Case study 3: Frank—I passed out
- Past smoker, quit 5 years ago.
- Brother had an MI at 55.
Question
You should consider:
- Cardiac causes, especially arrhythmias
- Medications that could cause arrhythmia or blood pressure problems (hypotension or orthostatic hypertension)
- Other neurologic causes, such as subarachnoid hemorrhage, stroke, or seizures (reconsider whether cluster headaches is the correct diagnosis).
- Finally, dehydration and cardiac ischemia should always be considered.
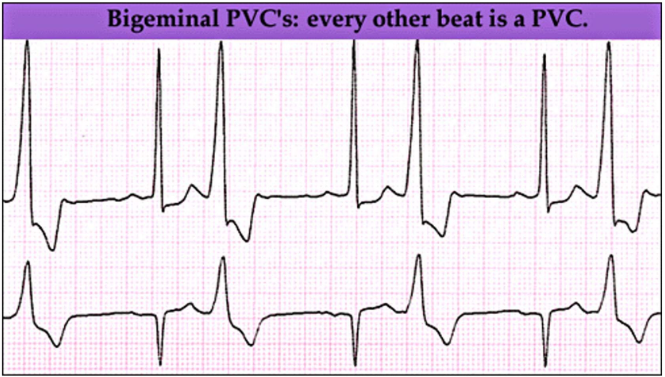
It is important to think about cardiovascular syncope (dizziness) vs vertigo (neurologic cause). Within cardiovascular, consider underlying causes (ischemia and arrhythmias are common and can be deadly), including medication side effects (e.g., antihypertensives or anticholinergics; long QT–inducing medications, etc.). This is likely cardiac syncope secondary to arrhythmia. While infrequent PVCs are usually not an issue, and even bigeminy can be benign, this patient has an arrhythmia and symptoms.
- Medication
- Physical exam
- Echocardiogram
- Ambulatory ECG Monitoring
- Nitroglycerin.
- Aspirin.
- Furosemide.
- Benazepril.
- Metoprolol.
- Amitriptyline.
- Atorvastatin.
- BP 120/72. P 65 with slight irregularity.
- CV: RRR S1S2 with 1/6 SM at LLSB without radiation.
- Chest: CTA.
- Extremities: No cyanosis or oedema.
LV mildly enlarged at 60 mm. Akinesis of the inferior wall and basal 2/3 of the septum. LV function is mildly reduced. LA is 45 mm (mildly enlarged). RV size and function are normal. Trileaflet AoV without AI. Mild mitral and tricuspid regurgitation present. Frequent PVCs noted.
Heart rate avg 79, min 50, max 107. Basic rhythm is sinus with frequent bigeminy (total 7 hours 12 minutes). There were 2443 premature ventricular contractions, more than 200 per hour for 6 hours. There were 25 couplets and no sustained ventricular arrhythmias. The patient experienced dizziness and fatigue while exercising. During this time, the patient had >200 PVCs per hour.
Key points
- Initial Hx + PE + ECG: Diagnosis in 45–69%.
- Mortality is high if the cause is cardiac and not increased if non-cardiac.
- If high risk for CVD and fatal arrhythmias, or falls (e.g. elderly): Hospitalize for evaluation.
- CV eval.
- Echocardiography: Stress testing.
- Loop event recorders (may identify PAF in 16% of patients vs 3% w/ 1–2 days monitoring in hosp/Holter).
- Neurological evaluation.
- Head CT.
- EEG only if abnormal neuro exam or suggestive history.
- Tilt-table testing is useful in further defining neurocardiogenic syncope.
Image credits
Unless otherwise noted, images are from Adobe Stock.