Author
Blake Cohoe, MD
editor
Dawn DeWitt, MC, MSc, MACP, FRACP
Hereditary motor and sensory neuropathy
Question
Hereditary motor-sensory neuropathy (HMSN) primarily affects the peripheral nervous system. Which of the following are features of the most common type of HMSN?
- ALS: Death of both upper and lower motor neurons in the motor cortex of the brain, the brain stem, and the spinal cord leads to muscle twitching and atrophy.
- Refsum’s disease: Impaired oxidation of branched chain fatty acids leads to neurologic damage, cerebellar degeneration, and peripheral neuropathy.
- Dejerine Sottas syndrome: Genetic mutations in axons or myelin protein leads to severe, rapidly progressive neurological damage by adolescence and complete loss of ambulation.
- CMT: Genetic mutations in axons or myelin protein leads to leg muscle atrophy, loss of sensation, and proprioception in early adulthood.
- Parkinson’s: This movement disorder is characterized by degeneration of midbrain neurons.1
Background and basics
- Abnormal peripheral axon or myelin proteins.
- More than 80 mutations have been described:
- Affect Schwann cell membranes, mitochondria, signaling, cell cycle, cytoskeleton, and genetic and protein processing.4
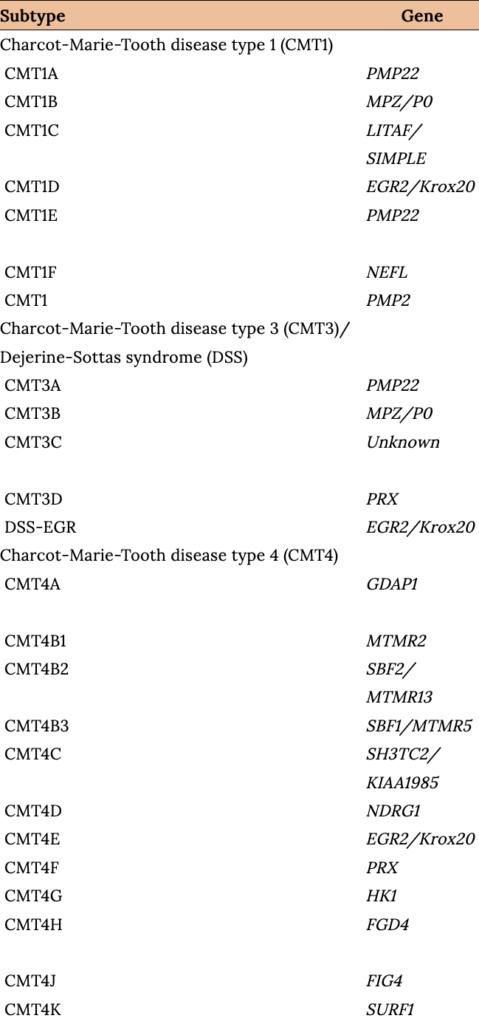
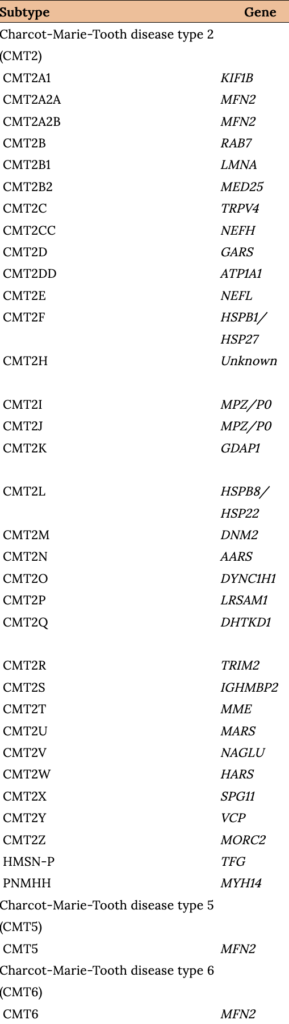
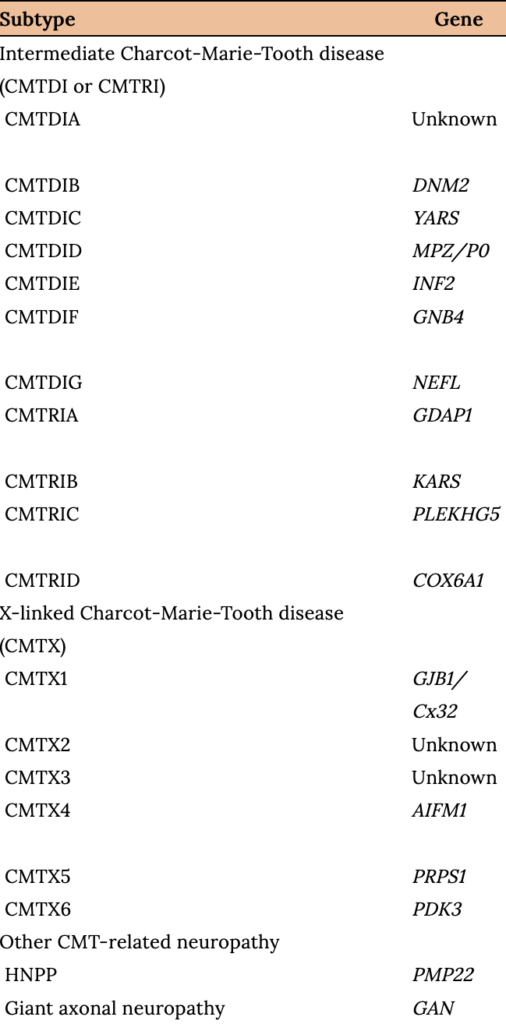
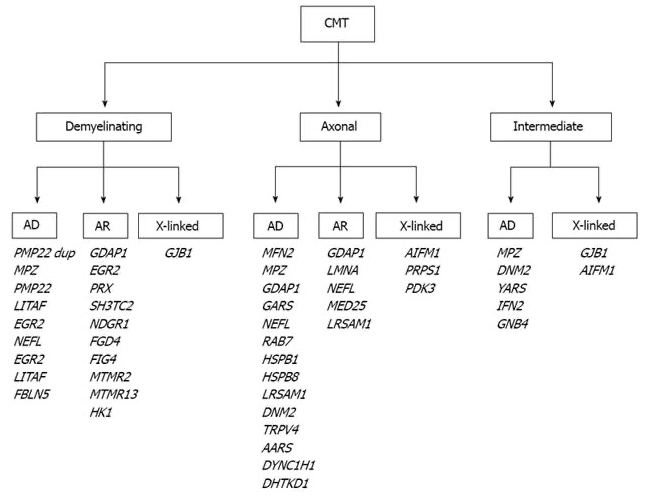
Clinical and genetic aspects of Charcot-Marie-Tooth Disease subtypes: A genetically diverse disease
Nam SH, Choi BO. Clinical and Genetic Aspects of Charcot-Marie-Tooth Disease Subtypes, Tables 1–3.
