The pre-work for this learning activity should take no more than 1 hour to complete.
Welcome
Please complete this module to prepare you for your upcoming interprofessional education (IPE) session. This preparation should be completed prior to your IPE session.
At the end of this module, you will download a profession specific encounter on an error disclosure. Please review and save this document as we will utilize the case during the live session.
Get the learning objectives on E.Flo MD
The Peripheral Vascular System
Get the learning objectives on E.Flo MD
Upper Respiratory System
Acknowledgments
The materials for this session were adapted from:
- Ryan Murphy, Suzette Goucher, Carrie Sullivan, Amanda Moloney-Johns, Christina Derbidge, Jared Henricksen. How to Disclose Medical Errors and Unanticipated Outcomes. Accelerate University of Utah Health curriculum (2021).
- Implementation Guide for the CANDOR Process. Content last reviewed August 2022. Agency for Healthcare Research and Quality, Rockville, MD.
Co-Authors
Jennifer Robinson, PharmD
Taylor Bertsch, PharmD
Introduction
To be human is to err.
Alexander Pope
Every practicing health care provider, even the most careful, will be involved in errors that impact patients and patient care outcomes. As health care providers, we have a responsibility to take ownership of our errors, learn from them, and be transparent disclosing errors to those impacted. Timely and clear disclosure builds trust with patients and families and reduces the risk of litigation.
How do errors occur?
- An error can occur because of incomplete knowledge or information.
- Sometimes there is an error in judgment or lapse of attention.
- The environment and the culture of an organization can lead to errors.
- Lack of sleep, an overwhelming amount of work, and distractions can increase the likelihood that an error can occur.
What is disclosure?
Disclosure is the act of revealing information to a patient or family. It is a process, not an isolated occurrence—especially after serious events.
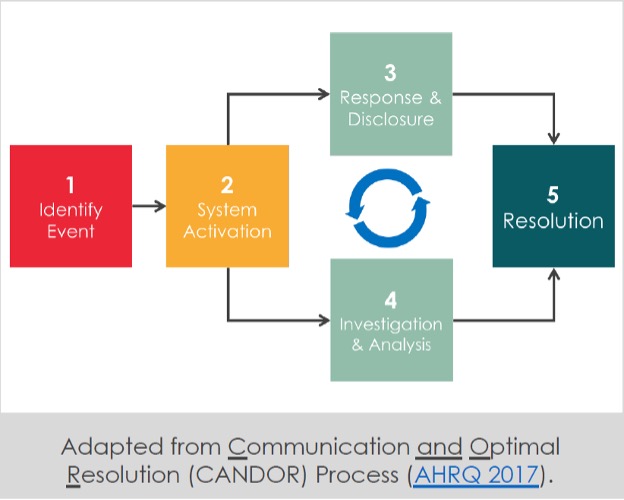
Whether the patient suffers an unanticipated outcome without clear fault or a true medical error, the process can include multiple cycles of response, disclosure, investigation, and analysis before ultimately achieving resolution. The initial disclosure conversation should be held as soon as possible and will set the tone for subsequent investigation and follow-up.
How to disclose
When disclosing a medical error, there are some unique challenges.
There are general strategies to help deliver bad news that should be followed, but disclosure of medical errors presents some unique challenges.
- Health care professionals may be embarrassed.
- Unsure of what to say.
- Nervous about legal liability.
As a result, disclosure of medical errors may be perceived as incomplete (“partial disclosure”) or may never happen. This not only fails to fulfill our responsibility for clear and consistent communication, but often leads to the very lawsuits providers hope to avoid.
Health care professionals should be careful not to admit or assign fault prematurely or inappropriately. A thoughtful and coordinated disclosure approach that includes the system and an investigation can be helpful when determining how best to respond (see the CANDOR process below). Multiple organizations have found that efforts to reform their disclosure practices increase transparency and reduce litigation costs.
