Learn the teaching philosophy behind the Transition to Clerkship on the Overview page
Thank you for serving as a preceptor for our Transition to Clerkship!
You will be working with our second-year medical students, who will soon be transitioning to their third year (where their learning will be primarily in the clinical space during our Longitudinal Integrated Clerkship).
Thank you for serving as a preceptor for our Transition to Clerkship!
You will be working with our second-year medical students, who will soon be transitioning to their third year (where their learning will be primarily in the clinical space during our Longitudinal Integrated Clerkship).
Please do
- Please RSVP and accept the Outlook invitation that we sent. This confirms your participation.
- Please arrive on time so you can be ready to meet your students in the hallway before the encounter begins. The encounters start at the top of the hour, but prior to entering the room, students will practice greeting you and asking for feedback.
- Please pay attention to the time. There will be a group of students arriving at the VCC every hour. It is important to pay attention to the overhead announcements so that each student receives a comparable amount of time with the patient and feedback.
- If you have an emergency on the day of your commitment:
- During business hours: Call the Virtual Clinical Center (VCC) at (509) 368-6910.
- Before or after business hours: Email both Kimberly Beine and Chris Martin.
Quick details for standardized preceptors
- You will receive an email with details about your patient one week prior to your scheduled day. It will include your Workplace-Based Assessment (WBA).
- You will be in the examination room with two students and a standardized patient (representing one of the students' patients).
- The encounter must be completed in 40 minutes.
-
-
- The standardized patient (SP) will give feedback for up to 5 minutes and then will leave the room.
- You will stay in the room and debrief with the students for 10 minutes, including filling out a workplace-based assessment (WBA) if the student requested this. (The student can decide to prompt a 1A or 1B WBA.)
- The student will provide the form on an iPad.
- When the SP returns to the room, you need to step out and greet your next two students (or allow the next preceptor to greet the students).
-
- Sessions may be recorded or viewed remotely for training and quality assurance purposes.
- Your room assignments will be posted at the front desk.
- Where will this educational activity occur?
The Virtual Clinical Center (VCC)
 The Virtual Clinical Center is the central point for all simulation-based training at the at the Elson S. Floyd College of Medicine. The center boasts 10 clinical exam rooms, two high-fidelity simulation suites, a classroom for skills-based instruction, a conference room to support video debriefing, and lab space for the creation of low-cost tissue models in-house.
The Virtual Clinical Center is the central point for all simulation-based training at the at the Elson S. Floyd College of Medicine. The center boasts 10 clinical exam rooms, two high-fidelity simulation suites, a classroom for skills-based instruction, a conference room to support video debriefing, and lab space for the creation of low-cost tissue models in-house.
 The curriculum supported by the VCC encompasses all aspects and modalities of health care simulation. These include partial-task trainers for teaching basic physical exam or clinical procedural skills, manikin-based simulators to allow learners to experience the pressures of caring for a patient in an acute-care setting, and RQI system and computer-based virtual reality simulations for the purposes of exploring emergent technologies and their application in educating the physicians of tomorrow.
The curriculum supported by the VCC encompasses all aspects and modalities of health care simulation. These include partial-task trainers for teaching basic physical exam or clinical procedural skills, manikin-based simulators to allow learners to experience the pressures of caring for a patient in an acute-care setting, and RQI system and computer-based virtual reality simulations for the purposes of exploring emergent technologies and their application in educating the physicians of tomorrow.
Standardized Patients
The Elson S. Floyd College of Medicine also uses Standardized Patient Simulation, which involves individuals playing the role of a patient. These standardized patient encounters assist in the development and assessment of humanistic and clinical reasoning skills.
Standardized patient simulation involves the use of individuals trained to portray the roles of patients, family members or others. A Standardized Patient (SP) is an individual who is carefully recruited and trained to portray or simulate all aspects of a real patient as part of a case scenario in order to provide an opportunity for a student to learn or be evaluated on their clinical skills in a simulated environment. SP’s learn all aspects of a patient portrayal and are carefully trained to not only simulate a real patient scenario but also provides feedback to the students, especially in regard to their communication and interpersonal skills.
Working with a standardized patient (sp)
Please take a few minutes to introduce yourself to the standardized patient (SP), your partner in this educational experience. Please share with the SP about your precepting style. Do you like to correct student actions as they occur, or do you prefer to wait until the debrief? This will make staying in character easier for the SP. When the student arrives, you will each play your standardized part in the encounter.
