Patient 1: Steve—Right-sided headache
A 55-year-old man comes to see you for recent onset of right-sided headaches which he refers to as “migraines.” He has some nausea with his headaches. He has no other symptoms with the headaches.
Question
Along with a careful neuro exam, the best thing to do first is:
Patient 2: Lina—Left-sided headache
A 49-year-old woman with polycystic kidney disease (PCKD) is concerned about increasing left-sided headaches. She has hypertension controlled on multiple medications.
BP: 150/92
Patients with polycystic kidney disease are at high risk for aneurysm!
8%–12% vs. 2%–3% in the general population.
Any new headache should prompt evaluation for bleeding or aneurysm.
See PCKD extrarenal manifestations in
UpToDate.
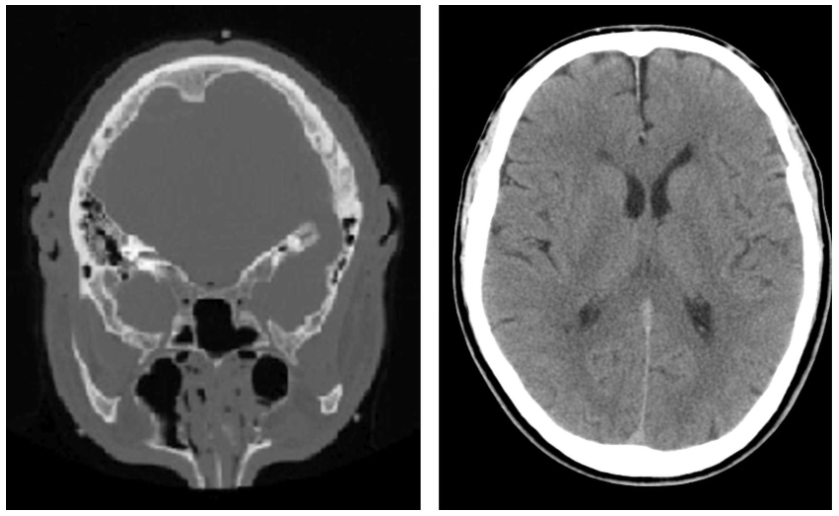
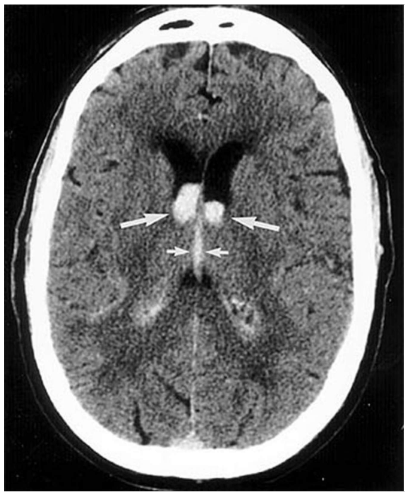
Patient 3: Tom—Slipped on the ice
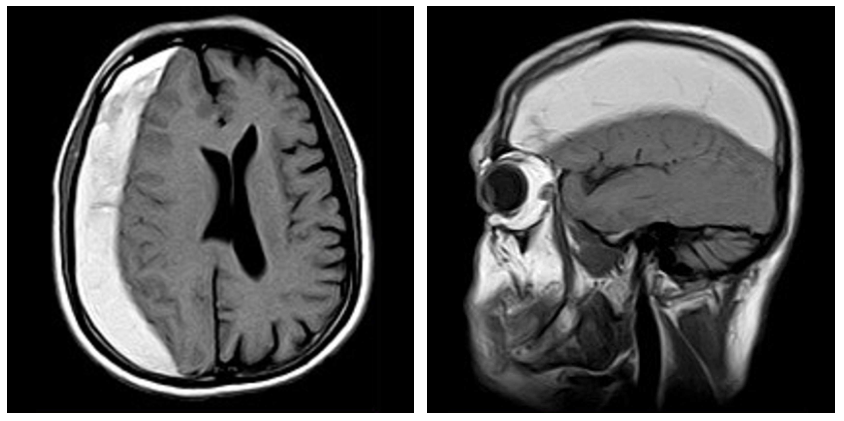
Subdural hematoma
In this case, evacuation and anticoagulation will need to be stopped.
MRI
- Good for soft tissues.
- More sensitive than CT for masses.
- May be normal early on in head bleed or stroke.
- Diffusion-weighted MRI determined to be better than CT for acute stroke.
Source: Radiology. 2002 Aug.,224(2):353–60.
Patient 4: Curtis—Headache in my temple
A 70 year-old man presents with right-sided headaches “in my temple” for 3 weeks. He also says he can’t chew properly: “I had to stop eating steak last night because my jaw started to hurt. I think it’s my teeth, but I can’t get into the dentist 'til next month.”
He has not had any vision changes, other new symptoms, or medication changes. He has had two root canals and had a tooth abscess 2 years ago. Sinuses are non-tender, his right temporal artery is tender. A CBC shows Hgb of 10. ESR is 20.
Question
What is the next best step in this case?
Despite a normal ESR, this patient probably has temporal arteritis (a small percentage (4–5%) of patients have a normal ESR and a normal CRP). Temporal artery biopsy (> 0.5cm, but 1–1.2 cm may be preferred) was the “gold standard” and is a low-risk, well-tolerated procedure. However, up to 44% of biopsies are false negatives, and sensitivity of bx ranges from 50 to 95% depending on prevalence in the population, length of biopsy, exposure to steroids, etc. Importantly, color Doppler ultrasound (CDUS) is becoming the first step in diagnosis in some centers. While the sensitivity of CDUS ranges from 55% to 100%, imaging of other regional arteries may be helpful (e.g., abnormalities in the carotid or subclavian arteries may be helpful).
Reminders
The most common headaches are:
-
Tension.
-
Migraine: With or without aura.
-
Cluster (neuralgias).
-
Medication overuse (rebound/chronic daily).
Head imaging?
-
Abnormal neuro exam.
-
New headache that is atypical.
-
Patient over age 50.
-
Trauma.
-
Anticoagulants.
-
History of cancer.
-
HIV.
-
After seizure.
- Consider Emergency CT in adults and children with first seizure, children younger than six months, and patients with AIDS.
- Consider immediate CT in patients who present with seizure in the ED and have abnormal findings on neurological examination, a predisposing history or focal seizure onset.
- CT changes treatment in up to 17% of adults and 8% of children presenting with a first seizure in the ED.
Final thoughts
- Always ask about caffeine, drugs, and specific precipitants.
- Think about facial pain—teeth, sinuses, jaw.
- Especially in older people with unilateral headaches always think about temporal arteritis and check ESR.
- Always do a careful exam.
- Know when to image (and when not to).
- Follow-up is important—if it doesn’t all make sense keep asking questions.
Note
Does this patient with headache have a migraine or need neuroimaging?
JAMA 2006;296:1274–83.
Image credits
Unless otherwise noted, images are from Adobe Stock.