Case study 1: Amanda—Worsening migraines
Stop and recall exercises:
Free recall helps you remember, so try to do answer these questions without looking at references.
Questions
What are the major types of migraines?
What is the definition of "chronic migraine?"
Write everything you remember about migraine diagnosis, treatment, and prevention.
Migraine is the leading cause of morbidity, ranked #7 in the world as a cause of disability (2010 statistics).
Migraine
Pathophysiology: Likely related to neurologic hypersensitivity to internal and external triggers of the trigeminovascular system; vasoactive neuropeptides promote changes in hypothalamic activity and dural afferent input from the meninges, as well as cortical spreading depression (CSD).
- Major Subtype
- Minor subtype
- Migraine without aura
- Migraine with aura
- Migraine with aura: Aura onset precedes or accompanies HA with sx increasing over ~5 minutes and lasting 5–60 minutes.
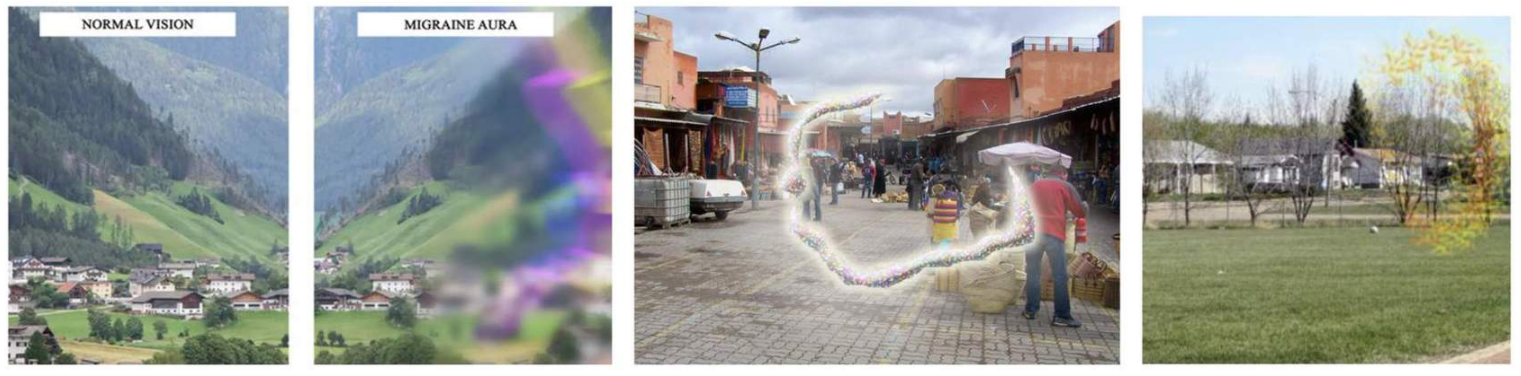
- Aura: “. . . fully reversible set of neurologic symptoms, often visual or sensory symptoms, that typically develops gradually, recedes, and is then followed by headache accompanied by nausea, vomiting, photophobia, and/or phonophobia.”
- Visual symptoms: Scotomata (negative sx); scintillations (positive sx).
- Migraine without aura (most common): Unilateral, pulsating, n/v, photo/phonophobia, moderate/severe pain, aggravation with activity.
- Ocular migraines (“classic aura without headache”).
- Basilar: Brainstem-predominant symptoms
- Vestibular: Transient vestibular or balance problems without experiencing an actual headache.
- Hemiplegic migraines: Have a rare type of aura that features unilateral weakness, likely due to transient cortical depression.
Criteria for diagnosis
ICHD-3 (Beta) Migraine without aura8
- At least 5 headache attacks fulfilling the criteria B–D.
- Attacks last 4–72 hours.
- With at least 2 of the following characteristics:
- Unilateral location.
- Pulsating quality.
- Moderate or severe pain intensity.
- Aggravation by or causing avoidance of routine physical activity.
- At least 1 of the following during headache:
- Nausea and/or vomiting.
- Photophobia and phonophobia.
- Not better accounted for by another ICHD-3 diagnosis.
ICHD-3 = International Classification of Headache Disorders, 3rd edition.
Criteria for diagnosis
- Same diagnostic criteria as migraine without aura (see prior slide); plus aura.
- Aura can precede headache symptoms by hours to days; generally subsides 5–60 mins prior to onset of headache.
- Common aura: Scintillating scotoma, photophobia, phonophobia, nausea/GI upset.
Tap the image to enlarge.
Migraine treatment
American Headache Society Treatment Guidelines, Updated 23 June 2021.
Prescribed to treat individual attacks (take at symptom onset).
- NSAIDs and combination (caffeine-containing) analgesics.
- Triptans (e.g., sumatriptan): Subcutaneous (highest and fastest response), oral, dissolvable, nasal spray; 30% of patients don’t respond.
- Selective 5-HT1B/D serotonin agonists.
- Calcitonin gene-related peptide (CGRP) receptor antagonists (gepants): NEW (also just FDA-approved for prevention, but $$$$).
- Ergotamine-containing preparations (e.g., IV/intranasal dihydroergotamine).
- Antiemetics (e.g., metoclopramide or prochlorperazine).
Prescribed to reduce the overall frequency and severity of chronic individual migraines. Goal is reduction of disability.
- Anticonvulsants (e.g., topiramate, valproic acid).
- Tricyclic antidepressants (e.g., amitriptyline, nortriptyline).
- Beta blockers (e.g., propranolol).
- Calcium channel blockers (e.g., diltiazem, verapamil).
- Botulinum toxin (Botox): Expensive; must meet certain criteria for insurance coverage.
- Opioids and butalbital compounds are avoided; high risk of overuse and medication overuse (formerly “rebound”) headache (MOH).
Cluster headache
Note
Prevalence of < 1% in general population; more common in males and smokers.
- Signs and Symptoms
- Ddx
- Treatment
15–180 minutes, 1–8 times per day
- Severe unilateral, stabbing pain located behind one eye.
- May have associated autonomic symptoms:
- Lacrimation.
- Scleral injection.
- Ptosis.
- Rhinorrhea.
- Sweating.
- Generally transient in nature, coming to maximum intensity within minutes and lasting no longer than a couple of hours. May be cyclic, with headache-free periods in between.
- Sinusitis.
- Primary ocular conditions.
- Cavernous sinus process (thrombosis).
- Supplemental 100% O2 via nasal cannula (usually x 20 mins).
- Medications:
- Abortive: Sumatriptan/dihydroergotamine injections; lidocaine nasal drops.
- Preventative: Verapamil >> galcanezumab (CGRP monoclonal ab); topiramate; lithium [high side-effect profile].
- Dual-action (abortive + preventative): Vagal nerve stimulator recently approved by the FDA.
Image credits
Unless otherwise noted, images are from Adobe Stock.