-
Learning objectives
After completing this session, learners will be able to do the following:
-
- Describe the impact of AMR on individuals, society, health systems, and global health goals
- Identify key international responses to AMR
Impact on individuals: Increased mortality
Based on what we have seen so far in the course, you might find it easy to conclude that AMR has drastic implications for patients in terms of their health outcomes; however, it also has potentially devastating financial, social, and psychological effects.
Patients who are infected with pathogens that are resistant to standard treatments typically require more complicated treatment, take longer to recover, and are more likely suffer treatment failure and death (see figure below).
Comparative data on death rates: Drug-sensitive versus drug-resistant bacteria
*K. pneumoniae resistant strain: Carbapenem-resistant Klebsella pneumoniae (CRKP)
**S. aureus resistant strain: Methicillin-resistant Staphylococcus aureus (MRSA)
Sources
ReAct 2012; President's Council of Advisors on Science and Technology 2014
Highlight
A 10-hospital study from India analyzed results from antimicrobial susceptibility testing for Enterococcus spp., E. coli, S. aureus, K. pneumoniae, A. baumannii, P. aeruginosa, and Enterobacter spp. The 5,103 patient samples showed a significant relationship between multidrug resistance (MDR) and mortality: patients with MDR or extremely drug- resistant (XDR) E. coli, XDR K. pneumoniae, and MDR A. baumannii infections had two to three times higher mortality.
Source: Gandra S et al. 2019.
Now we will dive into specific impacts we have not discussed yet.
Impact on individuals: Financial and psychological consequences
Drug resistance results in increased costs to patients for several reasons, including:




Patients with AMR-related illnesses may miss work for longer periods, which results in loss of productivity and income.
Managing drug-resistant infections may bring catastrophic financial hardship to patients and their families and can prevent people from ever seeking care. AMR therefore represents a significant barrier to achieving the Sustainable Development Goals and universal health coverage. Drug-resistant infections may also increase anxiety and have other psychological effects on patients and their families. Stigma around certain diseases, such as HIV or TB, may also affect a patient’s ability to seek care or remain adherent to their treatment regimens, which can further exacerbate poor health outcomes. Long-term treatment regimens, especially those with medicines that may cause side effects, can have drastic psychological implications that may also negatively influence health outcomes.
Sources
Van der Heijden M et al. 2019.
Glossary term
Highlight
A study of 220 patients in a hospital in India showed notable differences in experience for patients who had drug-resistant sepsis vs. those that had drug-susceptible sepsis. The total median cost difference was $700, representing approximately 442 days of wages of a rural male casual worker in India. Further, the antibiotic cost difference was $139 and pharmacy cost difference was $358. The differences in health consequences were also significant: admission to the intensive care unit—44% vs. 21%; complications—56% vs. 37%; length of stay—14 vs. 11 days; and mortality—12% vs. 2%.
Source: Chandy SJ et al. 2014.
Impact on health systems and societies: Increased mortality and cost
The negative effects of AMR are not borne by patients alone, but also by health systems. Societal impacts may also result, as patients with prolonged drug-resistant infections may inadvertently put family and other community members at risk of illness, not to mention the long-term effects due to loss of productivity and increased morbidity.
-
Mortality
Globally, the current estimated number of deaths due to drug-resistant infections is already approximately 700,000 each year. This figure is likely to reach as high as 10 million per year by 2050 if AMR remains unchecked.
-
Costs
AMR also imposes enormous financial burdens on society as a whole from increased morbidity and mortality, but also as a result of longer hospital stays, more expensive treatment, and personal financial losses. AMR costs the US health system $20 billion per year. Globally, it is estimated that $5.8 trillion is lost annually in productivity. Some estimates indicate that, if left unchecked, AMR may lead to a cumulative global cost of $100 trillion by the year 2050 and thrust an additional 24 million people into extreme poverty by 2030—mainly individuals living in low-income countries.
Sources
CDC 2019; Review on Antimicrobial Resistance 2016; World Bank 2017.