You may know your standardized patient. Please do not divulge this information to your students! We try very hard to ensure that our students treat our patient actors no differently than they would a patient in the clinical setting.
Our patients are highly trained to provide feedback surrounding the encounter from the patient’s perspective such as eye contact, clarity in asking questions, jargon, empathy, and rapport building. They are instructed to only provide feedback in this area.
Please bring any standardized patient or VCC concerns to the director of Simulation-Based Training, Chris Martin.
Learning Goals for Students in the Virtual Clinical Center
-
-
- Learn how to ask for feedback.
- Practice and demonstrate history and physical exam, incorporating feedback in the moment.
- Practice and demonstrate clinical skills in front of peers and preceptors.
-
How the sessions will work
(Each encounter: 40 minutes total)
- Students will work in pairs (when there is an absence, you may have one student) for this patient encounter with a ‘preceptor’ (you) in the room.
- Prior to entering the room, students will decide which student will take the history and which one will perform the physical (and which one will provide the counseling on May 13, 2025).
- Each student should ask you for specific feedback on something they are working on. They may ask you to fill out a workplace-based assessment (WBA) on their iPad.
- One student will begin the interview with the standardized patient (SP). The second student will perform the physical exam. It is fine if students participate in each other’s tasks if time allows.
- At the end of the encounter, if time allows, you may want to demonstrate some of the skills that might need improvement in the students.
- Students record their findings to take back to the next CBL session or to document the encounter.
- Practice asking the preceptor before entering the room for feedback on practicing history-taking skills, physical exam skills, or patient-counseling skills.
- Practice the clinical skills (patient care, professionalism, interpersonal, and communication) developed since the beginning of medical school.
- Pay attention to good time management.
- One student will take the history, and the other will perform the physical exam. On May 13, 2025, one student will provide contraceptive counseling to the patient.
We expect students to:
-
- Come prepared! Students are instructed to arrive at the VCC with a structured plan for the H&P.
- Arrive in the VCC 10 minutes before their assigned time with the SP.
- Decide who will obtain the history and who will perform the exam.
- Conduct the appropriate history and physical exam, anticipating feedback from you.
- Ask you, the preceptor, for direct observation and feedback on their interview skills or physical exam skills; students must request 2 workplace-based assessments (WBAs) over three weeks of this course.
- Incorporate your feedback into a learning plan to support improved skill demonstration over the 5 weeks of this course.
- Watch, listen, take notes as needed (simulate a preceptor in the clerkship).
- Provide specific feedback on missed history information and review physical examination techniques as needed.
- Invite the standardized patient to provide feedback at the conclusion of the H&P.
- Provide verbal feedback to students designed to help them prepare for learning in the clinical environment.
- Fill out a WBA on the student’s iPad if the student asked for that feedback at the beginning of the encounter.
- The student’s role during the encounter
- Your role as the standardized preceptor
- Practice asking the preceptor before entering the room for feedback on practicing history-taking skills, physical exam skills, or patient-counseling skills.
- Practice the clinical skills (patient care, professionalism, interpersonal, and communication) developed since the beginning of medical school.
- Pay attention to good time management.
- One student will take the history, and the other will perform the physical exam. On May 13, 2025, one student will provide contraceptive counseling to the patient.
We expect students to:
-
- Come prepared! Students are instructed to arrive at the VCC with a structured plan for the H&P.
- Arrive in the VCC 10 minutes before their assigned time with the SP.
- Decide who will obtain the history and who will perform the exam.
- Conduct the appropriate history and physical exam, anticipating feedback from you.
- Ask you, the preceptor, for direct observation and feedback on their interview skills or physical exam skills; students must request 2 workplace-based assessments (WBAs) over three weeks of this course.
- Incorporate your feedback into a learning plan to support improved skill demonstration over the 5 weeks of this course.
- Watch, listen, take notes as needed (simulate a preceptor in the clerkship).
- We will provide a clipboard with paper.
- Provide specific feedback on missed history information and review physical examination techniques as needed.
- Was there missed history information?
- Do students need guidance with physical exam techniques? Review these before the patient leaves the exam room.
- Invite the standardized patient to provide feedback at the conclusion of the H&P.
- Provide verbal feedback to students designed to help them prepare for learning in the clinical environment.
