Patient 1: Marie
Question
Which of the following examination findings would confirm a diagnosis of brain death?
Cyanosis:
-
While the patient may present with cyanosis, if you were to withdraw mechanical ventilation such as when an apnea challenge is performed, this is not a required finding for a physician to declare brain death.
Loss of corneal reflex (correct answer):
-
In order to declare brain death, the patient must not have any brain stem reflexes present. Other examples of brainstem reflexes include gag reflex and vestibular ocular reflex.
Positive plantar reflex:
-
This is a sign that can be present in the setting of come or disorder of consciousness; however, it is not a key physical exam finding to declare brain death.
Systolic blood pressure less than 100:
-
Again, this patient may have a low SBP due to blood loss. However, in order to declare brain death, the patient has to maintain an SBP>100 is required prior to testing to declare brain death.
Unresponsive to stimuli:
-
While this is also true of a patient who has had brain death, being unarousable is also true of a coma, which is not the same as brain death, and patients in a coma do have a chance at recovery.
Keywords: Disorders of consciousness; brain death
Resources
- Starr, R. Brain death. StatPearls [Updated 2021, Oct 14]. In:StatPearls. Retrieved January 14, 2022.
- NeuroBytes: Medical Student Series: Brain Death: A Case-Based Discussion. American Academy of Neurology. (n.d.). Retrieved January 14, 2022.
Patient 2: Roberta
Question
Which of the following elements in this patient’s history and physical exam suggests the need for imaging now?
Family history:
-
Migraines often run in families and would not be red flag for possible life-threatening cause of migraine.
Lack of response to Sumatriptan:
-
While this could be a sign of new headache patter—which can be a red flag—this is also commonly seen in medication overuse headaches and would not necessarily be enough to warrant imaging the patient immediately.
History of breast cancer (correct answer):
-
With the patient’s past history of an advanced stage breast cancer, it is possible that the cancer has recurred and could possibly have a brain metastasis and would warrant imaging to rule out.
Unilateral distribution of pain:
-
Migraines are often in a unilateral distribution and is not a red flag.
Visual disturbances:
-
Given that the patient’s prior migraines are with aura, this itself isn’t necessarily a red flag, but you should confirm that the visual disturbance is the same as her past migraines.
Keywords: Headache
Resources
- NeuroBytes: Medical Student Series: The Approach to a Patient With Headache. Aan. (n.d.). Retrieved January 14, 2022.
- DeWitt, D., and Coxon, K. (n.d.). Headache and Migraine. Lecture.
- Costello, F. Headache. MEDSKL. (n.d.). Retrieved January 14, 2022.
Patient 3: Dawson
Prior to this incident, he was completely normal. On physical exam, the patient had left visual field deficits and was unable see you when you stood to his left.
Question
Given the patient’s initial history, in arterial territory, where would you expect to find an occlusion?
Right anterior cerebral artery:
- Occlusion in this territory would likely lead to left sided paresis and sensory loss of the lower extremity.
Right posterior cerebral:
- This would present with visual loss and loss of sensation.
Right middle cerebral artery (correct answer):
- This patient is displaying signs of left sided hemineglect, which is consistent with right MCA in most patients, as this is the non-dominant side in 90% of patients.
Right cerebellar:
- Occlusion in this territory would likely cause ataxia and slurred speech.
Right lenticulostriate:
-
A stroke affecting this region would result in purely motor deficits in both upper and lower extremities.
Keywords: Ischemic stroke, cerebral vascular territories
Resources
- Konan LM, Reddy V, Mesfin FB. Neuroanatomy, Cerebral Blood Supply. [Updated 2021 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
- Sarwar A, Emmady PD. Spatial Neglect. [Updated 2021 Aug 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.S
- Le, T. (2019). Neurology. In First aid for the USMLE step 2 CK: Clinical knowledge. essay, McGraw Hill Education.
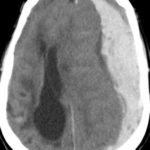
Patient 4: Ivana
Question
What would be the most appropriate management of this patient?
