Generalized motor (“tonic clonic”) seizures
- Pathophysiology
- Clinical presentation
- Workup
Abnormal electrical activity in bilateral cortical or subcortical areas; often initially localizes to one side of the brain (focal seizure) and then spreads bilaterally to become generalized.
“Grand mal” seizures
Great video by Epilepsy Toronto
-
Vocalization (patients may cry out, grunt, or make other noises).
-
Loss of consciousness.
-
Rhythmic shaking, muscle jerks, or spasms.
Tonic-clonic seizure activity*
-
Tonic = stiffening of muscles.
-
Clonic = jerking or twitching.
*Note that 1–2 tonic-clonic movements can be seen with syncope (brain hypoxia), and this does not constitute a seizure, per se.
After initial seizure, if unprovoked, must determine cause.
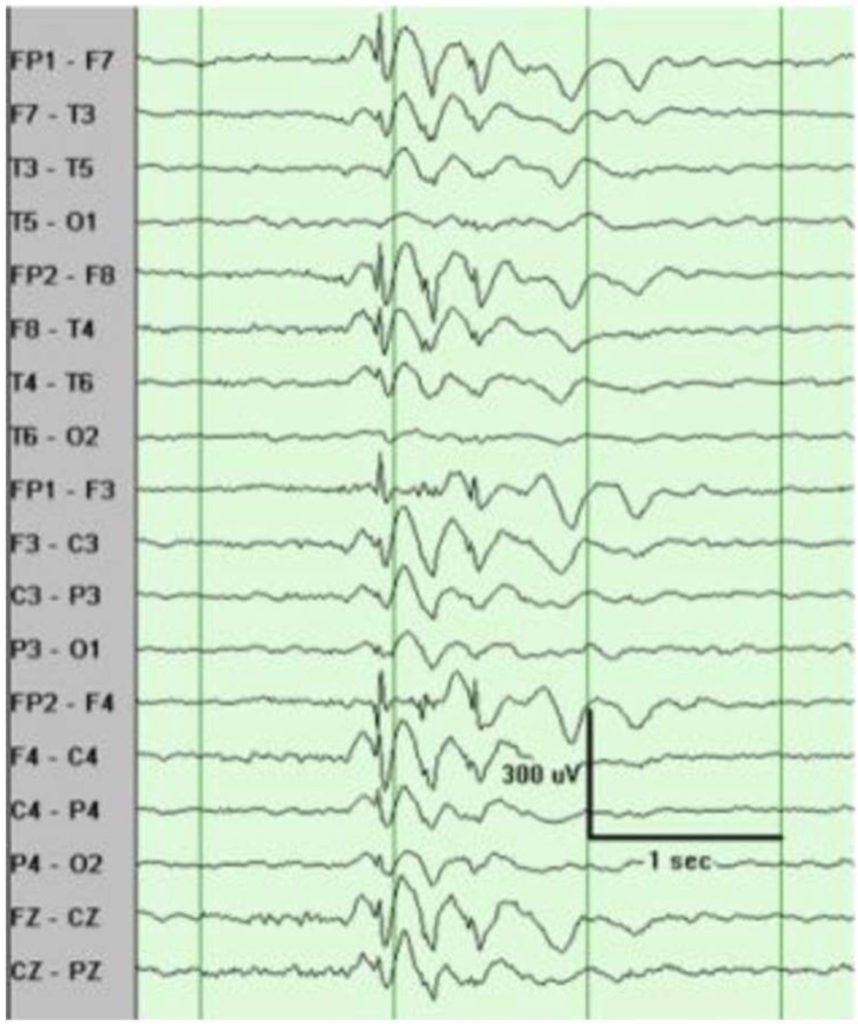
- EEG: Bilateral, symmetric, generalized epileptiform waves. This may follow unilateral, localizing initial seizure activity.
- MRI: r/o lesion, brain bleed, etc.
- CBC/CMP: Severe anemia, signs of infection, metabolic derangements.
- Urinalysis (UA); urine culture if infection is suggested by H&P; urine toxicology.
EEG consistent with generalized epilepsy. Spikes are usually followed by a slow wave.
Generalized non-motor (“absence”) seizures
- Pathophysiology
- Clinical presentation
- Diagnosis
- Treatment
- Generally more common in kids, especially ages 4–14.
- Exact etiology is unknown; assumed to be genetic.
- Often precipitated by hyperventilation.
- Transient loss of awareness or focus; no loss of consciousness or body tone.
- Patient may stop what they are doing and “stare into space.”
- Other common signs: Rapid blinking, repetitive chewing, or lip smacking motions.
- May go unnoticed for many months or years, and occur multiple times per day. Some children are wrongly thought to have inattentive ADHD, or told they are “not paying attention” in school, which brings the problem to parents’ attention.
Clinical presentation
- Parents and/or teachers may describe episodes.
- May also be able to induce an absence seizure on exam via hyperventilation.