The most common Charcot-Marie-Tooth (CMT) genetic mutations and their clinical associations
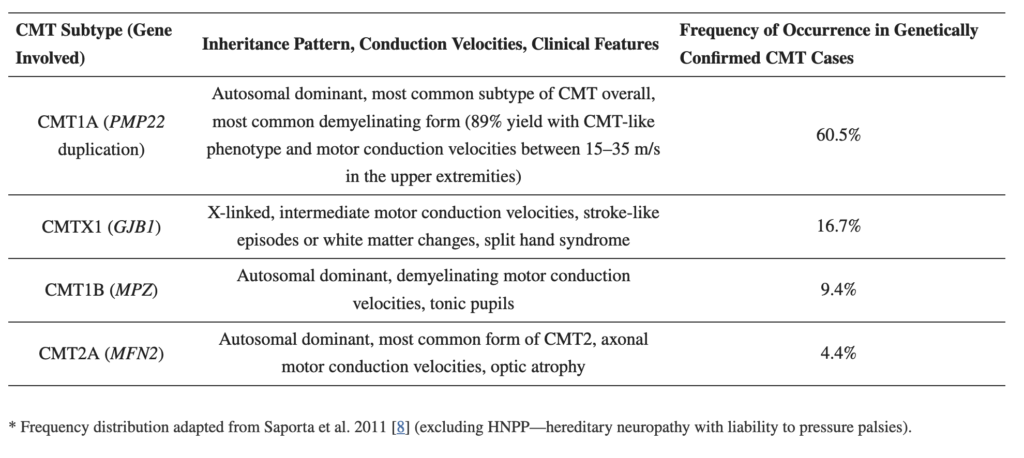
- Classification and Pathophysiology
- There are many ways to classify. The majority of CMT neuropathies are demyelinating, although up to one-third are primary axonal disorders.4
- The three most common types of HMSN are CMT1, CMT2, and CMTX.
- HMSN/CMT Type 1: Demyelinating. Autosomal Dominate
- HSMN/CMT Type 2: Axonal. Autosomal Dominate
- HSMN/CMT Type X: Intermediate motor conduction. X-linked
- Loss of myelin (CMT1) slows nerve conduction. Motor conduction velocity below 35 m/sec in the forearm segment of the median or ulnar nerves is a proposed cutoff value to distinguish CMT1 from CMT2 and CMTX.4
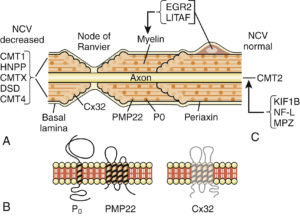
Charcot-Marie-Tooth Disease type 1
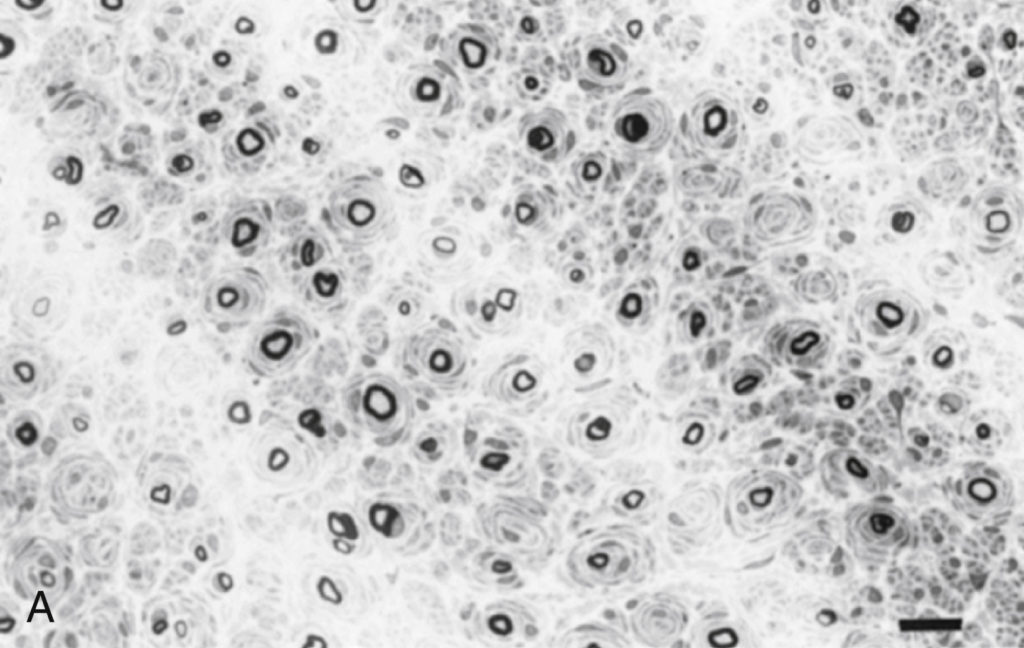
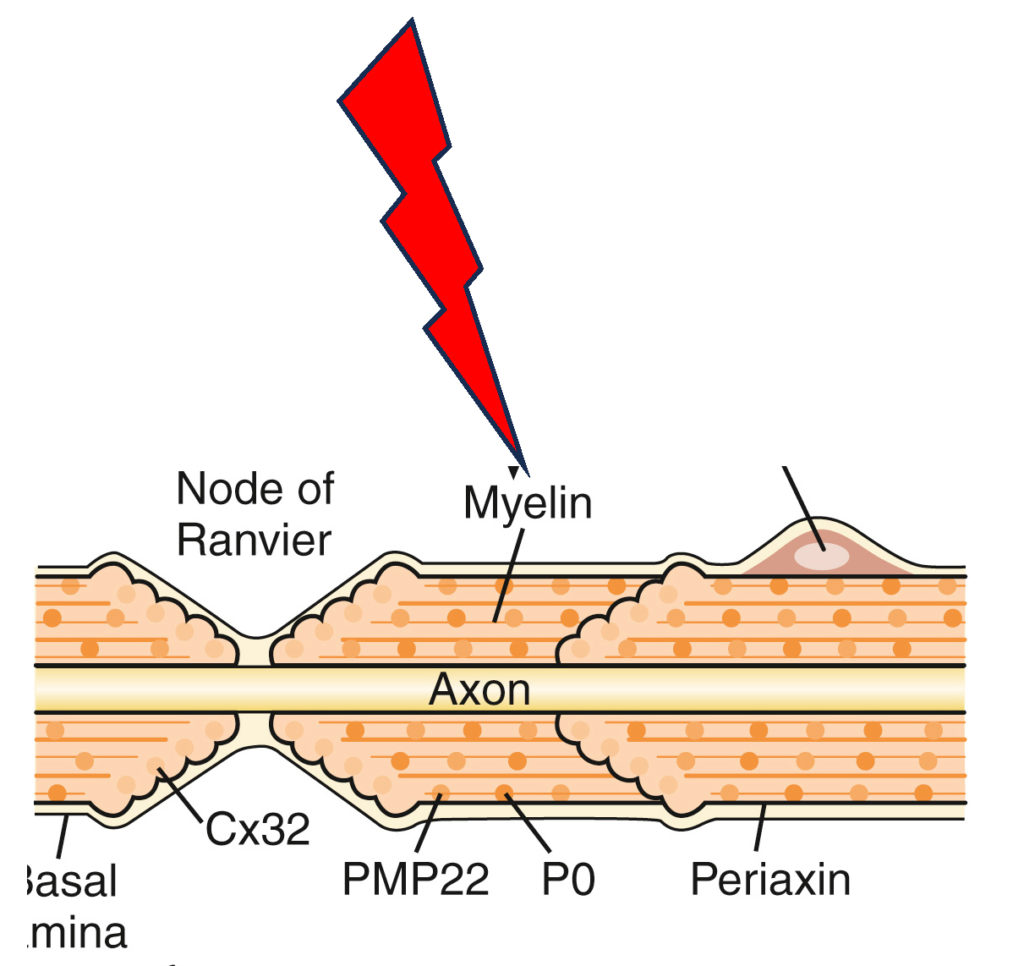
- Abnormal myelin sheath protein is the basis of this degenerative neuropathy.
