the peritoneum, to the right of the abdominal aorta. It leaves the abdominal cavity through an aperture in the diaphragm and immediately enters the right atrium of the heart.
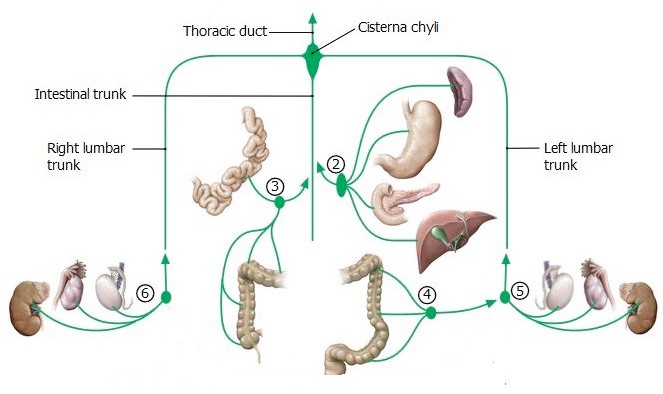
Lymphatic drainage
Lymph from digestive organs (gut) travels in lymphatic vessels that parallel the blood vessels in a retrograde direction toward the abdominal aorta. As it does so, the lymph usually percolates through two sets of lymph nodes.
- Intraperitoneal organs
- central lymph nodes
Distally, peripheral lymph nodes are located adjacent to organs or within mesenteries (e.g., along the mesenteric border of the small intestine).
Proximally, lymph passes through central lymph nodes located near the aorta. These nodes are situated around the major arteries to the gut, and named as such:
-
- Celiac nodes are the central nodes that receive lymph from foregut organs = organs in the supracolic region.
- Superior and inferior mesenteric nodes are the central nodes of the midgut and hindgut, respectively.
Lymph from the central nodes of the foregut and midgut (celiac and superior mesenteric nodes) enters several intestinal lymph trunks. Lymph from the hindgut (inferior mesenteric nodes) drains to the left lumbar lymph trunk, rather than joining the intestinal trunks. Ultimately, the intestinal lymph trunks join the left and right lumbar lymph trunks to form a saccular, dilated structure of variable size behind the abdominal aorta called the cisterna chyli = this is the origin of the thoracic duct. Lumbar lymph trunks receive lymph from the lower limbs, pelvis, kidneys, gonads, and body wall, as well as the hindgut organs.
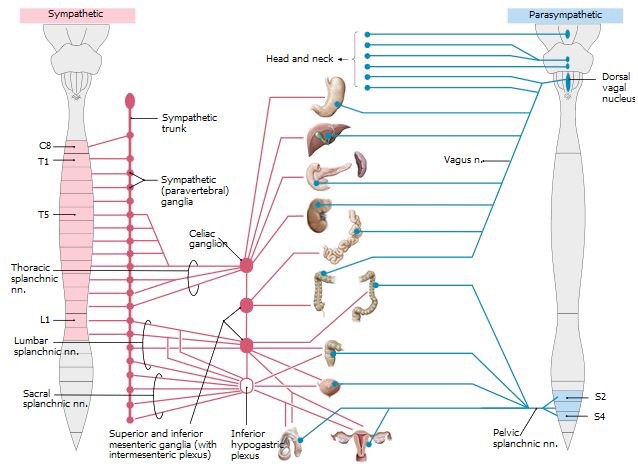
Innervation
Abdominal organs receive autonomic (sympathetic and parasympathetic motor fibers) and visceral afferent nerve supplies. In general, abdominal organs are innervated by both sympathetic and parasympathetic nerve fibers. Autonomic efferent and visceral afferent fibers reach organs through autonomic nerve plexuses = networks of nerve fibers that accompany the blood vessels serving the organs. The major autonomic plexuses are the celiac, superior mesenteric, and inferior mesenteric plexuses. Smaller plexuses branch from these and are named for the blood vessels they associate with. Example: gastric plexus supplies the stomach.
Remember
Autonomic plexuses usually contain three types of fibers: sympathetic, parasympathetic, and visceral afferent nerve fibers.
Nerve fibers reach the foregut via the celiac plexus:
-
- Parasympathetic fibers are from the vagus nerves (via the anterior and posterior vagal trunks). Preganglionic fibers in the vagi synapse on intramural ganglia in or near the walls of target organs.
- Sympathetic fibers to the foregut are from the greater splanchnic nerves. These are typically formed from the union of fibers derived from T-5 to T-9 sympathetic chain ganglia in the thorax. Once formed, the greater splanchnic nerves penetrate the crura of the diaphragm. Preganglionic fibers synapse on postganglionic neuron cell bodies in celiac ganglia. These are classified as prevertebral ganglia, located on the abdominal aorta near the origin of the celiac trunk. Postganglionic sympathetic fibers reach organs of the foregut via autonomic plexuses, where they are mixed with preganglionic parasympathetic and visceral afferent fibers.
-
- Visceral afferent fibers from foregut organs leave through the celiac plexus. Depending on the types of information they carry, they ascend through the greater splanchnic nerves (cell bodies in dorsal root ganglia) or through the vagus nerves (cells bodies in vagal ganglia near the skull).
