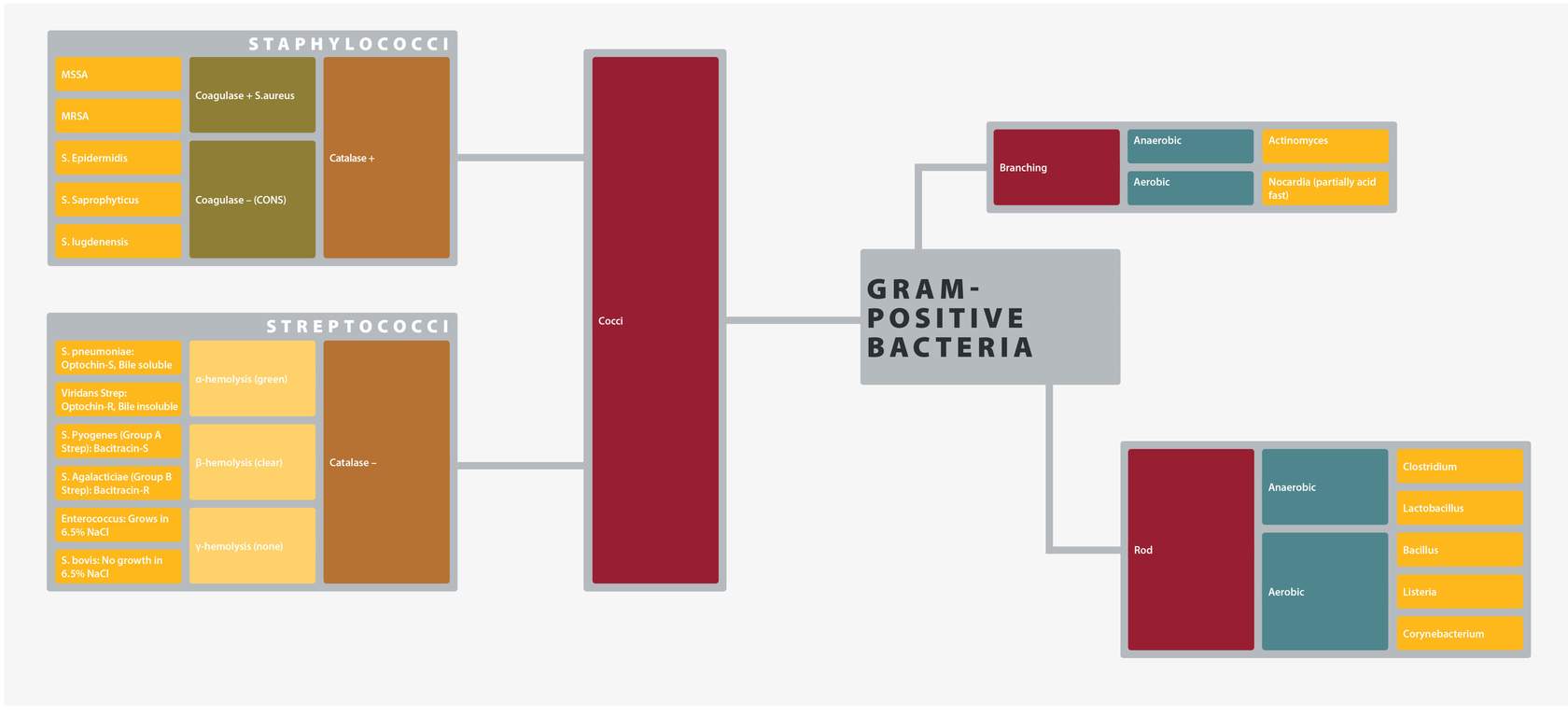
Gram-Positive Cocci (GPCs)
Staphylococci
Beta-hemolytic, golden colored colonies on blood agar.
One of the most common causes of infections in humans. The main habitat is the anterior nares in humans and as a colonizer of human skin. S. aureus has several important toxins that facilitate disease, including toxic-shock superantigens. S. aureus can cause disease almost anywhere in the body, but most commonly associated with purulent abscesses. Toxin-mediated diseases include food poisoning, toxic shock syndrome, and scalded skin syndrome.
Methicillin-resistant staphylococcus aureus (MRSA) is an important community and nosocomial-acquired pathogen that is associated with higher morbidity and limited therapeutic options. Antibiotics with MRSA activity include:
-
- Trimethoprim-Sulfamethoxazole
- Tetracyclines
- Clindamycin (variable)
- Vancomycin
- Daptomycin
- Linezolid
- Telavancin
- Ceftaroline
CONS are an abundant habitat of the normal microbiome of the skin and to a lesser extent, mucous membranes. Infections in humans usually result from one’s own flora due to breakdown in the natural barriers and defenses. Many strains are capable of forming biofilms that facilitate persistence. Most common infections include:
-
- Prosthetic joint infections
- Intravascular catheter–related infections
- Endocarditis
CONS tend to have more inherent antimicrobial resistance, and beta-lactam resistance is common. Infections are treated with antibiotics similar to those used for MRSA.
