These bacteria do not conform to the typical gram-positive and gram-negative distinctions, largely due to differences in their cell walls. Their ecologic niche, types of diseases, and immune response are resultantly different as well.
Spirochetes
Spiral shaped bacteria. While cell wall structures are technically similar to gram-negative bacteria, most are far too thin to be seen with traditional gram stain. Spirochetes are well-represented in the normal human flora of the mouth and GI tract.
Treponema pallidum
Cannot be cultured in laboratory conditions.
It is restricted to humans as the causative agent of syphilis. Transmission is by sexual contact and from mother-to-fetus across the placenta. After infection, T. pallidum distributes widely throughout the body with predilection for central nervous system, vascular endothelium, bones, muscles, and skin.
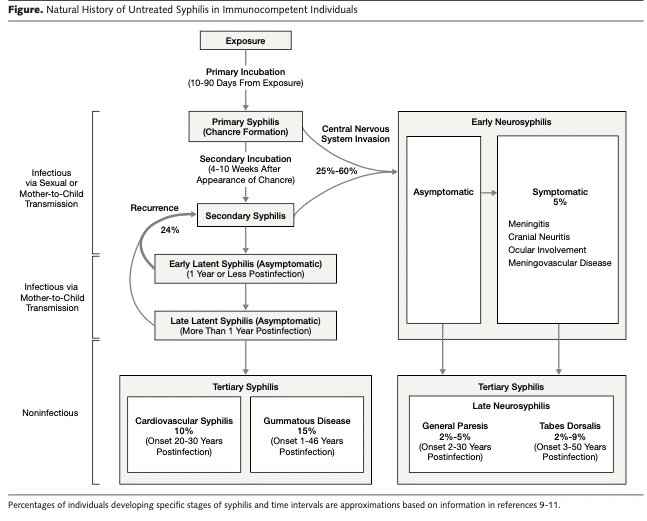
Sexually transmitted syphilis is divided into early and late phases based on time since transmission with three distinct clinical entities:
-
- Primary syphilis presents as a painless chancre
- Secondary syphilis occurs at onset of spirochetemia
- Tertiary syphilis is characterized by late manifestations.
Note that neurologic involvement with meningoencephalitis or uveitis can occur at any time.
Notable clinical entities of syphilis include:
-
- Painless chancre
- Aortitis
- Tabes dorsalis
- General paresis
- Argyll Robertson pupillary defect
Diagnosis of syphilis relies on a combination of nontreponemal testing (RPR, VDRL) and treponemal specific antibody testing
Treatment is Penicillin. Route and duration of treatment depend on stage of disease.
Links related to this section
Borrelia
Long, slender spirochetes with multiple axial flagella in loose spirals that give organism an irregular wave like appearance microscopically.
Unlike other spirochetes, Borrelia can be demonstrated with common Giemsa or Wright stains. Distinctively, their genome is split between one large chromosome and multiple plasmids. This feature is allows for significant antigenic variation and results in the clinical manifestation of relapsing fevers. There are over 15 species that can cause human disease. The most important to know are B. burgdorferi, B. recurrentis, and B. hermsii.
Causes Lyme disease which is transmitted to humans through the bite of the ixodes tick (deer tick), which acquire the bacteria in blood meal from the white-footed mouse, the main reservoir. The tick must be attached for 24 hours to effectively transmit the bacteria. Geographic restrictions of clinical disease reflect the geography of reservoir and vector and may change with changing climate. The vast majority of cases in the US occur in the Northeast and Midwest.
Like other spirochetes, after initial inoculation, widespread dissemination occurs. Clinical disease is divided into three stages.
-
- Early infection is characterized by erythema migrans, a targetoid cutaneous lesion around site of tick-bite.
- Disseminated infection or spirochetemia can be associated with meningitis, neuropathies, and cardiac arrythmias.
- Late or persistent infection can lead to inflammatory arthritis, and chronic neurologic sequelae.
Treatment is effective: doxycycline is recommended for early disease and ceftriaxone for disseminated or late disease.
The cause of epidemic relapsing fever. Humans are only known reservoir and the vector is the human louse. Humans are infected when lice are scratched, crushed, and inoculated into skin.
The cause of endemic relapsing fever.
Small mammals, especially rodents, are the reservoir, and infections are transmitted to humans through the bite of the soft tick (Ornithodoros).
Leptospira interrogans
Thin, tightly coiled, and highly motile spirochete.
It has worldwide distribution in mammals, especially dogs and rats, and is excreted from animals into urine. It can survive for prolonged periods in water where humans can be infected across small breaks in skin or mucosal surfaces. Outbreaks are particularly common in tropical areas that are prone to flooding.