Nerve fibers reach the midgut via the superior mesenteric plexus (which is a continuation of the celiac plexus):
-
- Parasympathetic fibers vagus nerves. As in the foregut, preganglionic fibers relay on postganglionic cell bodies in intramural ganglia.
-
- Sympathetic fibers Lesser and least splanchnic nerves (branches from T-10 to T-12 sympathetic chain ganglia), with contributions from the greater splanchnic nerves (T-8 and T-9). After penetrating the diaphragm, preganglionic fibers synapse on postganglionic cell bodies in the superior mesenteric ganglia, located along the aorta near the origin of the superior mesenteric artery. Sympathetic, parasympathetic, and visceral afferent fibers reach midgut organs through the superior mesenteric plexus.
-
- Visceral afferent fibers course in the superior mesenteric plexus, then ascend through the greater, lesser, and least splanchnic nerves(cells bodies in dorsal root ganglia) or the vagi (cell bodies in the vagal ganglia).
Sympathetic and visceral afferent fibers reach the hindgut via the inferior mesenteric plexus (parasympathetic fibers take a different route):
-
- Parasympathetic fibers derived from the pelvic splanchnic nerves. These are branches of the ventral rami of spinal nerves S-2, S-3, and S-4. Pelvic splanchnic nerves contain preganglionic parasympathetic fibers. To reach the descending colon and sigmoid colon, they ascend from the pelvic cavity along the superior rectal artery and marginal artery. Preganglionic fibers relay on postganglionic cell bodies in intramural ganglia in or near the walls of the colon and rectum.
- Sympathetic fibers mainly from the lumbar splanchnic nerves. These are medial branches of upper lumbar sympathetic chainganglia, derived from L-1 and L-2 levels of the spinal cord. Preganglionic fibers in lumbar splanchnic nerves synapse on postganglionic cell bodies in inferior mesenteric ganglia, located near the origin of the artery of the same name. Postganglionic sympathetic fibers reach hindgut organs via the inferior mesenteric plexus of nerves.
- Visceral afferent fibers afferent fibers from the descending colon down to the mid-sigmoid colon (above the pelvic pain line) course in the inferior mesenteric plexus, and then enter the lumbar splanchnic nerves. Cell bodies are in upper lumbar dorsal root ganglia. Afferent fibers from the mid-sigmoid colon and rectum (below pelvic pain line) travel in pelvic splanchnic nerves. Cell bodies are in S-2 to S-4 dorsal root ganglia.
Effects of autonomic innervation
Visceral afferent nerve fibers and referred pain from gut organs
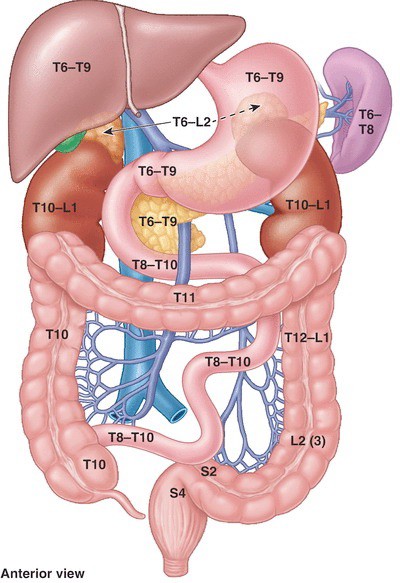
Recall from discussions in Principles of the Autonomic Nerve System (ANS) that visceral afferent fibers carrying pain from internal organs travel along sympathetic innervation routes in a reverse direction (ascend along splanchnic nerves to sympathetic chain ganglia, then pass through white rami communicantes to spinal nerves). Cell bodies of these sensory neurons are in the dorsal root ganglia of spinal nerves. Their central processes enter the dorsal side of the spinal cord through dorsal roots and synapse within the spinal cord on interneurons in the dorsal horns of grey matter.
Visceral afferents from different parts of the gut enter the spinal cord at different levels. Visceral afferents from the foregut enter the spinal cord at T-5 to T-9 spinal cord levels. Those from the midgut enter at T-8 to T-12 and those from the hindgut enter L-1 and L-2 cord segments.
Keep in mind that somatic sensory neurons from the skin also enter the spinal cord through dorsal roots and have their cell bodies in the same dorsal root ganglia as do visceral afferent neurons. Once in the spinal cord, visceral afferent and somatic afferent pathways ascend to the brain, using the same pools of interneurons. Pain from an internal organ therefore may be interpreted by the brain as coming from skin dermatomes. This is the concept of “referred pain”: pain originating from an internal organ manifesting as a dull ache in the body wall. Pain referred from the three parts of the gut tube have characteristic regions of the body wall (dermatomes) where they are perceived:
There is overlap and variation in the distribution of sympathetic nerve fibers from the greater, lesser, least, and lumbar splanchnic nerves—not surprising. Thus, there is probably overlap in the dermatomes involved in referred pain from gut organs.
Clinical correlation
Referred pain occurs early on in an inflammatory state, when the wall of the organ and the visceral peritoneum are involved and become distended. Later, if the infection spreads to parietal peritoneum on the body wall adjacent to the organ, pain will become sharp and more precisely localized. For example, pain from early appendicitis manifests as a dull ache around the umbilicus; if the infection spreads to the body wall, pain is localized in the right lower quadrant, adjacent to the inflamed appendix.