Administer tPA:
- Based on the CT, this patient appears to have suffered an ischemic infarct to the MCA, which you could treat with tPA; however this patient’s last known normal was 10 hours ago, well outside the 4.5-hr window for tPA administration.
Recommend supportive care only:
- This patient has not been fully evaluated, and at this point it would be too premature to withdraw care at this point. If this patient was presenting with a hemorrhagic stroke, supportive care might be an option, as interventions are limited and may not change prognosis.
Administer Heparin:
- There is no current evidence or recommendations that show benefits from urgent anticoagulation.
Goal BP less than 220/120 (correct answer):
- In the case of ischemic stroke, recent evidence suggests that permissive hypertension may improve patient outcomes. Allowing a patient’s BP to rise to 220/120 as long they are not showing any adverse effects from elevated BP is warranted.
Goal BP less than 160/90:
-
See the answer above.
Keywords: Ischemic stroke; stroke management; tPA
Resources
- Gaillard, F., Rahman, F. Middle cerebral artery (MCA) infarct. Reference article, Radiopaedia.org. (accessed on 02 May 2022) https://doi.org/10.53347/rID-1617
- Le, T. (2019). Neurology. In First aid for the USMLE step 2 CK: Clinical knowledge. essay, McGraw Hill Education.
- Konan LM, Reddy V, Mesfin FB. Neuroanatomy, Cerebral Blood Supply. [Updated 2021 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
- Powers, W. J., Rabinstein, A. A., Ackerson, T., et al. (2019). Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals. The American Heart Association/American Stroke Association. Stroke, 50(12).
Patient 5: Davíd
Question
What of the following would indicate that this patient would be a candidate for spinal nerve decompression surgery?
Worsening pain:
-
Pain is never an indication for spinal surgery, as it rarely improves the pain a patient is experiencing. It can, however, improve nerve pain but is not the first-line treatment option for back pain.
Leg paresthesias:
-
This can indicate possible nerve damage, which would indicate the need for surgical nerve decompression, but it can also be a sign of reversible nerve inflammation, and an EMG is needed to evaluate nerve health.
Back pain impacting his daily life:
-
While this is important to appreciate when evaluating the patient and while participating in patient shared decision-making, it is not an indication for spinal surgery.
EMG indicating nerve damage (correct answer):
-
EMG is the best way to evaluate nerve health. Nerve compression that is causing irreversible nerve damage is the best indicator for the necessity of surgical nerve decompression over less invasive options.
MRI confirming stenosis:
-
This can be an indicator of possible future nerve damage, but it would not be enough of an indicator for an invasive surgical option until either confirmation of irreversible nerve damage or less invasive options have been exhausted.
Keywords: Spinal stenosis; EMG; nerve compression
Resources
- Patel, A. M. Lumbar stenosis. PM&R KnowledgeNow. Updated Dec. 15, 2020.
- Saad, A. E. A., Vazzquez-Galliano, J, Chen, Y. Basic Electrodiagnostics for the Referring Physician. PM&R KnowledgeNow. Updated Sep. 28. 2020.
Patient 6: Anika
Question
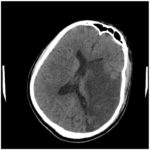
Which of the following is the most likely etiology for the CT findings?
Middle meningeal artery bleed:
- Is consistent with an epidural hematoma.
Bridging veins rupture (correct answer):
- This non-contrast CT head is consistent with subdural hemorrhage. Bridging vein rupture is the most common cause.
Saccular aneurysm rupture:
- Is consistent with a subarachnoid hemorrhage.
Atherosclerotic embolic event:
-
Is consistent with an ischemic stroke.
Patient 7: Kevin
His wife expresses concerns about her husband’s personality changing significantly over the years. She states he used to be reserved and responsible, but now is flamboyant and reckless, especially with their finances. He often lashes out for no reason and makes “a scene.” Last week, he bought a new car without telling anyone. The patient laughs at this and states everyone should be more like him. His wife denies noticing any apparent memory issues, new tremors or rigidity, or changes in speech.