Clinical disease manifestations are related to endothelial activation and disruption of endothelial cell connections. Initial bacteremic phase is characterized by fever and myalgias; conjunctival suffusion is a common association. The second, immunopathologic phase is uncommon but has severe manifestations of meningitis, liver dysfunction, renal failure, and DIC with pulmonary hemorrhage (Weil’s syndrome).
There is no known antimicrobial resistance: Penicillin and Doxycycline are effective.
Chlamydia
Obligate intracellular bacteria that lack peptidoglycan.
Their replicative cycle has two forms:
-
- The elementary bodies (EB) are the infectious form that are metabolically inactive but can survive extracellularly.
- Reticulate bodies (RB) form when EBs are endocytosed and are the metabolically active replicative form.
Major human pathogens are Chlamydia trachomatis and Chlamydophila species.
C. trachomatis
Causes disease in several sites, primarily genital tract and conjunctiva.
Humans are the sole reservoirs, and it is estimated to be the most frequent infection in the world with 100 million new cases a year. C. trachomatis has three biovars with distinct tissue tropism. Demonstration of bacteria requires intracellular cultivation and is not commonly done in commercial labs. Nucleic acid amplification tests are preferred.
Infect ocular epithelial cells and is the cause of trachoma, the most common cause of blindness worldwide.
It is a chronic follicular conjunctivitis that is contracted in infancy or childhood by contact with human secretions (hands, fomites, or flies). Blindness results from chronic corneal irritation and scarring.
Infect urogenital epithelial cells.
Transmission is via sexual contact and causes urethritis, epididymitis, mucopurulent cervicitis, and pelvic inflammatory disease. Neonatal acute inclusion conjunctivitis can occur when the baby is exposed to bacterial during birth, but it is not usually associated with permanent damage or vision loss.
Links to related sessions
-
Coming soon!
Infect urogenital and colorectal epithelial cells.
Transmission is via sexual contact, and Lymphogranuloma venereum results. Geographically, L1–3 is found more commonly in tropical areas of Caribbean, South America, Africa, and Southeast Asia. The primary lesion of LGV is often asymptomatic transient papule or ulcer. Progression to multilocular suppurative inguinal lymphadenopathy then follows and is typically the chief complaint. Draining fistulae can develop, and related systemic symptoms are common. Hemorrhagic ulcerative proctitis can occur if infection through anal route.
Links related to this section
-
Coming soon!
Chlamydophila psittaci
Zoonotic disease from exposure to poultry or other birds.
It causes an atypical pneumonia with fevers, myalgias, dry cough, and bilateral interstitial infiltrates. The organism, while not highly virulent, is highly infectious. It is category B bioterrorism agent/disease and is not frequently cultivated in diagnostic laboratories due to risk to personnel. Serology is preferred method of diagnosing infection.
Chlamydophila pneumoniae
Common cause of community-acquire pneumonia, similar to Mycoplasma pneumoniae.
It can be spread person-to-person. It causes an atypical pneumonia with fevers, myalgias, dry cough, and interstitial infiltrates. Disease is generally not severe, but cough may persist for weeks.
Azithromycin is the preferred treatment for Chlamydial infections.
Rickettsia
Obligate intracellular parasites that are not seen well on gram stains and are better demonstrated by immunofluroescence.
They technically have structures similar to gram-negative bacteria, including LPS. The major human pathogens have tropism for vascular endothelial cells, leading to severe disease with vasculitis and distributive shock due to increased vascular permeability. They can only be grown in cell cultures or embryonated eggs. Most rickettsiae have animal reservoirs and are transmitted to humans by arthropod bites. Major human pathogens to know are:
-
- The spotted fever R. rickettsia (other species of spotted fevers are endemic in eastern hemisphere)
- Typhus group R. prowazekii, R. typhi, and O. tsutsugamushi
R. rickettsia
Cause of Rocky Mountain Spotted Fever (RMSF).
The tick is the main reservoir and vector:
-
- In the Eastern U.S., the dog-tick (Dermacentor) predominates
- In the South and West, the Lone Star tick is implicated.
 Clinical infection presents with acute onset of fever, headache, rash, confusion, and myalgia. Rash demonstrates distinct pattern that begins with macules that become petechiae and spread from the wrists and ankles upwards and involve the palms and soles.
Clinical infection presents with acute onset of fever, headache, rash, confusion, and myalgia. Rash demonstrates distinct pattern that begins with macules that become petechiae and spread from the wrists and ankles upwards and involve the palms and soles.
Treatment is with doxycycline. Prompt recognition and treatment is required, as mortality without treatment or with treatment delay is high.