- Fill out a WBA on the student’s iPad if the student asked for that feedback at the beginning of the encounter.
Background on the patients
Below are five of the Transition to Clerkship’s patients. Tap on each of them to see the preceptor summary (PDF ). (The PDF will also be included in your Outlook invitation.)
Tips for providing feedback in real time in the exam room
-
Remind students you are there to observe and provide feedback to help their developmental preparation for the Longitudinal Integrated Clerkship starting in July.
-
Let students know you may interrupt them (if that is your style).
-
If you notice that students are omitting parts of the history that might be important in the case, you might say:
“Let me suggest you explore that symptom a bit further.”
or
“I noticed the patient mentioned [symptom, such as constipation]. It’s a good idea to explore what the patient means by that.”
or
“I noticed the patient seems confused by your question. How might you re-frame it or check for understanding to see if you’ve explored that symptom well enough?” -
Help students with physical examination skills using proper technique.
After observing the student who performs the physical examination, feel free to demonstrate to both students physical exam techniques that may need improvement and allow them to practice, as time allows.
Framework for simulated encounters
We believe that everyone participating in activites at the Virtual Clinical Center is intelligent, capable, and cares about doing their best and wants to improve.
Simulation is an opportunity for learners to discover and experience interpersonal risk-taking relationships in a safe and harm-reductive strategy/space to empower critical thinking concepts.
We acknowledge the technology we use has limitations. We have done everything in our power to provide a valuable learning experience for you. We ask that you meet us halfway and act as if you were in the clinical environment.
- The basic assumption
- Psychological safety
- Realism
We believe that everyone participating in activities at the Virtual Clinical Center is intelligent, capable, and cares about doing their best and wants to improve.
Simulation is an opportunity for learners to discover and experience interpersonal risk-taking relationships in a safe and harm-reductive strategy/space to empower critical thinking concepts.