The potential for catastrophic effects
The consequences of antimicrobial resistance already discussed in this course are just part of the issue.
AMR has clear implications for medical advances that rely on antibiotics to prevent infections, including complex surgeries, cancer treatment, and organ transplantation. These advanced procedures could become increasingly risky or infeasible, which would increase morbidity and mortality around the world.
If a particular AMR strain were to reach pandemic levels, food shortages could occur due to untreatable infections in farm animals and restrictions could be imposed on travel, migration, and trade. Such scenarios could lead to serious market failures, challenges in global governance, and huge social impacts. Low-income countries would suffer the most, resulting in greater income inequality. The World Bank estimated that the global economic losses would rival those of the 2008–2009 global financial losses, but last for many more years.
Of additional concern is the potential for existing drug-resistant bacteria (or bacteria engineered with resistant genes) to be intentionally released as a weapon.
Creating a world safe and secure from infectious disease threats was the impetus behind the 2014 launch of the Global Health Security Agenda. The agenda outlines 19 areas of action and leverages country commitments and cooperation to advance long-term global health security. AMR is one of the 19 technical areas.
Sources
Van der Heijden M et al. 2019; World Bank 2017.
AMR: A challenge to achieving the SDGs
Adopted by all UN Member States in 2015, the 17 Sustainable Development Goals (SDGs) are a call to improve the lives of everyone, everywhere by 2030. The goals cover a range of issues from poverty to health, to the environment.
There is a direct connection between AMR and achieving SDG 3—Good Health and Well-being. However, because many of the SDGs are intertwined, lack of progress on SDG 3, also affects others. For example, without good health of the family provider, the entire family is more likely to go hungry. Without AMR containment, SDGs 1, 2, 3, 8, and 10, among others, are likely not achievable.
Sources
IISD/SDG Knowledge Hub 2019; United Nations N.D.; van der Heijden M et al. 2019.
Glossary term
AMR: A challenge to achieving UHC
Under universal health coverage (UHC), everyone receives the health services they need without financial hardship.
Sustainable Development Goal 3 targets achieving universal health coverage, including:
Financial risk protection
Access to quality essential health care services
Access to safe, effective, quality, and affordable essential medicines and vaccines for all
AMR makes it more difficult for countries to provide UHC by:
-
Making first- and second-line antimicrobials ineffective,
affecting supply chains, access, and treatment efficacy
-
Diverting scarce health system resources,
affecting supply chain and affordability of treatment and health services
-
Translating into expensive treatment,
affecting affordability and causing financial hardship
-
Making treatment difficult and complex,
affecting health service quality and treatment effectiveness
Although many think of UHC primarily as a health financing issue that if achieved would provide access to essential health services, the service quality is also of utmost importance as is the inclusion of medical products in the basic package of care provided under UHC. The complex dynamics and relationships at play require a systems approach to achieve UHC and to contain AMR. There is growing international effort to use the momentum behind UHC efforts to simultaneously address AMR.
Sources
ReAct 2019; Tayler E. et al. 2019; Joshi MP 2016; WHO. 2019h; WHO 2020e.
Highlight
The first national TB patient cost survey carried out in Lao People’s Democratic Republic in 2018–2019 showed that 86.7% of people with drug-resistant TB faced catastrophic costs (>20% of household annual income) compared with 62.2% of people with drug-susceptible TB.
Source: Chittamany P. et al. 2020.
The World Health Organization’s response to AMR
Recognizing the potentially grave impact of AMR on global health outcomes, the World Health Organization (WHO) has taken several steps toward catalyzing coordinated global action toward the containment of AMR.
In 2015, following the World Health Assembly, the WHO adopted a global action plan to help address, build awareness, and promote coordinated global action to keep AMR from eroding the progress of modern medicine.
Part 2 of this course lists the objectives of the WHO Global Action Plan and some of the key actions to meet those objectives.
