- Optional Reading
- Clinically Oriented Anatomy, 9th ed., Perineum section.
The perineum is the inferior-most region of the trunk, located between the thighs and buttocks. In the anatomic position the perineum is partially hidden because the thighs are together. When the thighs are abducted, the perineum has a diamond shape. Due to the forward tilt of the pelvis, the perineum faces anterior and inferior in the anatomic position. Therefore, clinicians often examine the perineum, and medical illustrations show the region, with the patient in the lithotomy position (patient supine with thighs flexed and abducted—see Figure 2 for example).
Boundaries
The pelvic diaphragm is the ceiling separating the perineum from the pelvic cavity. Inferiorly the perineum presents a free surface covered with skin and the external genitalia. The other boundaries of the perineum are those of the pelvic outlet:
- Anterior: Pubic symphysis
- Posterior: Coccyx
- Lateral: Ischiopubic rami, ischial tuberosities, sacrotuberous ligaments.
Subdivisions
A line drawn between the two ischial tuberosities divides the perineum into two triangles: the urogenital (UG) triangle and the anal triangle.
Urogenital triangle
This is a multi-layered compartment, consisting of two “pouches.” Each pouch is a potential space delimited by fascia. The contents of the pouches differ in the sexes, but overall their architecture is similar. Let’s discuss the common features first, then delve into the contents specific to each sex.
Architecture of the urogenital (UG) triangle common to both sexes
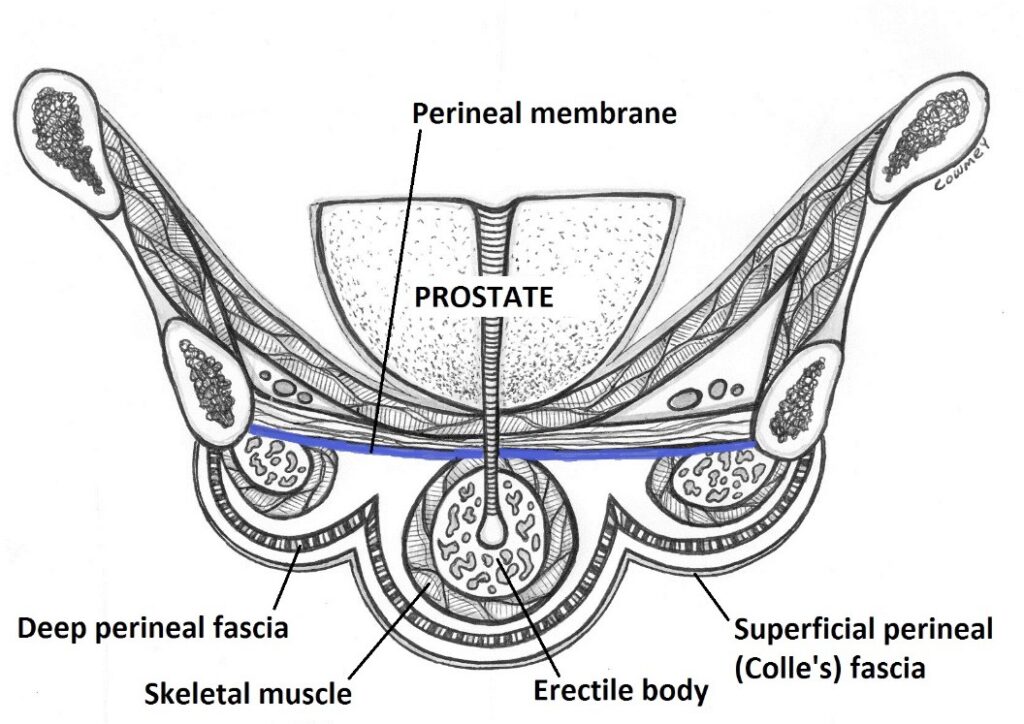
Fascia in the UG triangle
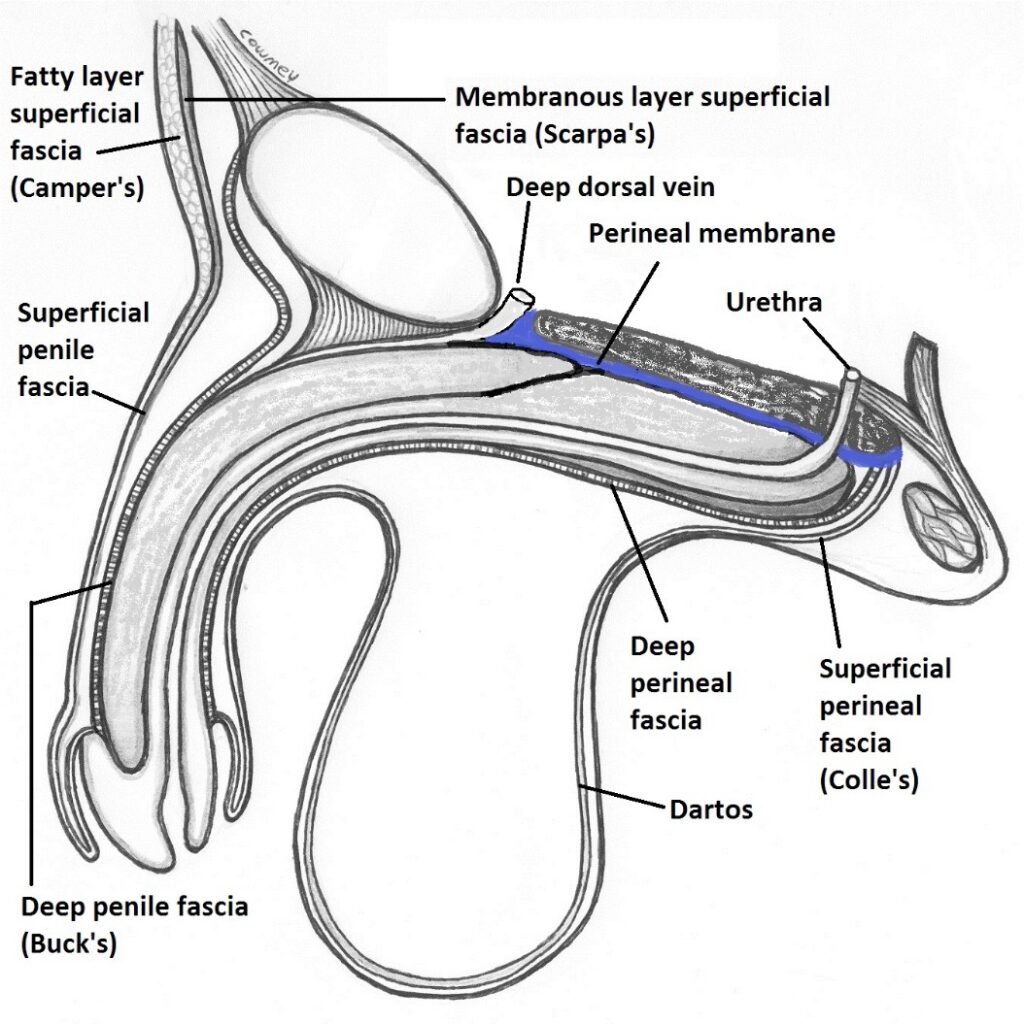
- Recall that the superficial fascia of the abdominal wall has a fatty layer (Camper’s) and a membranous layer (Scarpa’s). These layers are extended without interruption into the UG triangle of the perineum. In females, the fatty layer remains thick, especially over the mons pubis and in the labia majora. In males, the fatty layer is normally thinner, tapering down to practically nothing in the penis and scrotum. The membranous layer of superficial fascia in the UG triangle is called superficial perineal fascia (Colle’s fascia). The fatty layer has no name.