We acknowledge the technology we use has limitations. We have done everything in our power to provide a valuable learning experience for you. We ask that you meet us halfway and act as if you were in the clinical environment.
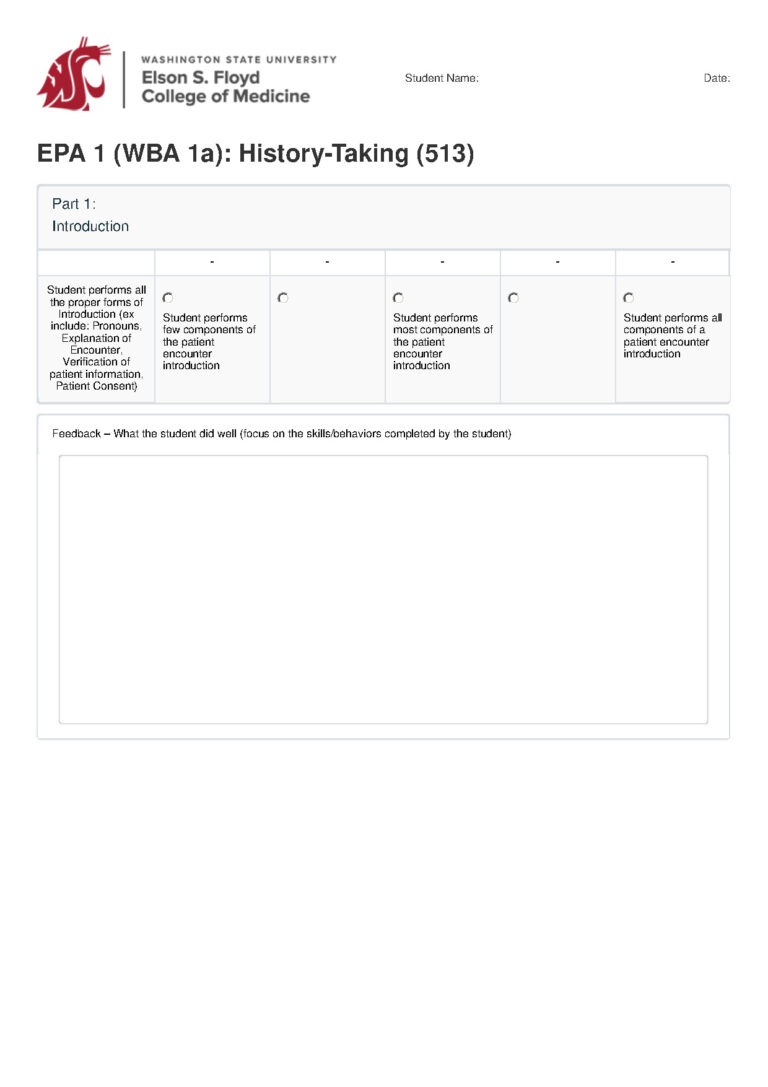
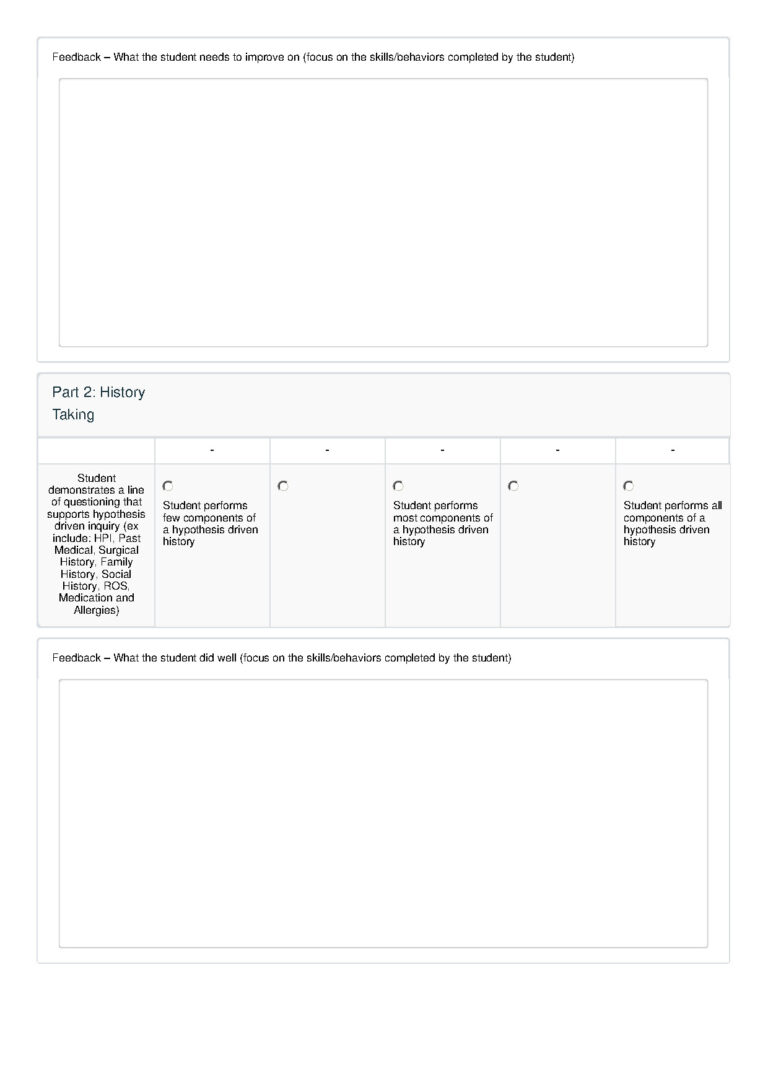
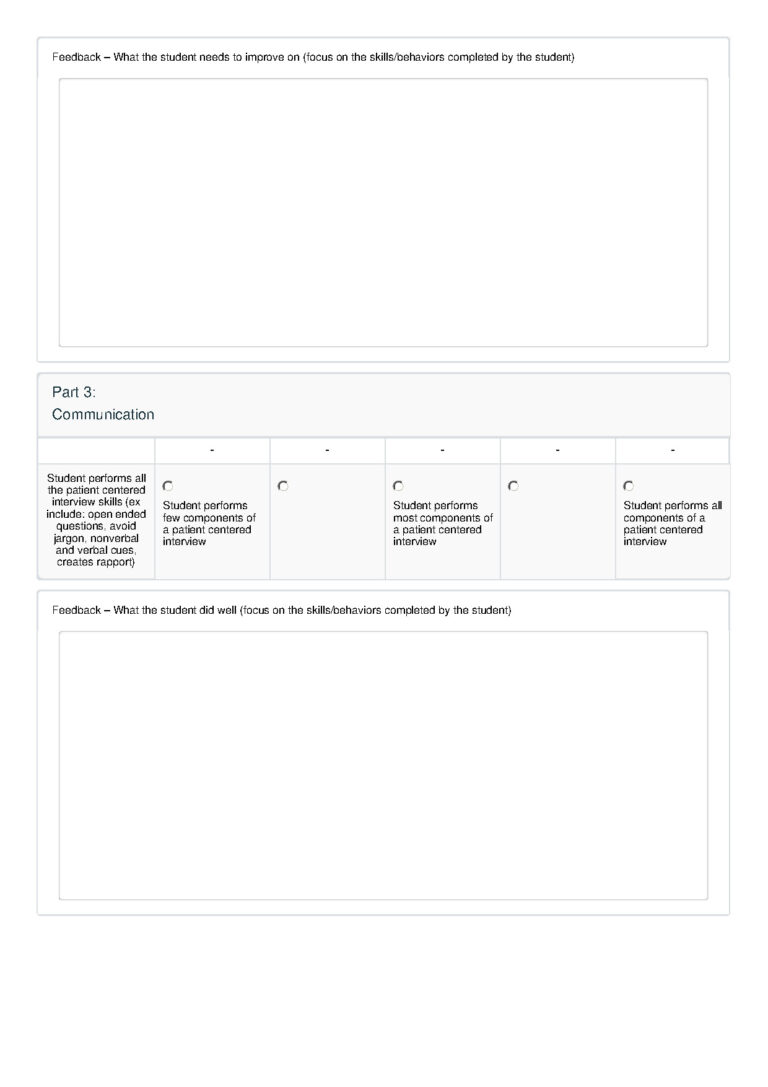
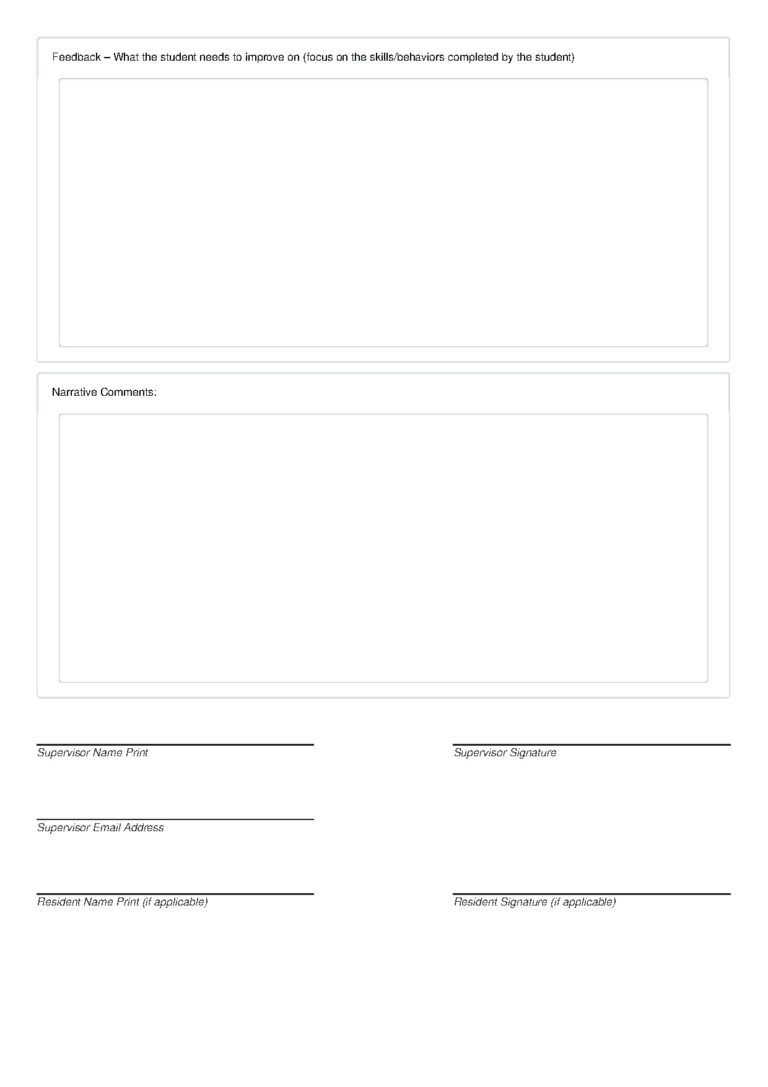
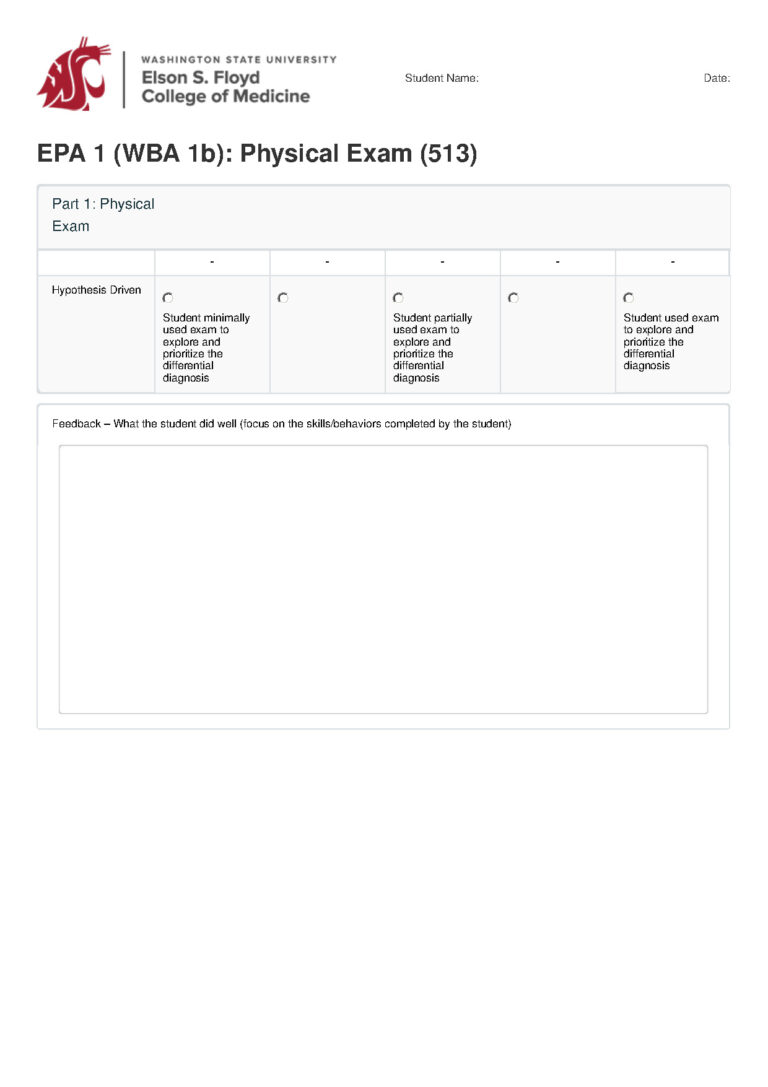
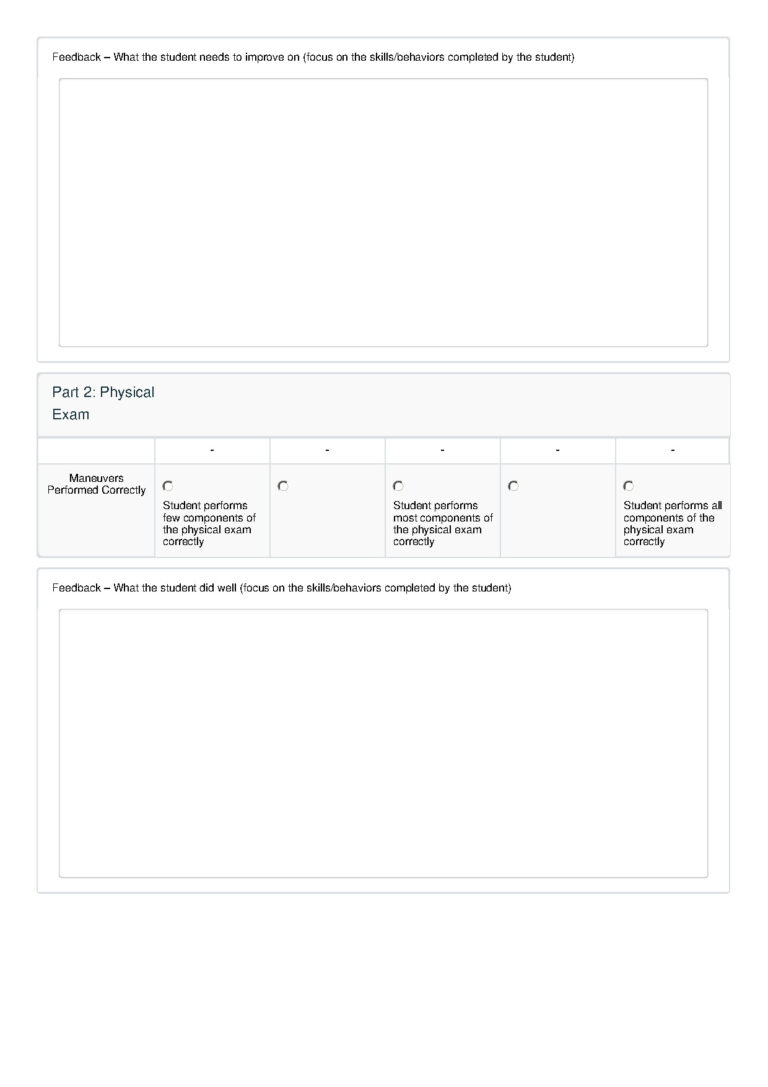
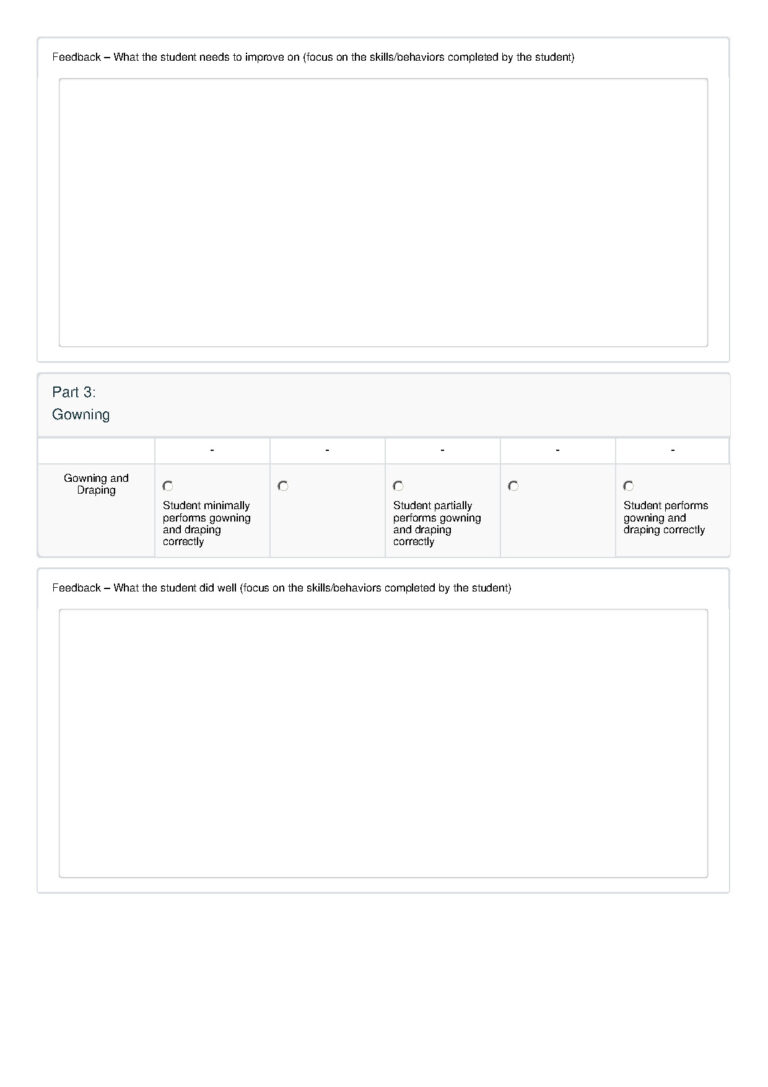
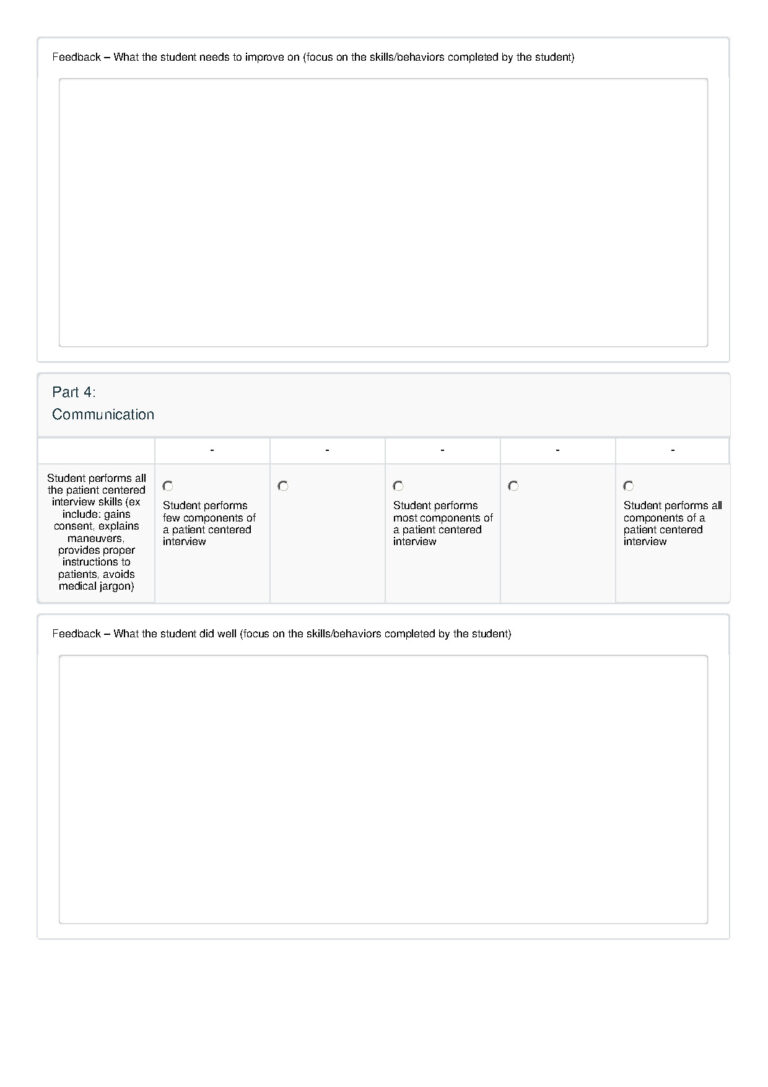
Workplace-Based Assessments (WBAs)
Please review the metrics of the Workplace-Based Assessments so that you are aware of what to look for when assessing students in the VCC.
1a
1b
Student orientation materials: Welcome to Wesford