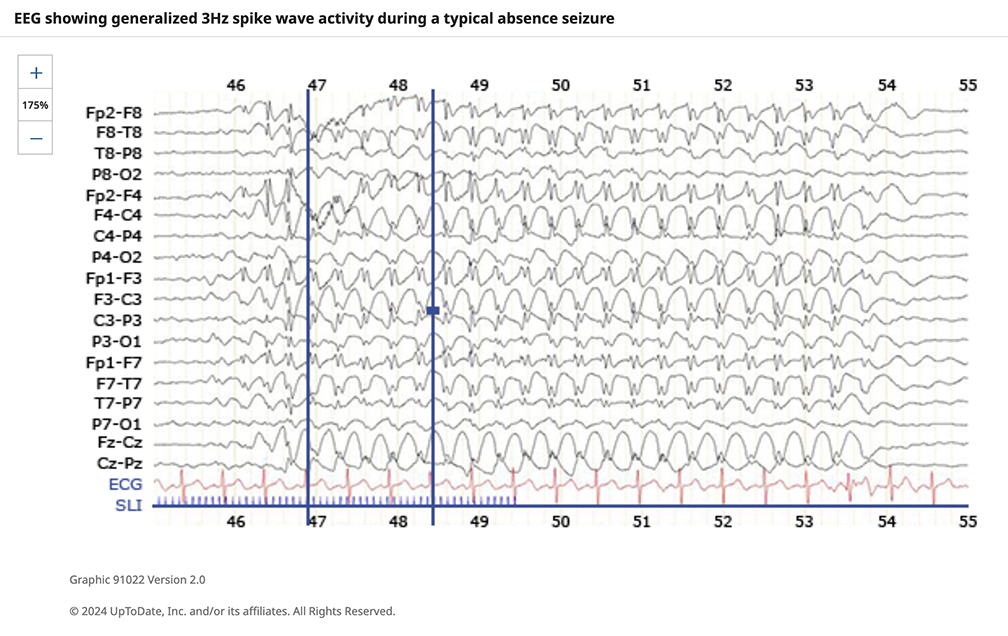
- EEG: 2.5–5 Hz spike wave discharges (3 Hz common).
Status epilepticus
- Definition
- Clinical guidelines
- Management
- Medical emergency involving sustained seizure activity that poses many risks to the patient, including compromise of cardiovascular and cerebral function.
- The definition of generalized convulsive status epilepticus (GCSE) originally proposed by the International League Against Epilepsy (ILAE) differs from the threshold for intervention used in clinical medicine.
- ILAE: Seizure activity for > 30 mins (single seizure) or an incomplete return to baseline between multiple discrete seizures during a 30-minute period.
- > 5 mins of continuous seizure activity (individual seizure).
- 2 discrete seizures between which there is incomplete return to baseline.
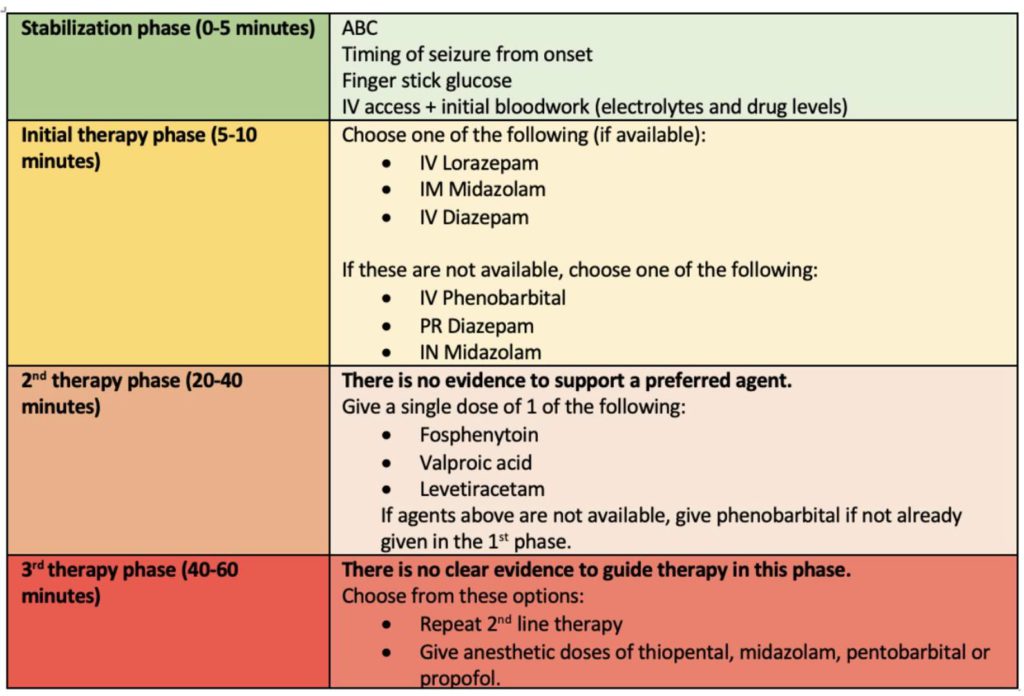
- Assess/stabilize ABCs = airway, breathing, circulation.
- Rapid neuro exam.
- Labs: CBC, CMP, urine toxicology, anti-seizure medication levels (if appropriate). ABGs if intubation required.
- Fingerstick glucose: If hypoglycemic → give 100 mg thiamine and 50 mL IV 50% dextrose solution. Can also give IM glucagon.
- First-line: IV benzodiazepines (lorazepam or diazepam).
- If no response to benzodiazepines, give anti-epileptic medication (fosphenytoin, valproate, or levetiracetam) and prepare to intubate.
- The neuromuscular blocking agents used for intubation can help prevent muscle contractions manifested with seizure, but they do not address the underlying seizure activity → need EEG monitoring.