Epidemic typhus and is transmitted by the human louse when louse feces are scratched into recent bite wound. War, extreme poverty, and crowding promote epidemics.
Endemic typhus or murine typhus and is transmitted via the rat flea. Humans are incidental hosts. Human incidence is ties to quantity of urban rodents. Severe disease is uncommon
Cause of scrub typhus and is found predominantly in South Asia, China, and Indonesia. Mites/chiggers are the reservoir and vector; humans are incidental hosts when they encounter the arthropods in the scrub brush or low hanging trees.
Anaplasma phagocytophilum
Along with Ehrlichia, is a tick-borne gram-negative bacteria that is commonly grouped with the rickettsia, though cellular structures differ. Anaplasma is spread by the Ixodes tick and has similar distribution to Lyme disease. Their cellular wall does not contain LPS or peptidoglycan, but they can independently meet basic metabolic tasks. They are obligate intracellular parasites, and Anaplasma preferentially infect PMNs, causing the disease human granulocytic anaplasmosis. Disease is similar to RMSF minus the rash. Cytopenias are frequent. Intragraunlocytic inclusions, ‘morulae,’ are the hallmark finding on peripheral smear, though clinically not always apparent. Look out for co-infection with other diseases spread by Ixodes.
Doxycycline in the treatment of choice.
Links related to this session:
Ehrlichia chaffeensis
Along with Anasplasma, is a tick-borne gram-negative bacteria that is commonly grouped with the rickettsia, though cellular structures differ. Ehrlichia is spread by the Amblyomma (Lone star) tick and is found in southern states. Their cellular wall does not contain LPS or peptidoglycan, but they can independently meet basic metabolic tasks. They are obligate intracellular parasites, and Ehrlichia preferentially infect Monocytes, causing the disease human monocytic ehrlichiosis. Disease is similar to RMSF minus the rash. Cytopenias are frequent. Intramonocytic inclusions, ‘morulae,’ are the hallmark finding on peripheral smear, though clinically not always apparent.
Doxycycline in the treatment of choice.
Links related to this session:
Mycoplasma pneumoniae
Most relevant species in Mycoplasma genus to human disease.
Mycoplasma is the smallest free-living organism and uniquely lacks a cell wall, which means it does not take any gram stain. While it can be cultured in lab conditions, this is rarely done in diagnostic labs, and PCR or serologic methods are more commonly employed. Habitat of M. pneumoniae is the human respiratory tract, where it is the most common cause of atypical community acquired pneumonia, also called “walking pneumonia.” Antibodies to Mycoplasma can cross react with RBC surface proteins, leading to mild hemolytic anemia and cold agglutinins. If cold agglutinins are found in patient with pneumonia, Mycoplasma can be inferred as the diagnosis.
Treatment is with macrolide or tetracycline. Cell-wall active agents have no effect since there is no cell wall.
Links related to this section
Mycobacteria
Nonmotile, non-spore-forming, obligate aerobes.
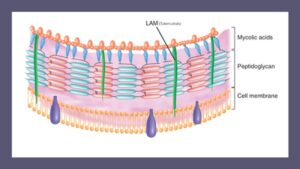 The abundance of long-chain fatty acids called mycolic acids are of particular importance as a microbiologic feature and for their role in pathogenesis and immunity. This gives a waxy coat to the bacteria, which confers protection and makes them “acid-fast” on staining—after prolonged exposure to stain and penetrating agents, the stain is “fast” and does not decolorize. Classification of mycobacteria are based on phenotypic characteristics, growth rates, pigmentation of colonies, and fatty-acid profile of the cell wall.
The abundance of long-chain fatty acids called mycolic acids are of particular importance as a microbiologic feature and for their role in pathogenesis and immunity. This gives a waxy coat to the bacteria, which confers protection and makes them “acid-fast” on staining—after prolonged exposure to stain and penetrating agents, the stain is “fast” and does not decolorize. Classification of mycobacteria are based on phenotypic characteristics, growth rates, pigmentation of colonies, and fatty-acid profile of the cell wall.
Disease caused by mycobacteria are typically slowly evolving, follow a chronic course, and elicit a granulomatous response. Granuloma formation is a key pathologic finding in mycobacterial disease and is mediated by IFN-γ, TNF-α, CD4 cells, and activated macrophages. Defects in cell-mediated immunity or TNF-α inhibitor use are major risk factors for disease.
Relevant mycobacteria can be made into three categories that cause clinically distinct diseases:
-
- Tuberculosis
- Leprosy
- Non-tuberculous mycobacteria
Links related to this section
Mycobacterium tuberculosis
Very slow growing acid-fast bacilli that is restricted to human hosts where the highly aerobic environment of the lung is preferred site.