Notable species are:
-
- Staphylococcus saprophyticus: One of the common causes of urinary tract infection in women.
- Staphylococcus lugdenensis: Technically CONS but has virulence factors that make it much more like S. aureus in the clinical diseases it causes.
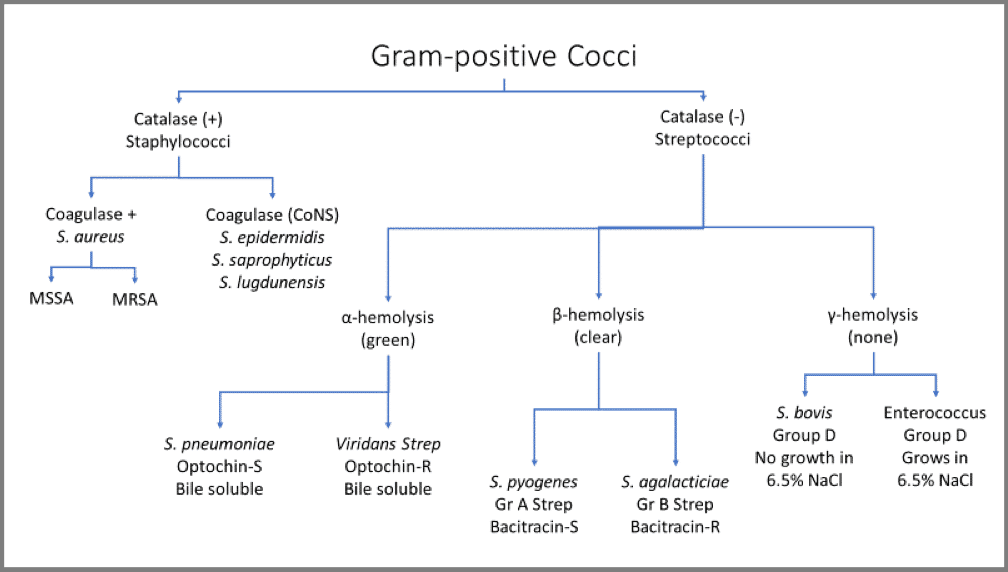
Streptococci
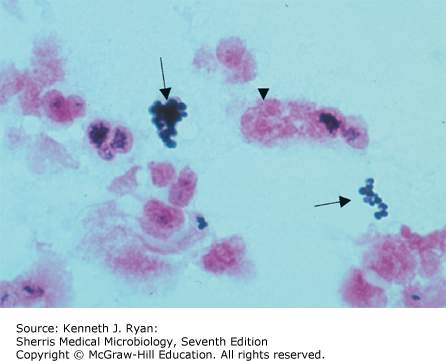
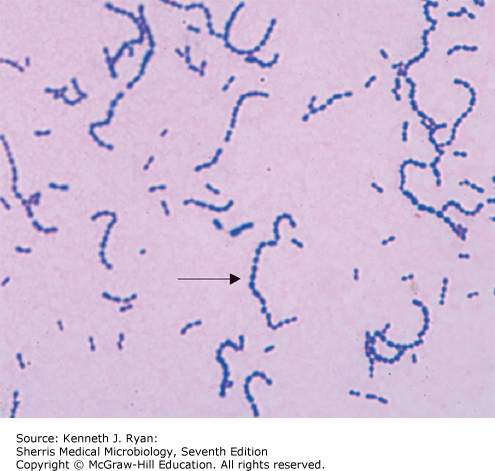
Gram-positive cocci that appear in chains and pairs on gram staining.
Group A streptococcus (GAS) Gram stain.
Species of Streptococci are characterized by a combination of growth characteristics and Lancefield grouping that is based on types of capsular polysaccharide. The Lancefield group largely apply to the beta-hemolytic streptococci (exception is group D). Streptococci are part of the normal human flora (skin, mucous membranes, and GI and GU tracts).
S. pneumoniae has a prominent capsule which is primary virulence factors. It is spread via respiratory droplets and the upper respiratory tract mucosa is its preferred habitat. After colonizing the pharynx, invasive disease can occur. It is the most common cause of community acquired pneumonia and bacterial meningitis in adults. Less serious infections include sinusitis and otitis media, with S. pneumoniae being the most common bacterial cause of these illnesses in children.
Most S. pneumoniae is susceptible to penicillin, but alterations in penicillin-binding-proteins can occur leading to high-level resistance. For serious infections, third generation cephalosporins with/without vancomycin is recommended.