- There are marked reductions in motor NCVs and nerve biopsy findings of demyelination and onion bulb formation.4
- This results in a combination of motor and sensory disturbances.
- Symptoms
Symptoms begin during the first or second decade of life:4
-
- Progressive weakness.
- Muscle wasting (foot intrinsics, peroneals, and tibialis anterior).
- Sensory impairment, distal leg.
- Symmetric.
- Upper extremities are affected in 2/3 of patients later in life.
- Absent ankle reflexes.
- Frequent ankle sprains, gait instability, clumsiness.
- Diminished vibration sense and light touch in the feet and hands.
Associated conditions

Bradley WG. Disorders of Peripheral Nerves, Fig. 106.08.
Question
Proper management of this patient should include evaluation for which of the following findings?
Common physical exam findings
- Pes cavus foot
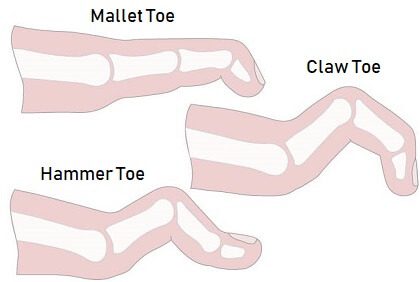
- Hammer toes
- Inverted champagne bottle legs
- Scoliosis
- Distal lower extremity and upper motor weakness and hyporeflexia.