While millions of people are exposed to TB every day worldwide, disease due to MTB is actually the exception, rather than the rule.
Transmission from human-to-human is through respiratory droplets.
-
- After inhalation, organisms replicate in alveoli
- Alveolar macrophages ingest organism, where MTB may resist digestion by the lysozome.
- Bacteria are then transmitted to regional and hilar lymph nodes (this is primary tuberculosis infection).
- Bacteria then disseminate throughout the body via lymphatic drainage into the blood stream.
While the upper lobes of the lungs are preferred location for on-going replication, the organism can seed bones, lymph nodes, visceral organs, and even CNS.
After dissemination, Th1 cellular immune responses respond to organisms with granulomatous inflammation that can essentially “wall-off” organisms within a granuloma. MTB may then enter a metabolically inactive state within the granuloma (this is latent infection). If the Th1 response is inadequate, progressive tissue destruction and disease can occur.
Failure to maintain immunologic control of the bacteria due to advancing age, immunosuppression, malnutrition, smoking, or other impairments to cell-mediated or heightened delayed-type-hypersensitivity response can lead to reactivation which develops at the site of granuloma. In the upper lobes, cavitary lesions can develop, organisms multiply and accumulate, then are coughed up to spread to another person.
Diagnosis of latent tuberculosis relies on measurement of delayed-type hypersensitivity response. Purified protein derivative (PPD) skin testing or interferon-gamma-release assays are used. Treatment of latent infection with isoniazid or rifampin for several months can prevent later reactivation and disease.
Diagnosis of active disease requires evidence of organism in acid fast smear, MTB culture, or nucleic acid amplification tests. Treatment of active disease must be prolonged and requires multiple agents. The most common combination is “RIPE”: rifampin, isoniazid, pyrazinamide, and ethambutol.
BCG vaccination programs in endemic areas may limit the morbidity/mortality of disease, but they have not effectively reduced the global burden of TB disease.
Mycobacterium leprae
Slow-growing acid fast bacilli with human reservoir, though also found in armadillos.
Optimal growth occurs at cooler temperatures, and preferred sites of infection include the skin of the nose, ears, superficial nerves, and extremities with cooler temperatures. Transmission from human-to-human is through nasal secretions and requires close and frequent contact.
Clinical manifestations are entirely dependent on the host immune response and there is a spectrum between Lepromatous (Th2 response) and Tuberculoid (Th1 response) leprosy. Tuberculoid leprosy presents with hypopigmented and anesthetic lesions on the skin. In lepromatous leprosy, dermal infiltration leads to nodular lesions and “leonine facies” and peripheral neuropathies. Digital loss is due to recurrent trauma of insensate fingertips.
Multi-drug treatment must be prolonged. Dapsone, Rifampin and Clofazimine are drugs of choice.
Links related to this section
Non-tuberculous mycobacteria (NTM) or atypical mycobacteria
Diverse group of species that cause diverse diseases.
Organisms are described as “fast-grower” or “slow-grower” based on whether they form colonies in culture in more or less than 7 days. They are found in natural environments (soil, water, sea water, etc.), and human-to-human transmission does not occur. There are over 140 different species of NTM with geographic differences in prevalence. Antibiotic resistance is frequently encountered.
Distinct clinical entities are associated with certain species, and these are worth noting. Types of clinical disease can be grouped into:
-
- Muco/cutaneous infection
- Pulmonary infections
- Lymphatic
- Disseminated
Links related to this section
Slow grower that is ubiquitous in environment.
It causes:
-
- Pulmonary infection, usually in persons with bronchiectasis or bullous lung disease, that mimics MTB clinically
-
Hypersensitivity pneumonitis (“hot tub lung”)
-
Lymphadenitis
-
Disseminated infection in persons with AIDS when CD4 count drops below 50–100.
Can mimic MTB pulmonary infection.
Water-loving intermediate grower that causes cutaneous granulomatous lesions at sites of abrasion and contact with swimming pool or aquarium water.
It can be associated with regional lymphangitis and lymphadenopathy.
Causes lymphadenitis, knowns as “scrofula.”
Rapid grower that is water loving and has been linked to infections of prosthetic joints and in dwelling vascular catheters.
It can cause cutaneous infections and has been linked with outbreaks related to pedicure water and tattoo ink.
Third-most common mycobacterial infections worldwide and found in tropical, warm climates.
Infection is likely due to exposure of water source. Infection causes debilitating ulcers (termed “Buruli ulcer” for the location in Uganda where it was first described). Ulcers are generally painless, but progressive and erode deeper mechanical tissues, including osteomyelitis.