GAS is transmitted from human to human via respiratory droplets and the throat is preferred habitat. There are several toxins and virulence factors that facilitate human diseases. Diseases are characterized as:
-
- Suppurative (pharyngitis and cellulitis) and
- Non-suppurative (rheumatic fever and acute glomerulonephritis)
Suppurative infections are due to exotoxins that cause tissue damage. Scarlet fever is caused by erythrogenic toxin which acts as a super-antigen and can lead to toxic-shock syndrome.
The non-suppurative complications are immunologic phenomena in which antibodies to Streptococci M protein cross react with endovascular and joint tissues.
GAS remains susceptible to penicillin.
“Viridans” refers to the green color of hemolysis. There are many species in this group, though many clinical labs may not identify the organism to the species level. Normal flora of the oral cavity and gingiva. They have low virulence. Clinical infections occur when bacteria gain access to bloodstream (e.g., gingival disease, dental procedures). Hematogenous seeding of cardiac valves causes endocarditis, the most important disease of viridans strep. Infections in bones, joints, or implanted prosthetic devices can also occur. Polymicrobial infections of the deep neck space or brain abscesses typically include Viridans strep.
Most viridans strep are susceptible to penicillin. Aminoglycosides are frequently added for synergy in treatment of endocarditis.
A normal commensal in the genitourinary and vaginal mucosa, the most problematic infection occurs in neonates who are exposed to the organism during birth. GBS is the leading cause of neonatal sepsis and meningitis in the first year of life. Clinical disease in adults is uncommon; when reported, it is most often linked to urinary tract infections and chronic wound infections in persons with diabetes.
Enterococcus
Normal commensal of the GI, biliary, and GU tracts.
It has low virulence. There are two species, E. fecalis and E. faecium; the former is most commonly encountered in clinical disease. Infections occurs when natural defenses or barriers are impaired (e.g., GU or GI procedures), which can allow entry to blood stream and hematogenous spread. Endocarditis is rare, but the most serious infection due to enterococcus. Enterococcus is frequently involved in intra-abdominal or biliary infections (e.g., post-surgical or cholecystitis).
Enterococcus species have natural resistance to many antibiotics. Ampicillin is preferred treatment for susceptible E. fecalis strains. Resistant strains are treated with Vancomycin. Vancomycin resistance (VRE) is an increasing problem with limited options for treatment of serious infections.
Gram-Positive Rods (GPRs)
Clostridia
Clostridium tetani.
Spore-forming anaerobic bacteria that are ubiquitous in environment and several species are commensal anaerobes in the gut microflora.
The spectrum of diseases caused in humans is related to the type of exotoxin produced by the species and the target of those toxins. The species most commonly implicated in human diseases are detailed here.
Clostridium botulinum is normally found in soil and is the causative agent of botulism. Botulism can be produced by ingestion of food contaminated with C. botulinum toxin or spores (commonly improperly canned foods and infants who are given honey) or inoculation of Botulinum toxin into wound. Botulinum toxin is a heat-labile protease that prevents fusion of the synaptic vesicle and release of acetylcholine from the motor neuron. The result is a failure of muscle contraction and flaccid paralysis.
Botulism is a category A bioterrorism agent/disease and the deadliest toxin in the world.
Clostridium tetani is normally found in the soil and is the causative agent of tetanus when spores are introduced, usually into a wound or other appropriate environment for germination and production of tetanospasm toxin. Microscopically, spores are terminally located, given the appearance of a tennis racket. Tetanus toxin is a protease that prevents the fusion of the synaptic vesicle and release of GABA from inhibitory neurons. The result is constitutive and unopposed stimulation from motor neuron and extreme muscle spasm. Toxoid vaccine is effective at prevention.
Clostridium perfringens is normally found in soil and within the human colon. It is considered the “toxin-master” due to numerous and virulent toxins that it may produce. The primary clinical diseases caused by C. perfringens are myonecrosis (gas gangrene) and food poisoning. The latter is due ingestion of vegetative organisms that germinate and produce enterotoxin within the GI tract. Necrotizing infections are due to several toxins that destroy connective tissues. Alpha-toxin, or “lethal toxin,” a lecithinase, is implicated in massive tissue destruction. Necrotizing infections of organs in the GI tract or Gyn structures are part of the spectrum of invasive C. perfringens diseases.
Clostridium difficile is found in the human colon. Clinical disease usually results after the normal diversity of GI microflora is disrupted with antibiotics, allowing C. difficile to overgrow and produce large amounts of disease-producing toxins. Clinical disease ranges from febrile diarrhea to pseudomembranous colitis to septic shock with multi-organ failure. Exotoxins A and B are implicated in disease. Toxin B is considered most virulent as it causes apoptosis of enterocytes.