Bradley WG. Disorders of Peripheral Nerves, Fig. 106.08.
Charcot-Marie-Tooth Disease type 2
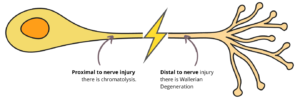
- Wallerian axonal degeneration with intact myelin sheath.
- Motor NCVs are normal or near normal, and nerve biopsy reveals axonal loss without prominent demyelination.4
- Symptoms commonly present in the second decade, or even later.4
- 20% are asymptomatic.
- Foot and spinal deformities are less common.
- The presentation is more variable (optic nerve atrophy, foot ulcers, vocal cord atrophy, intercostal muscle weakness).
Note
One cannot differentiate CMT Type 1 or 2 based on clinical presentation alone.
X-linked Charcot-Marie-Tooth Disease
- Phenotypically similar to CMT1.
- Consider in CMT that does not demonstrate male-to-male transmission.
- 7%–16% of all forms of CMT, making it the second most common form of CMT.4
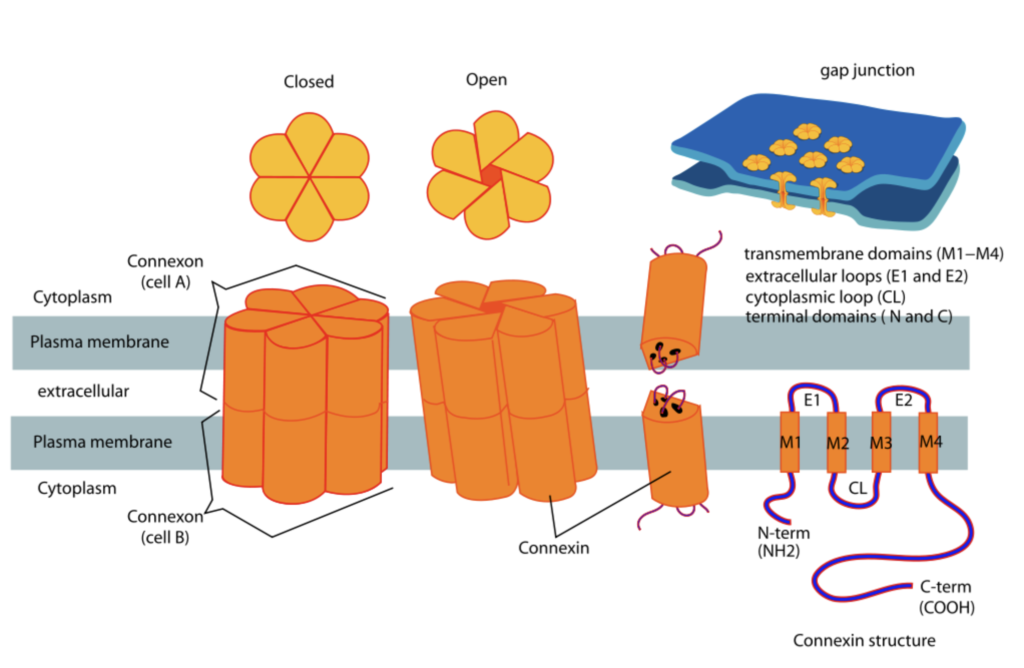
- Commonly affects gap junction protein B1.4–5
- Connexins are a family of highly related genes and can affect cranial nerve/peripheral nerve/non–nervous system cells.
- Male subjects tend to be more severely affected; females are asymptomatic.
Charcot-Marie-Tooth Disease type 4
- Consider in a patient with AR inheritance pattern.5
- Accounts for less than 10% of all CMT cases.4
- Symptom onset is in early childhood and has a faster progression than CMT1 and CMT2.
- Progressive weakness leads to the inability to walk in adolescence.
- Typically demyelinating. The most common gene affected is GDAP1 (CMT4A), which codes for a mitochondrial membrane protein.5
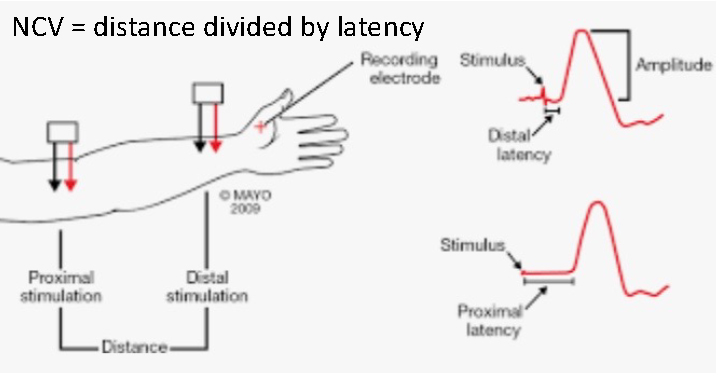
- Testing
- Treatment
- Nerve conduction studies:
- Nerve conduction velocity:4
- CMT1: <38 m/s.
- CMT2: >38 m/s.
- INT CMT: 24–45 m/s.
- EMG:
- Uniform and symmetric abnormalities.
- Nerve conduction velocity:4
- Molecular and genetic testing.
- CSF analysis, CBC, and CMP normal.
Reilly MM. Classification and diagnosis of the inherited neuropathies. See at Diagnosis of Charcot Marie Tooth Disease.