In the state of Washington, health care providers have protections that allow for early disclosure and the implementation of measures to address an error. The legislature “prioritizes patient safety and the prevention of medical errors above all other considerations as legal changes are made to address the problem of high malpractice insurance premiums. Thousands of patients are injured each year as a result of medical errors, many of which can be avoided by supporting health care providers, facilities, and carriers in their efforts to reduce the incidence of those mistakes. It is also the legislature’s intent to provide incentives to settle cases before resorting to court.” Disclosure of an error through an apology, condolence, or expression of compassion, and an offer to take action to address the act of omission in the first 30 days following an incident are encouraged and protected by law (RCW 5.64.010).
The disclosure process recommendations from the Agency for Healthcare Research and Quality helps individuals and the organization time to respond to patients and families in a timely, thorough, and just manner.
Five steps to successful disclosure
The following Five Steps to Successful Disclosure are recommended for the initial disclosure meeting after a medical error or unanticipated outcome:
Ask for and host a conversation.
Don’t wait! Do this as soon as possible after the event is discovered. Gather as much information as possible for the patient and family. Consider which members of the patient’s personal support system should be present. Identify which members of the health care team should take part in the disclosure with you. The attending provider should be present if possible, but you may not be able to wait.
- Set the stage: Find a private and quiet place to meet.
- Know and use the patient’s name.
- Introduce yourself and any other individuals in attendance.
- Sit down.
- Minimize distractions.
Prepare the patient/family for a serious conversation.
- Make an opening statement.
- Start from the beginning and prepare the patient/family with a shot across the bow: “There has been an unanticipated event in your care, and I am here to tell you everything I can.”
- Share the information you know.
- Explain objectively what occurred: “You did not receive the antibiotics we intended to give you last night.”
- Make factual conclusions and resist the urge to speculate on what may have happened.
Invite questions and listen openly.
- Listen—allow silence, explore emotion.
- After sharing a sentence or two about the event, ask if they are ready to hear more details.
- Allow time for a response.
- Throughout this conversation, there may be comments or behaviors reflecting grief responses such as anger or disbelief.
- Assess understanding. Depending on the situation, patients and families may misinterpret or not hear information discussed.
- Be ready to repeat information or give information in another way if needed.
- Encourage patients and families to ask questions so they gain understanding.
- Anticipate varied responses from different people. Be prepared to listen and offer support.
Allow yourself to be vulnerable.
- Vulnerability is sincerity—it’s okay to feel uncomfortable. You should offer words of apology and condolences such as, “I am sorry this happened.” Apologize more than once.
- When appropriate, use phrases of reassurance such as, “We are going to take care of you.”
- Avoid blame. Be careful not to prematurely assign blame with phrases like “we screwed up” or “this is _____’s fault.” Subsequent conversations after additional investigation will better address this.
Discuss the next steps in caring for the patient.
You can reassure patients they will receive the ongoing medical care they need: “We will monitor you closely and provide any further care you need.”
Discuss the next steps for investigation and prevention of recurrence.
If certain details remain unclear, explain that further investigation will take place. You can assure the patient that results of this investigation will be shared with them and inform specific actions to prevent a similar event from happening again.
Discuss who will speak to the patient/family next and when.
Identify a contact for patients and families who will manage follow-up communication to discuss the situation. Be as specific as possible.
For Patients and Families
- Offer support services to the patient/family. Consider inviting a behavioral health provider or clergy to the meeting. Otherwise, offer to facilitate services afterward.
- Navigate a patient death.
- If a patient dies unexpectedly, be sure to use the word “dead,” “died,” or “death” to be clear about what you are saying.
- Use the patient’s name.
- Death of a patient is a significant event and will result in numerous coordinated actions from members of the health care team. Familiarize yourself with the process, leverage support services, and take your time to walk the family through the next steps.
For Providers and Teams
- Seek support for you and your team. Recognize the impact medical errors, especially those resulting in death, will have on you and your team.
- Health care providers can become the second victim of a medical error. Be proactive about seeking support from local resources like counseling services or risk management for any general assistance with disclosure or after any serious unanticipated outcome.
Questions
Which of the following statements would be an appropriate apology?
- “I take full responsibility” is not advised as it may cause liability issues and should not be used without council from legal representation or following an investigation to what occurred.
- “Frank caused the error” places blame on other members of the team, which is inappropriate.
Questions
When an error occurs, there can be a “second victim." Which of the following are examples of “second victims?"