Treatment options include:
-
- Oral vancomycin (IV is not effective)
- Fidaxomicin
- Metronidazole
- Fecal transplantation
Clostridium septicum is similar to C. perfringens as cause of gas gangrene and produces similar toxins. It is more frequently associated with spontaneous gas gangrene (as compared to traumatic gas gangrene of C. perfringens). Endogenous/GI source is most commonly implicated as origins of disease and the diagnosis of C. septicum gas gangrene should prompt an evaluation of the GI tract for disease or malignancy.
Bacillus
Large ‘box-car” shaped aerobic spore-forming gram-positive rod that forms short or long chains; spores when seen are centrally located.
Species with major relevance to human disease are B. anthracis and B. cereus.
Bacillus cereus is found in soil and vegetation. It causes toxin-mediated food poisoning which is rapid in onset.
-
- Most notable is the emetic form that begins 1–5 hours after ingestion of pre-formed toxin in fried rice, milk, or pasta. This form is characterized by nausea, vomiting, and abdominal cramps.
- A diarrheal form with onset of 1–24 hours results from ingestion of vegetative cells in improperly prepared food that sporulate within GI tract and produce toxin leading to diarrhea and abdominal cramping.
Symptoms are mostly self-limited. Invasive disease due to B. cereus is rare, but can be seen in the severely immunosuppressed.
Bacillus anthracis‘s usual habitat is soil, but it can be transmitted to humans by contact with infected animals or inhalation of spores. The inhalational route of transmission makes anthrax a Category A bioterrorism agent/disease. The main clinical manifestation of disease are:
-
- Cutaneous
- Injection site (PWID)
- Gastrointestinal/mucosal
- Pulmonary
Disease is due to the Anthrax toxin, which is made of three parts:
-
- The protective antigen
- The edema factor
- The lethal factor.
Hallmark finding for cutaneous anthrax is a progressive papule that develops into a necrotic ulcer with central black eschar. Edema and regional lymphadenopathy are common.
Inhalational anthrax causes hemorrhagic mediastinitis with radiographic widening of the mediastinum. Mortality from inhalational anthrax with respiratory failure is very high (>80%).
Corynebacterium
Clubbed or irregularly shaped aerobic gram-positive rods, commonly called “diphtheroids” and sometimes described as resembling characters of the written Chinese language.
There are over 80 species, most of which represent normal flora of the skin microbiome. C. diphtheriae is of importance in human disease.
Corynebacterium diphtheriae colonizes the human throat and is transmitted via respiratory droplets. Disease is mediated by diphtheria-toxin, a heat-labile exotoxin that inhibits ADP-ribosylation and protein synthesis. Death of mucosal epithelial cells causes the grey pseudomembrane that is the hallmark of diphtheria pharyngitis. Vaccination with TDaP (tetanus, diphtheria, and acellular pertussis) is effective prevention. Penicillin is the treatment of choice.
Listeria monocytogenes
Small aerobic gram-positive rod that exhibits “tumbling motility” and moves intracellularly from cell-to-cell via ‘actin rockets.’
It can colonize the GI and female genital tract and is usually introduced from food sources (dairy and processed meats most frequently implicated). Clinical manifestations of disease include:
-
- Febrile gastroenteritis
- Meningitis (neonates and age >65 or immunosuppressed)
- Neonatal sepsis
Treatment is ampicillin (with or without gentamicin).
Lactobacillus
Facultative anaerobic gram-positive non-spore-forming rod.
They are an important component of the human microbiota in the GI tract, urinary system, and genital system. They are mutualistic and provide protection to the human host by protection against potential pathogens.
Gardnerella vaginalis
Facultative gram-variable rod.
In the dysbiosis, bacterial vaginosis (BV), Gardnerella bacteria can be seen encasing vaginal epithelial cells on a wet-mount. These are referred to as “clue cells” and, in the right clinical setting, are diagnostic of BV.
Branching gram-positive rods
Nocardia asteroides
Aerobic, gram-positive filamentous branching rods that occur naturally in the soil.
Nocardia are weakly acid fast and can be better identified with a modified acid-fast stain compared to gram stain. Clinical disease is most frequently seen in immunocompromised persons. Disease results from aspiration of organisms into the lungs with subsequent hematogenous spread. CNS disease with brain abscess is the next most common infection. Prolonged treatment with trimethoprim-sulfamethoxazole is recommended.
Actinomyces israelii
Anaerobic filamentous gram-positive branching rod.
Actinomycetes are common commensals of the oral-gingival mucosa and GI tract. Clinical disease results when organism is transmitted to tissues through trauma, procedures, devices (e.g., IUD), or aspirated from the mouth into the lungs. The hallmark clinical findings are chronic abscess with draining sinuses and sulfur granules seen on microscopic evaluation of the drainage.