- Symptomatic treatment.4–6
- Physical therapy.
- Proper footwear and insoles and orthotics.
- Avoid insults to PNS, like neurotoxic drugs.4,6
- Risks with pregnancy (birth complications/↑severity of disease).4,6
- Orthopaedic consultation for cavovarus, claw foot, hammer toes, and scoliosis.
- No effective pharmacological treatment.
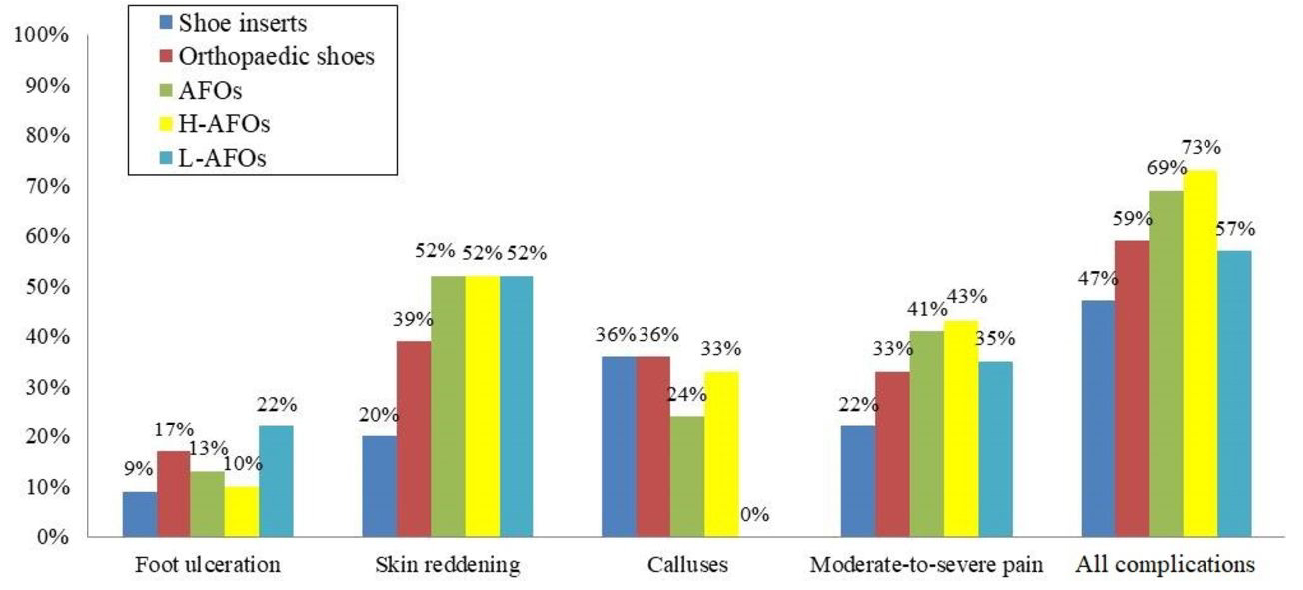
Orthotics and CMT
Perceived improvement in gait, stability/balance, and reduction in falls.7
-
- 21% never used, 31% abandonment, 69% reported complications.7
The utility of physical therapy in CMT
- After intensive rehabilitation treatment, all outcomes significantly improved.8
- This improvement was lost at the 1-year mark.8
Conclusion
Intensive rehabilitation program improves short-term symptoms and functional outcomes in a cohort of inpatients affected by mild to moderate CMT.
Source: Ferraro F, Calafiore D, Curci C, Fortunato F, Carantini I, Genovese F, Lucchini G, Merlo A, Ammendolia A, de Sire A. Effects of intensive rehabilitation on functioning in patients with mild and moderate Charcot-Marie-Tooth disease: a real-practice retrospective study. Neurol Sci. 2024 Jan;45(1):289-297. doi: 10.1007/s10072-023-06998-0. Epub 2023 Aug 8. PMID: 37552411; PMCID: PMC10761523.
Rigid vs. flexible hindfoot deformity
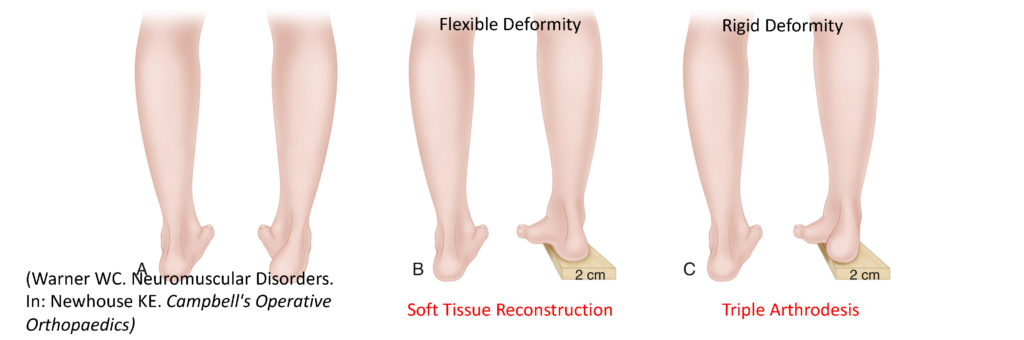
- Coleman Block Test
- WB AP, lateral, and oblique radiographs6
Pathoanatomy of cavovarus foot deformity
Question
The cavus deformity in Charcot-Marie-Tooth disease is caused by which muscular imbalance?
Peroneus brevis overpowering peroneus longus.
