Case study 4: Ernie—New onset aphasia
In the ED, the patient was not oriented to person, place, or time. He was stringing words together that did not make sense and did not follow commands. NIH Stroke Scale was 8. Bilateral LE extremity strength is 4/5. Overnight, he had urinary incontinence.
Question
Which of the following is the most appropriate prescribing action at this time?
No medications indicated:
- Rationale: Medications are indicated at this time due to the high risk of seizure recurrence given his history of metastatic lung cancer. Stabilizing seizures in cancer patients is an important concept to keep in mind while on the medicine wards. In a patient with no known risk factor for seizure reoccurrence, two unprovoked seizures are typically needed before anti-epileptic medications are indicated.
Start Alteplase (tPA):
- Rationale: Alteplase is used for tPA and can only be given 3 to 4.5 hours after the onset of a stroke. This is known as the golden tPA window. After this time, the benefits of tPA are overshadowed by the risks of this medication, which is hemorrhage. Moreover, given the patient’s normal head CT and CT Angio, there is only a small possibility that the patient had a stroke. Symptoms are more consistent with a seizure. It is important to keep in mind that seizures can often mimic strokes!
Start Keppra/Levetiracetam (correct answer):
- Rationale: The patient’s clinical picture is consistent with a focal seizure that resulted in 8–12 hours of post-ictal confusion. This is the likely cause of his transient aphasia and motor weakness. Given his history of metastatic lung cancer, it is likely that the seizure is due to metastases to the patient’s brain that disrupted the normal electrical activity. Patient is at a high risk of a recurrent seizures. Up to 15–35% of patients with metastases to the brain can have seizures. This is a common problem in hospitals. It is important to stabilize the patient on an anti-seizure medication. Keppra has the safest drug profile out of all these drugs, can be given IV and is typically the first anti-epileptic medication used in the hospitalized setting. The biggest contraindication for Keppra is mood disorder as Keppra is known to destabilize mood.
Start Depakote/ Valproic Acid:
- Rationale: Depakote has many side effects including weight gain, pancytopenia, tremor, nausea/vomiting, teratogenic defects, and interaction with CYP450 enzymes. It is not the best drug for an older cancer patient who is on Warfarin. The risk of drug interactions makes it an unlikely choice.
Start Carbamazepine/Tegretol:
-
Rationale: Carbamazepine is not recommended due to the high risk of SIADH, which can worsen the patient’s hyponatremia. In addition, it interacts with CYP450 enzymes and can cause hepatotoxicity and agranulocytosis.
Start Phenytoin/Dilantin:
-
Rationale: Phenytoin is not recommended due to side-effect profile. It interacts with CYP450 enzymes and can cause gingival hyperplasia, osteomalacia, among many other side effects.
Start Lamotrigine/Lamictal:
-
Rationale: Lamictal has a relevantly benign side-effect profile aside from the potential of causing a Stevens Johnson Rash. This occurs in less than 1% of the population. However, because this rash is life threatening, the FDA *** recommends a strict titration schedule of Lamictal. It takes around 2 months to titrate to the full effective dose. Given that the patient has metastatic lung cancer w/ likely metastases to the brain, 2 months is too long of a time for this patient.
