Case study 2: Mariah—Where is the lesion?
Question
Case study 3: Brad—Hands tingling
Question
Guillain-Barré syndrome (GBS)
- Respiratory failure is the do not miss life-threatening complication of this condition.
-
Progressive rapid ascending demyelinating polyneuropathy.
-
Resp or GI infxn triggers T-cell attack.
-
DDx: Botulism, West Nile, myasthenia, Lyme, tick paralysis and others. Note Miller-Fisher GBS variant (GQ1b ganglioside antibodies + CN findings, ataxia).
-
- Worsens over 2–4 weeks: Resp failure is biggest risk.
- Recovery usually spontaneous.
- May have paresthesias, but sensation is usually normal; diffuse arreflexia is common.
- Treatment is IVIG (or plasmapheresis)—avoid steroids!
- 80% are ambulatory at 6 months; relapse in 6%.
Case study 4: Daniel—Cook got burned
Question
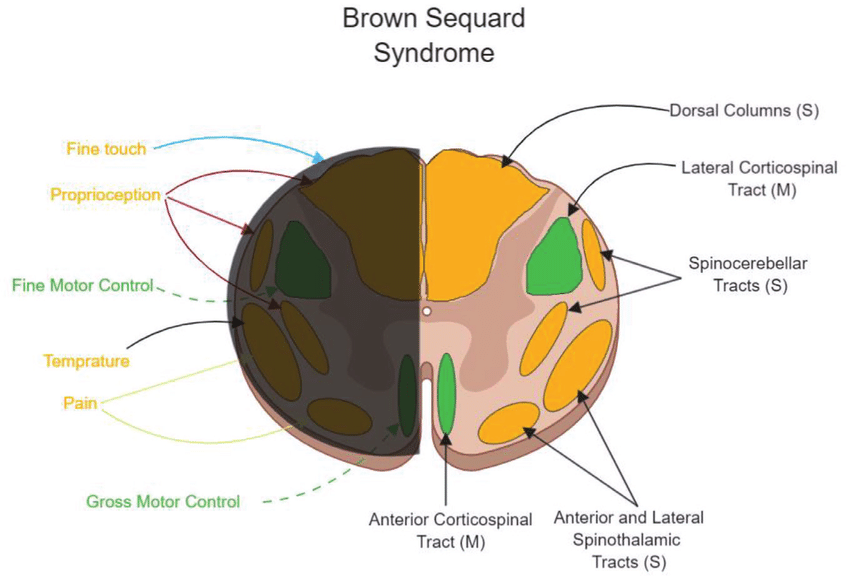
In the central cord (in the neck).
Question
The most likely diagnosis is syringomyelia. You should also consider MS in this man. Hemorrhage or tumor affecting the central spiral cord should also be considered.
Syringomyelia
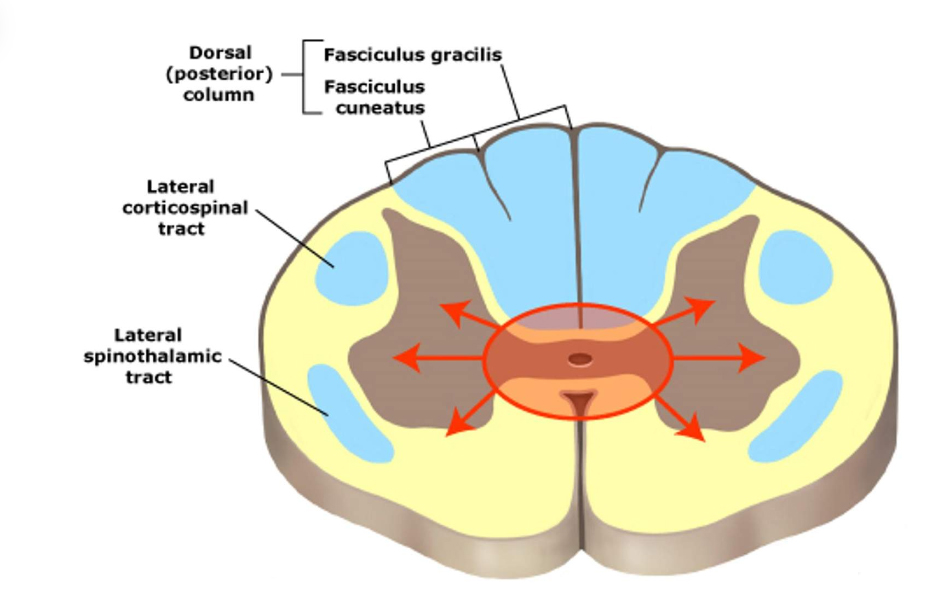
Central cord lesion caused by CSF collection.