-
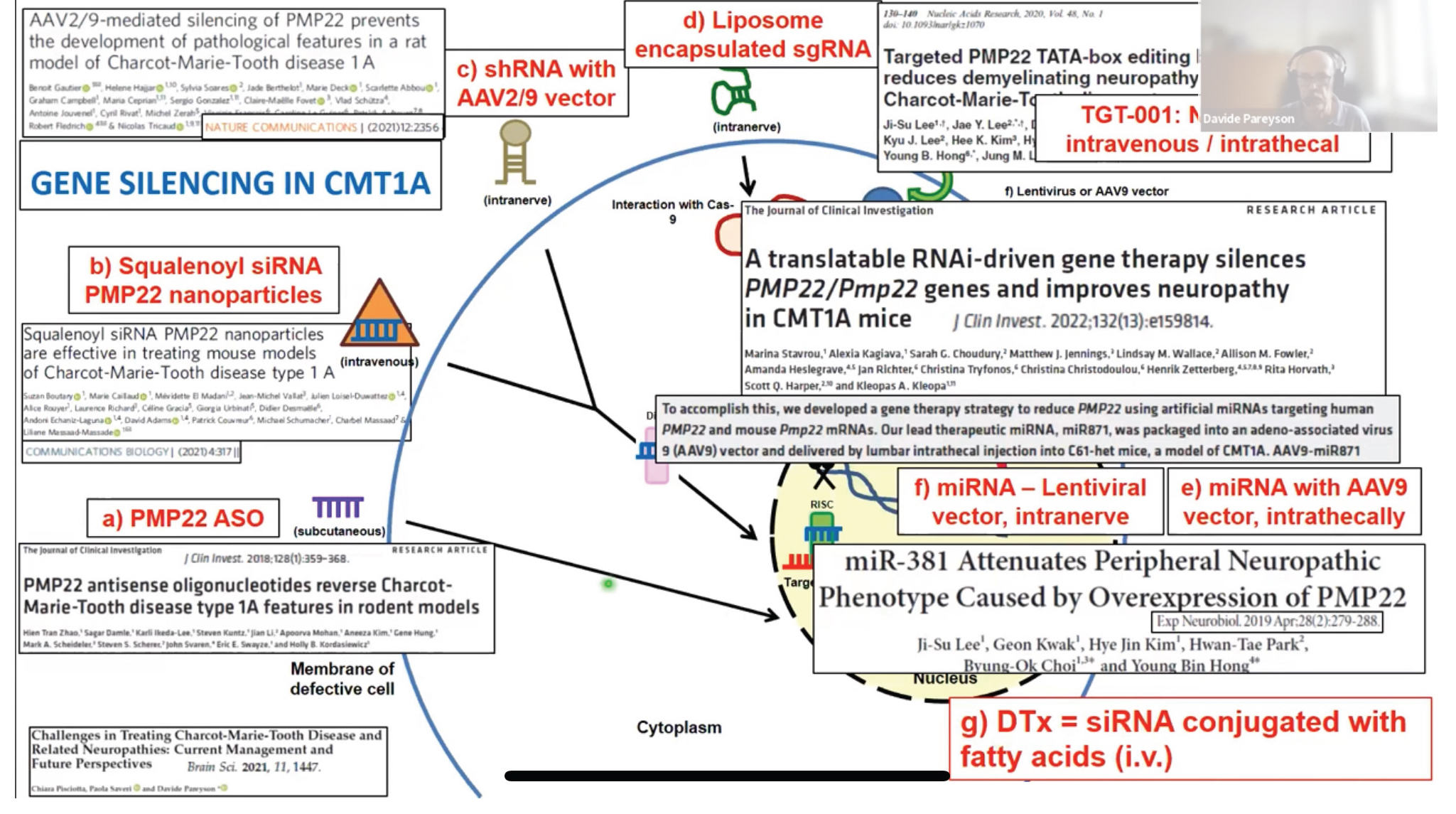
Novel treatments
- Differential for Polyneuropathies
- Fredrich ataxia.
- Alcoholic polyneuropathy.
- Chronic inflammatory demyelinating polyneuropathy.
- Refsum disease.
- Vitamin B12 deficiency.
- Guillain-Barré.
- Thyroid disease.
- Diabetes Mellitus.
- Amyloid neuropathies.
- Leprosy.
- HIV-associated distal symmetric polyneuropathy.
- Toxic polyneuropathy:
- Chronic: Cisplatin, doxorubicin
- Acute: Diphtheria toxin, suramin, amiodarone.
Text citations
- Kazamel M, Boes CJ. Charcot Marie Tooth disease (CMT): historical perspectives and evolution. Journal of neurology. 2015;262(4):801–805. doi:10.1007/s00415-014-7490-9
- Orthobullets. Accessed December 7, 2023.
- Martyn CN, Hughes RA. Epidemiology of peripheral neuropathy. J Neurol Neurosurg Psychiatry. 1997;62(4):310–318. doi:10.1136/jnnp.62.4.310
- Bradley WG, Katirji B. Disorders of Peripheral Nerves. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff’s Neurology in Clinical Practice. 8th ed. Elsevier; 2022: 1853–1929. Accessed December 1, 2023.
- Morena J, Gupta A, Hoyle JC. Charcot-Marie-Tooth: From Molecules to Therapy. International Journal of Molecular Sciences. 2019; 20(14):3419. https://doi.org/10.3390/ijms20143419
- Warner WC, Sawyer JR. Neuromuscular Disorders. In: Newhouse KE. Campbell’s Operative Orthopaedics. 7th ed. Yale J Biol Med; 1987. 1459–1490. Accessed December 1, 2023.