Question
Which of the following is likely to be found on histology of brain tissue?
Ubiquitinated TDP-43 (correct answer):
- This patient likely has frontotemporal dementia with noted grandiose behavioral changes. Ubiquitinated TDP-43 is a common histologic finding.
Alpha-synuclein:
- Is consistent with Lewy bodies in Lewy body dementia.
Senile plaques in gray matter with extracellular beta-amyloid core:
- Is consistent with Alzheimer’s disease.
Spongiform cortex:
- Is consistent with Crutzfeldt-Jakob disease.
Depigmentation of substantia nigra:
- Is consistent with Parkinson disease.
Patient 8: Marina
While doing your exam, you notice the patient’s right eye seems to be displaced medially. When testing extraocular motor movements, the patient is unable to move her right eye away from her nose to look laterally. Her left eye moves normally. The rest of her neurological exam is unremarkable.
Question
Which of the following cranial nerves (CN) corresponds to the likely deficit?
CN 2:
-
CN 2 corresponds to the optic nerve, which assists with vision and the efferent limb of pupil reflex.
CN3:
-
CN 3 corresponds to the oculomotor nerve, which assists in eyelid function, most of the eye muscles movement (superior rectus, inferior rectus, medial rectus, inferior oblique), and the afferent limb of pupil reflex.
CN 4:
-
CN 4 corresponds to the trochlear nerve, which supplies the superior oblique muscle that moves the eyes down/out and inward.
CN 5:
-
CN 5 corresponds to the trigeminal nerve, which assists in facial sensation, taste, jaw movement, and the afferent limb of corneal reflex.
CN 6 (correct answer):
-
This patient has a lateral rectus muscle palsy, likely secondary to microvascular disease. CN 6 (abducens nerve) supplies the lateral rectus muscle.
CN 7:
-
CN 7 corresponds to the facial nerve, which assists in facial expression, taste, and the efferent limb of the corneal reflex.
Patient 9: John Doe
Question
Which of the following is likely to be found on examination?
Right side loss of pain and temperature below the level of injury (correct answer):
-
The patient likely has Brown-Sequard Syndrome from traumatic hemisection spinal cord injury. Below the injury, spinothalamic tract damage is expected on the opposite side as the tracts decussates at the level of the spinal nerve.
Right side loss of proprioception and vibration:
-
You would expect ipsilateral (left) loss of proprioception and vibration below the level of injury due to dorsal spinal column damage. The dorsal spinal column decussates in the medulla.
Left-side Horner syndrome:
-
You would expect ipsilateral Horner syndrome if the lesion were above T1 due to oculosympathetic pathway damage. This patient appears to have a lesion in the lower thoracic region.
Left-side lower motor neuron signs below the injury:
-
You would expect ipsilateral upper motor neuron signs below the level of injury due to corticospinal tract damage. Lower motor neuron signs would be expected at the level of the injury.
Patient 10: Vijay
Question
What is the likely mechanism of action of the patient’s new medication for management of his Parkinson disease, that is resulting in his change in behavior?
Glutamate NMBA antagonist:
-
Amantadine toxicity generally presents with edema, livedo reticularis, ataxia.
Dopamine agonist (correct answer):
-
This patient was likely started on a dopamine agonist, such as pramipexole and ropinirole, which can also be used for restless leg syndrome. Effects can include impulse control disorders.
Dopamine precursor:
-
Levodopa is a dopamine precursor. This medication is generally first line treatment for patients >65. Common effects include wearing off effects, dyskinesia, and psychosis.
Adrenal steroid with mineralocorticoid properties:
-
Fludrocortisone can be used to help manage symptoms of orthostatic hypotension caused by other Parkinson medications. It alone is not a medication for the management of Parkinson.
Image credits
Unless otherwise noted, images are from Adobe Stock.