Usual onset in 3rd–4th decade; men > women; slow progression.
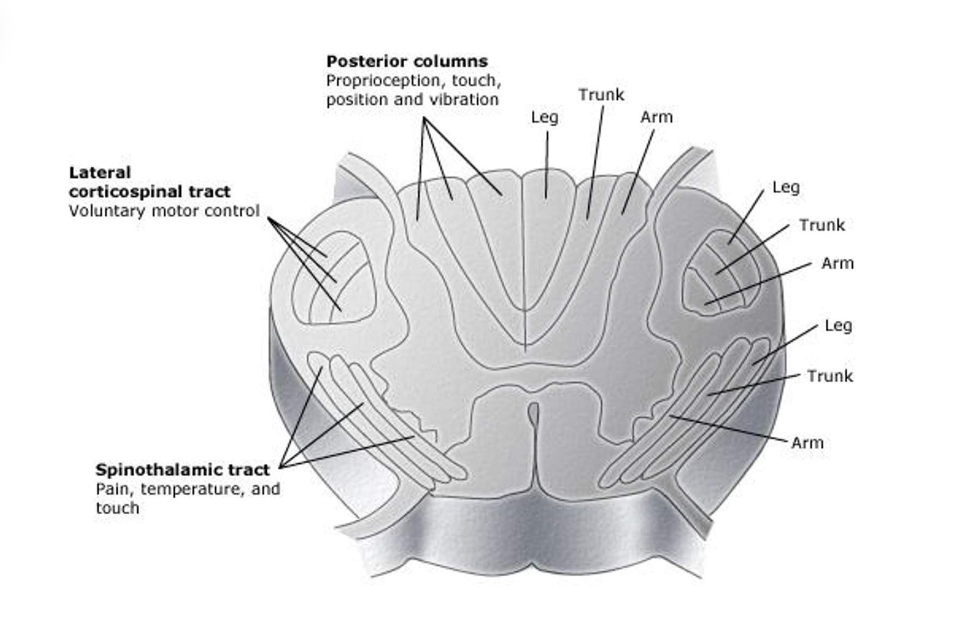
Loss of pain/temperature via disruption of the decussate spinothalamic fibers (dissociated sensory loss).
Extension to posterior columns loss of position and vibratory sensation in the feet.
Extension to anterior horns (motor neurons) hand amyotrophy with claw hands and muscle wasting of hands arms.
Question
- If he had extension to the posterior columns, he would develop loss of position and vibratory sensation in the feet.
- If he developed extension to the anterior horns, where the motor neurons are located, he would develop hand symptoms, including muscle wasting and contractures.
Case study 5: Cynthia—Difficulty swallowing
Unpack the case
The timing is progressive over months, making it unlikely to be a stroke. While she has pre-diabetes, it would be highly unusual to have these symptoms as complications of diabetes.
These symptoms could be described as:
- Speech “Bulbar.”
- Swallowing “Bulbar.”
- Lower-extremity weakness (distinguish LMN from UMN/central with testing).
Question
ALS
- Degenerative disease of motor neurons, leading to progressive weakness, atrophy, death.
- Upper-motor neuron (UMN) plus lower-motor neuron (LMN).
- Bulbar: Dysarthria and dysphagia.
- Weak extremities: Often isolated extremity weakness at presentation.
- Frontotemporal dementia in 50% of patients.
- Differentiate from MS: Oculomotor palsy, incontinence, and tremor rare in ALS but common in MS.
- DX: Both UMN + LMN and EMG evidence of LMN signs in at least 2 or more ALS regions.
- DDx is Multifocal motor neuropathy (no UMN), Cervical cord compression (LMN @ level and some UMN below that), vitamin B12 deficiency, copper deficiency. Exclude Lyme (can be focal), hyperparathyroidism, and thyrotoxicosis.
Image credits
Unless otherwise noted, images are from Adobe Stock.