- Bertini A, Manganelli F, Fabrizi GM, et al. Use, tolerability, benefits and side effects of orthotic devices in Charcot-Marie-Tooth disease. Journal of Neurology, Neurosurgery and Psychiatry. Published online first: November 2, 2023. doi: 10.1136/jnnp-2023-332422
- Ferraro F, Calafiore D, Curci C, et al. Effects of intensive rehabilitation on functioning in patients with mild and moderate Charcot-Marie-Tooth disease: a real-practice retrospective study. Neurol Sci. Published online August 8, 2023. doi:10.1007/s10072-023-06998-0
- Boutary, S., Caillaud, M., El Madani, M. et al. Squalenoyl siRNA PMP22 nanoparticles are effective in treating mouse models of Charcot-Marie-Tooth disease type 1 A. Commun Biol 4, 317 (2021). https://doi.org/10.1038/s42003-021-01839-2
Image citations
- Bradley WG, Katirji B. Disorders of Peripheral Nerves, Fig. 106.10, 106.9, 106.8. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff’s Neurology in Clinical Practice. 8th edition. Elsevier; 2022. Accessed December 1, 2023.
- CMTA Logo. Charcot-Marie-Tooth Association. Accessed December 7, 2023.
- Connexins and Connexin Structure. Mariana Ruiz.
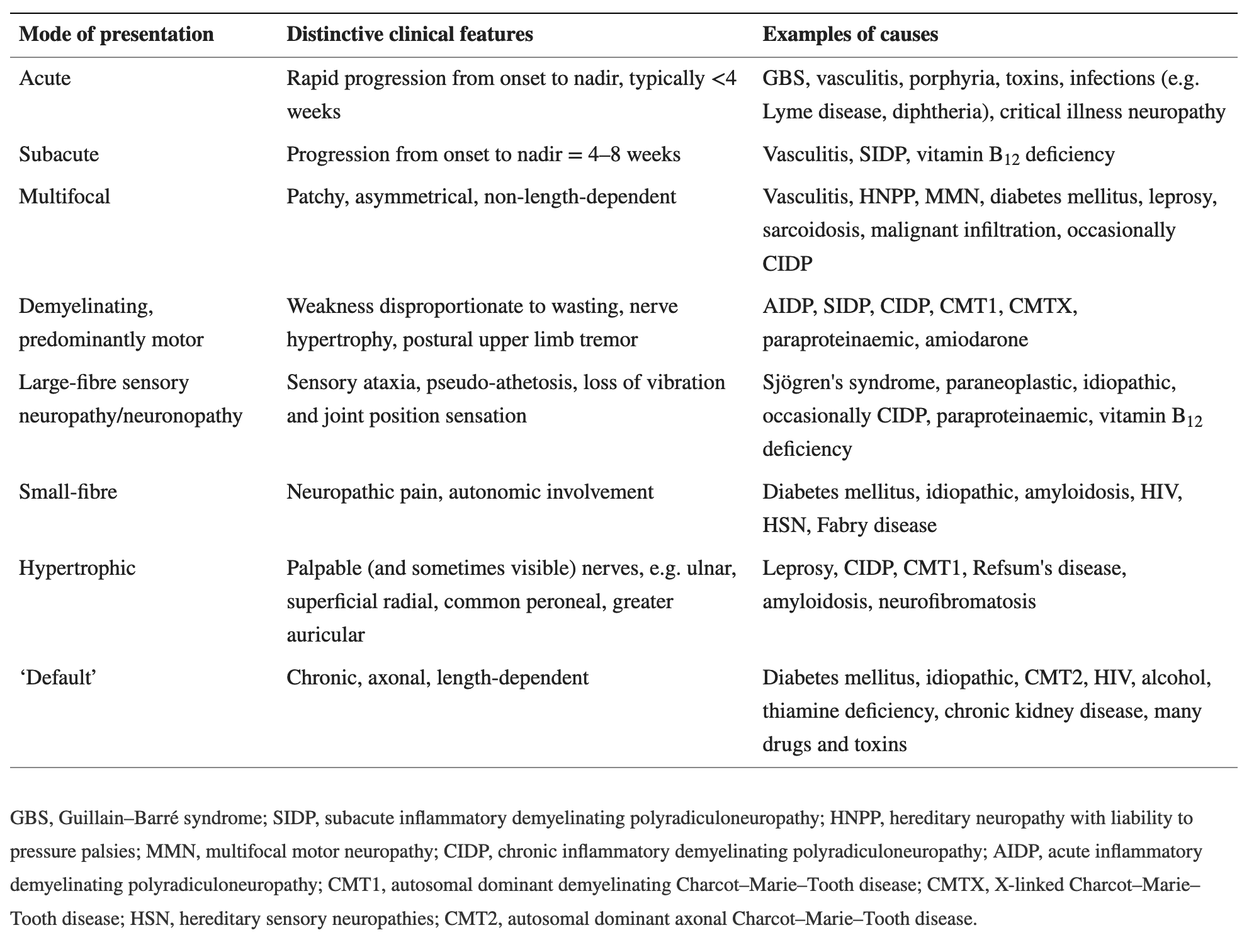
- Ginsberg L. Acute and chronic neuropathies, Table 2. Medicine (Abingdon). 2020;48(9):612–618. doi:10.1016/j.mpmed.2020.06.009
- Morena J, Gupta A, Hoyle JC. Charcot-Marie-Tooth: From Molecules to Therapy, Figure 1. International Journal of Molecular Sciences. 2019; 20(14):3419. https://doi.org/10.3390/ijms20143419
- Nam SH, Choi BO. Clinical and genetic aspects of Charcot-Marie-Tooth disease subtypes, Tables 1–3. Precis Future Med. 2019. Vol. 3(2):43-68. DOI: 10.23838/pfm.2018.00163
- Nerve Conduction Study. Mayo. 2009.