The chart below provides a chronology of the major actions WHO and the tripartite—WHO, Food and Agriculture Organization (FAO), and World Organsiation for Animal Health (OIE)—have taken to fight AMR, along with links to each respective document.
|
Year |
Select WHO Responses to AMR |
|
2015 |
|
|
2016 |
Antimicrobial resistance: A manual for developing national action plans |
|
2017 |
|
|
2019 |
|
|
2019 |
|
|
2015–2020 |
|
|
2017–2019 |
|
|
2019–2020 |
Tripartite AMR Country Self-assessment Survey (TrACSS) Global Analysis Report |
|
2020 |
The One Health Global Leaders Group on Antimicrobial Resistance |
|
2014–2021 |
|
|
2021 |
Tripartite AMR Country Self-assessment Survey (TrACSS) 2021 data |
One health approach to AMR
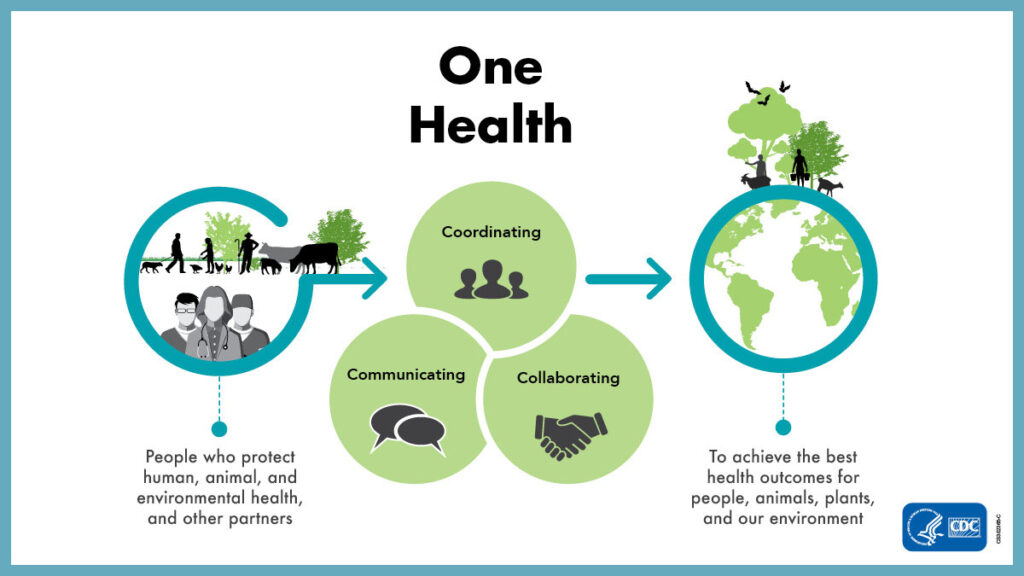
Because the drivers of AMR come from humans, animals, plants, and the environment and are intertwined, controlling AMR requires coordination among these sectors. For example, misuse and overuse of antimicrobials not just in humans, but also in animal husbandry, agriculture, and aquaculture, can lead to resistant microbes circulating among these various sectors, including the environment. Being a multifaceted and multifactorial issue, AMR requires a coordinated and concerted approach.
Previous efforts to combat AMR were highly siloed with little collaboration between players and sectors. One Health is the concept of multisectoral coordination to ensure optimal health for people, domestic animals, wildlife, plants, and our environment. In the context of One Health, the Food and Agriculture Organization (FAO), the World Organisation for Animal Health (OIE), and the World Health Organization (WHO) committed to support governments; health care workers; veterinary, plant, and environmental professionals; and other stakeholders to promote multisectoral activities to contain AMR.
Examples of One Health actions include the following:






For example, many countries now have multisectoral coordination bodies on AMR that include members from various sectors, including the human, animal, and environmental sectors. The main objective of these bodies is to help implement their national action plans on AMR through multisectoral meetings, reviews, collaborations, and actions.
Sources
Alas M 2020; Collingnon PJ and McEwen SA 2019; Interagency Coordination Group on Antimicrobial Resistance 2019; Joshi MP et al. 2021.
Glossary term
National action plans on AMR
As of January 2021, 143 countries had finalized national plans to help combat AMR and 43 were in the process.