This is an introduction to Wesford, our fictional Transition to Clerkship city.
-
 Wesford’s healthcare team
Wesford’s healthcare team
- Family Physicians: Hamad Khan, Stephanie Lambert
- Internists: Lauren Hall, Eric Chan
- Hospitalists: Mariana Sanchez (FM), Richard Burnham (FM), Keisha Jones (IM), Dakota Ferguson (IM)
- EM Physicians: Lilly Krieger, Karl Harrison
- Radiologist: Eric Ng
- General Surgeons: Stephen Dieters, Leslie Romero
- Anesthesiologist: Jeff Flett
- Nurse Anesthetist: Karen Lee
- ICU Nurses: Kelly Anne Larsen, Chris Takala
- Pharmacist: Esther Chege
- Registered Dietitian: Keith Somers
- Hospital RN Care Manager: Abbie Edwards
The following specialists are available for remote consult, occasionally take shifts in Wesford, and will care for transferred patients from Wesford during your rotation:
-
- Cardiologist: Sam Watson
- Interventional Cardiologist: Christine Zhu
- Pulmonologist: Elizabeth Chaterjee
- Nephrologist: Adam Ryerson
- Endocrinologist: An Nguyen
- Obstetrician/Gynecologist: Amber Sawyer
- Neurologist: Sofia Rudenko
- Gastroenterologist: Scott Johnson
- Pediatrician: Maria Guzman
- Infectious Disease Specialist: Lee Park
- Pathologist: Natalie Odenkirk
- Psychiatrist: Sam Horace
Thank you! We are grateful for your expertise. We trust that variability among different preceptors will make the experience rich and realistic for students.
Thank you! We are grateful for your expertise. We trust that variability among different preceptors will make the experience rich and realistic for students.