- Pareyson D. Treatment of Charcot Marie Tooth Disease. www.youtube.com. Accessed December 1, 2023.
- Reilly MM. Classification and diagnosis of the inherited neuropathies. Ann Indian Acad Neurol. 2009;12(2):80–88. doi:10.4103/0972-2327.53075
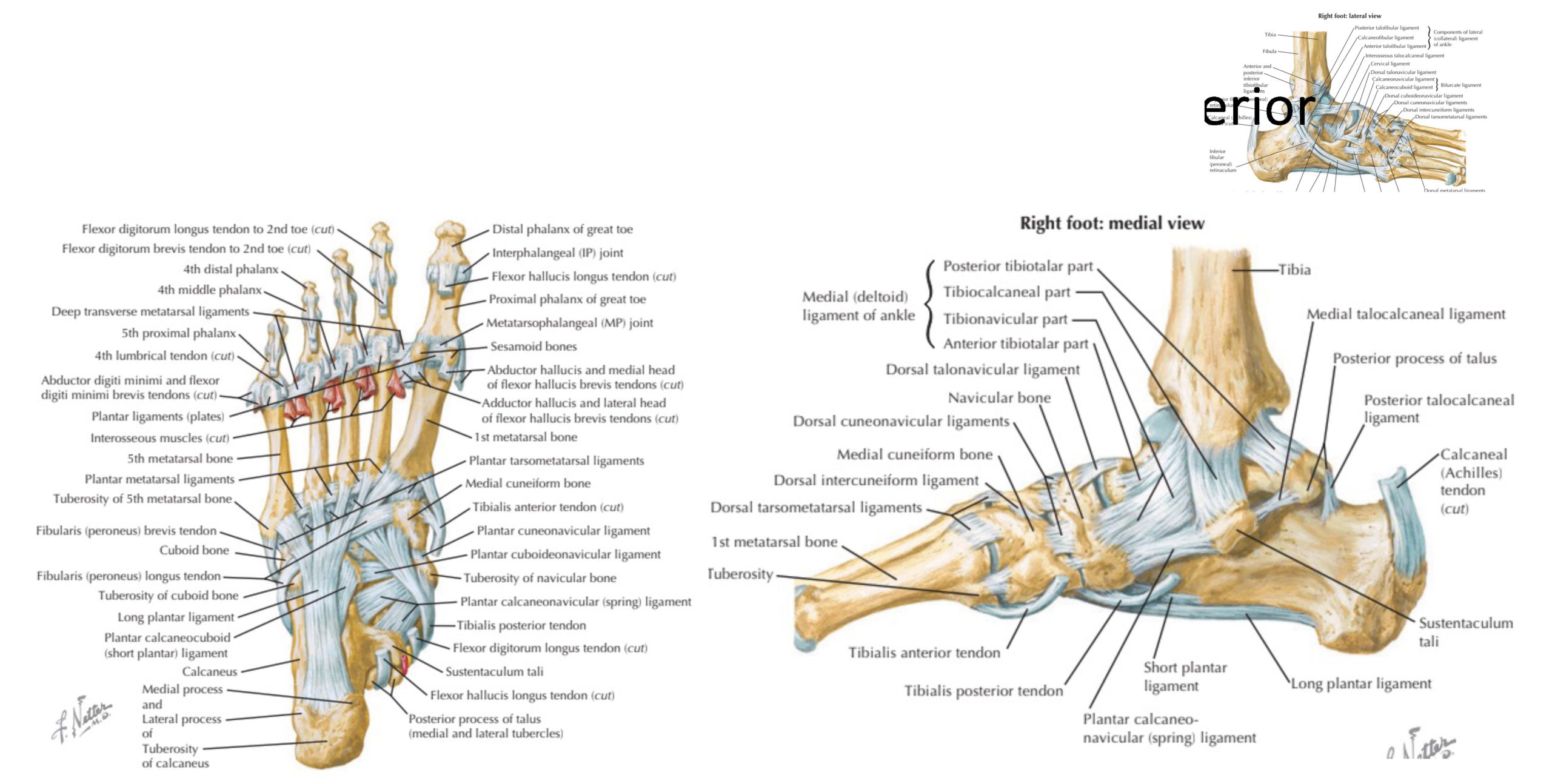
- Thompson JC, Netter FH. Netter’s Concise Orthopaedic Anatomy. 2nd ed. Elsevier Health Sciences; 2009.
- Wallerian Degeneration. thePlasticsFella. Created June 9, 2022. Accessed December 1, 2023.
- Warner WC, Sawyer JR. Neuromuscular Disorders. In: Newhouse KE. Campbell’s Operative Orthopaedics. 7th ed. Yale J Biol Med; 1987. 1459–1490. Accessed December 1, 2023.
- Wilson C. Mallet Toe, Hammer and Claw Toe. Foot Pain Explored. Page last updated: November 14, 2023.
Image credits
Unless otherwise noted, images are from Adobe Stock.