Côte d’Ivoire launched its national action plan (2019-2020) with an accompanying AMR policy and governance manual. The action plan for the U.S. National Strategy for Combating Antibiotic-Resistant Bacteria has been updated for 2020-2025. It takes a One Health approach and expands activities that have proven effective in combating AMR such as infection prevention and control and antimicrobial usage.
Sources
WHO 2021a.
The global health security agenda
Launched in 2014, the Global Health Security Agenda (GHSA) is a partnership of more than 70 nations, international organizations, and non-governmental stakeholders and private sector entities to strengthen the world’s ability to prevent, detect, and respond to infectious disease threats. The GHSA includes 19 technical areas or action packages, including one specifically focused on addressing antimicrobial resistance.
The AMR Action Package of GHSA seeks to support the WHO Global Action Plan on AMR by building country capacity related to multisectoral coordination, AMR surveillance, infection prevention and control, and antimicrobial stewardship in human and animal sectors, and maintaining AMR as a priority on political agendas.
The GHSA 2024 target is to strengthen 100 countries to a level of “Demonstrated Capacity” in at least five technical areas as measured by relevant health security assessments, such as the WHO’s Joint External Evaluation (JEE) tool.
Sources
Source: GHSA 2018.
WHO Joint External Evaluation (JEE) tool
The WHO developed the International Health Regulations Joint External Evaluation (JEE) tool in 2016 (revised in 2018) to measure progress in all elements of the GHSA assessment. The JEE process is voluntary, collaborative, multisectoral, and transparent and rates country capacity across five levels:
As of November 2020, 113 countries had completed a JEE.
The four indicators of AMR country capacity in the JEE tool are:
Sources
WHO 2018; CDC 2020a; de la Rocque 2021
Highlight
In its 2017 JEE, Kenya scored 2 (“Limited Capacity”) for indicator 3.4 related to antimicrobial stewardship. The evaluators found that Kenya’s national plan for the prevention and containment of AMR had been approved and included antimicrobial stewardship, its national action plan for antimicrobial stewardship was complete, and development of antibiotic use guidelines for veterinary practice was complete.
The evaluators made the following recommendations for Kenya to advance its capacity level score:
-
- There is a need for systematic implementation of existing treatment guidelines.
- There is a need to develop training curriculum for antimicrobial stewardship for pre-service and in-service training to reinforce the provisions for prudent/correct use of antimicrobials at all levels.
- An evaluation of antibiotic use patterns is required.
- There is a need for full implementation of antimicrobial stewardship activities in the human and animal health sector.
Source: WHO 2017c.
WHO benchmark actions
In 2019, WHO published a complementary list of benchmark actions designed to help improve the International Health Regulations capacities. This tool provides recommended actions for each JEE capacity level for the different technical areas, including AMR.
For example, the following are the recommended actions to achieve capacity level 3 for the indicator P.3.1. (multisectoral coordination on AMR):
-
Develop a plan of action to address AMR in line with the Global Action Plan (GAP) on AMR
-
Submit a plan for approval through relevant governance mechanisms
(such as office of head of state, cabinet, or ministries of health and agriculture)
-
Develop terms of reference for a multisectoral governance mechanism,
with clear lines of accountability between the AMR coordinating committee and the high-level One Health group making strategic and resourcing decisions
-
Organize effective coordination through regular meetings
Sources
WHO 2019; Alliance for Health Security Co-operation 2019.
Session summary
As shown in this session, AMR affects not only individuals, but also entire health systems and societies. Moreover, AMR impedes the achievements of key global public health goals such as the Sustainable Development Goals and universal health coverage. AMR’s wide-reaching consequences have elicited major global initiatives aimed at curbing its development and spread, including its inclusion in the Global Health Security Agenda, which is a growing partnership of over 70 countries and other stakeholders.
Part 2 of this course explains, in more detail, the major factors contributing to AMR and the range of interventions that can help contain it.
These materials were adapted from the Global Health eLearning Center, U.S. Agency for International Development.
Image credits
Unless otherwise noted, images are from Adobe Stock.