Following a medical error, a health care provider can be overwhelmed with thoughts and feelings related to the incident. It is recommended that members of the health care team proactively seek care from counseling services or risk management following a serious event.
Determine cause and effect
Prepare to create your own fishbone diagram by watching the Institute for Health Improvement’s video tutorial Whiteboard: Cause and Effect Diagrams.
Questions
What are the main components of a fishbone diagram?
Fins and scales
Please try again
Bones and head
Correct!
Ribs and tail
Please try again
Questions
What information is included in the spines of the "fishbone?"
Error disclosure examples
When watching the disclosure examples, keep in mind the five steps of a successful disclosure. Pay attention to both verbal and non-verbal communication approaches that are used.
Inappropriate Disclosure to a Patient: Communication and Optimal Resolution (CANDOR)
Questions
Watch the above video and reflect: What went well, and what didn’t go well?
What went well?
- The provider was willing to have a conversation with the patient and appeared to have a previously established relationship.
What didn’t go well?
- The provider seemed to be in a rush and did not seem fully prepared for the conversation.
- There was no request if the patient wanted to have the conversation.
- The disclosure of the error was not clear and only disclosed based on additional questioning by the patient (Step 1: Set up).
- The patient’s emotional reaction was minimized by the provider, and he was told that “there is no reason to yell” (Step 2: Listen).
- The blame was placed with the nurse.
- The error was presented as not a big deal because there was “no permanent harm” (Step 3: Apologize).
- No next steps were discussed or identification of additional support (emotional, financial and medical) was not investigated (Step 4: Discuss and Step 5: Support).
Appropriate Disclosure to a Patient: Communication and Optimal Resolution (CANDOR)
Questions
Watch the above video and reflect: What went well, and what didn’t go well?
What went well?
- The provider disclosed that he would like to “talk about what happened last night” and asked if the patient was willing to talk for a few minutes.
- The provider sat down next to the hospital bed to be on the same level as the patient.
- The provider acknowledged that the night did not go well, but the patient was “back on track” (Step 1: Set up).
- Asked the patient open-ended questions including, “Can you say a bit about what happened last night”.
- The patient was allowed to talk and listened intently to his verbal and non-verbal responses.
- Toward the end of the video, the provider offered to reach out to the wife, who was briefly mentioned at the beginning of the conversation (Step 2: Listen).
- The patient’s emotional responses was validated, and the provider stayed calm as the patient was shouting.
- The provider took responsibility for the error that were the providers responsibility.
- The provider used “we” to talk about the responsibility of the entire team in providing care.
- The provider gave supportive comments for the nurse colleague when the patient voiced unhelpful assumptions (Step 3: Apologize).
- The provider had a willingness to be transparent, and briefly described the process that will occur to investigate the error and associated improvements to prevent a similar error from happening in the future (Step 4: Discuss).
- The provider offers the possibility of changing providers and continuing the conversation, with the inclusion of other individuals, to address concerns and minimize the impact of the error (Step 5: Support).
What didn’t go well?
- The error could have been disclosed earlier.
- The provider could have used the patient’s name more frequently during the conversation.
Disclosure Conversations with Family: Communication and Optimal Resolution (CANDOR)
Summary
As a health-care professional, you will make errors that result in negative patient outcomes. Your first reaction may be to respond with shame, anger, or disbelief. It is in these moments that we must remember that we are human, and our primary goal is to provide the best care possible. To provide excellent care, we must take errors as opportunities to be vulnerable and learn. Learning when and how our patient care systems and processes don’t work is of the utmost importance, so we can improve. Patients may understandably be upset and want answers. We need to be prepared for these difficult conversations by being adept at implementing the steps associated with successful disclosure.
Five steps of a successful disclosure
- SET UP the conversation.
- LISTEN and assess understanding.
- APOLOGIZE sincerely.
- DISCUSS next steps.
- SUPPORT for patient/family, you, and your team..
Upcoming IPE session patient case
Prior to your scheduled Error Disclosure IPE session, please download and review the following case. Save a copy of your case and bring it to the session.
Select your program of study:
Image credits
Unless otherwise noted, images are from Adobe Stock.