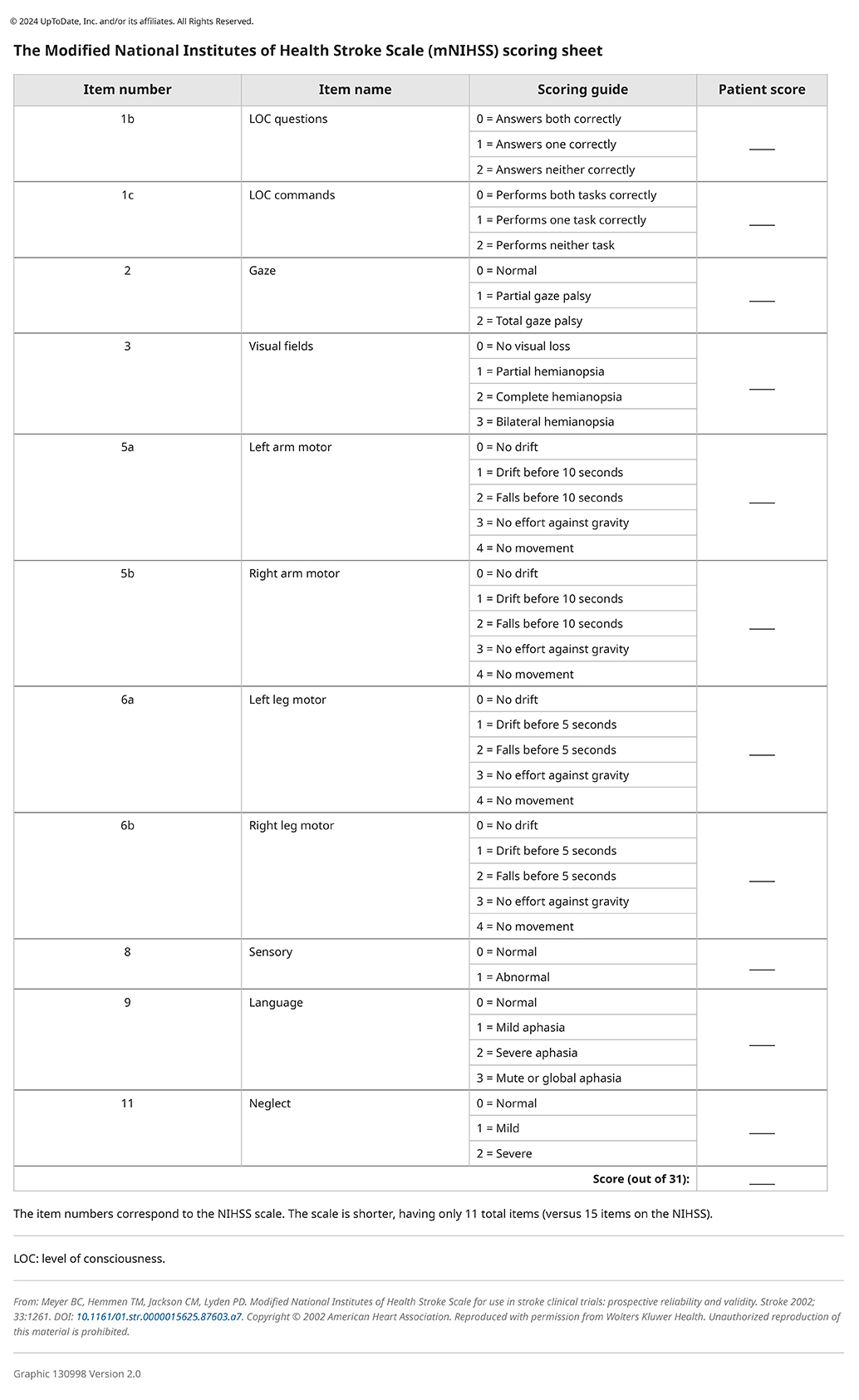
The Modified National Institute of Health Stroke Scale Scoring Sheet
References
- 2018 AHA/ASA Stroke Early Management Guidelines.” American College of Cardiology.
- Ajinkya, Shaun, et al. “Seizures in Patients with Metastatic Brain Tumors.” Journal of Clinical Neurophysiology, Publish Ahead of Print, 2019.
- Asadi-Pooya, Ali A., and Michael R. Sperling. “Clinically Important Drug Interactions with Antiepileptic Drugs.” Antiepileptic Drugs, 2015, pp. 120–126.
- Karceski, S. C. “Seizure Medications and Their Side Effects.” Neurology, vol. 69, no. 22, 2007.
- Singh, G., et al. “Seizures and Epilepsy in Oncological Practice: Causes, Course, Mechanisms and Treatment.” Journal of Neurology, Neurosurgery & Psychiatry, vol. 78, no. 4, 2006, pp. 342–349.
Image credits
Unless otherwise noted, images are from Adobe Stock.