- Attachments of Colle’s fascia in the UG triangle:
- Anterior/superior: Continuous with Scarpa’s fascia of the anterior abdominal wall.
- Posterior: Fuses with deep perineal fascia at the posterior boundary of the UG triangle (the line connecting the two ischial tuberosities).
- Lateral: ischiopubic rami.
- Observe: Colle’s fascia is fixed along its posterior and lateral borders in the UG triangle. It is not fixed anterior/superior—thus the potential space deep to Colle’s fascia continues into the anterior abdominal wall.
- In the male, the superficial perineal fascia continues on to the penis (superficial penile fascia) and dips down into the scrotum (forming the dartos). In the female, the superficial fascia extends into the clitoris and is fused to the margins of the vagina.
- Deep perineal fascia is equivalent to the deep fascia that covers the oblique muscles of the abdominal wall. In the UG triangle, deep perineal fascia covers skeletal muscles and erectile bodies.
- Attachments of deep perineal fascia in the UG triangle:
- Same as Colle’s fascia, except anterior/superior, where it fuses to the pubic bones and symphysis pubis.
- Observe: Deep perineal fascia is not continuous with deep fascia of the abdominal wall—its continuity is interrupted by attachment to the pubic bones. Therefore, the potential space deep to the deep perineal fascia is sealed and not connected to any spaces in the abdominal wall.
- In the male, deep perineal fascia continues on to the penis, becoming the deep penile fascia (Buck’s fascia). It is not present in the scrotum. In the female the deep perineal fascia continues on to the clitoris.
- The perineal membrane is a robust layer of deep fascia stretched across the UG triangle superior to (above) the erectile bodies. It separates the superficial perineal pouch from the deep perineal pouch. Its attachments are the same as those of the deep perineal fascia.
- The erectile bodies of the male and female are fused to the inferior surface of the perineal membrane.
- The urethra in both sexes and the vagina in females penetrate the perineal membrane.
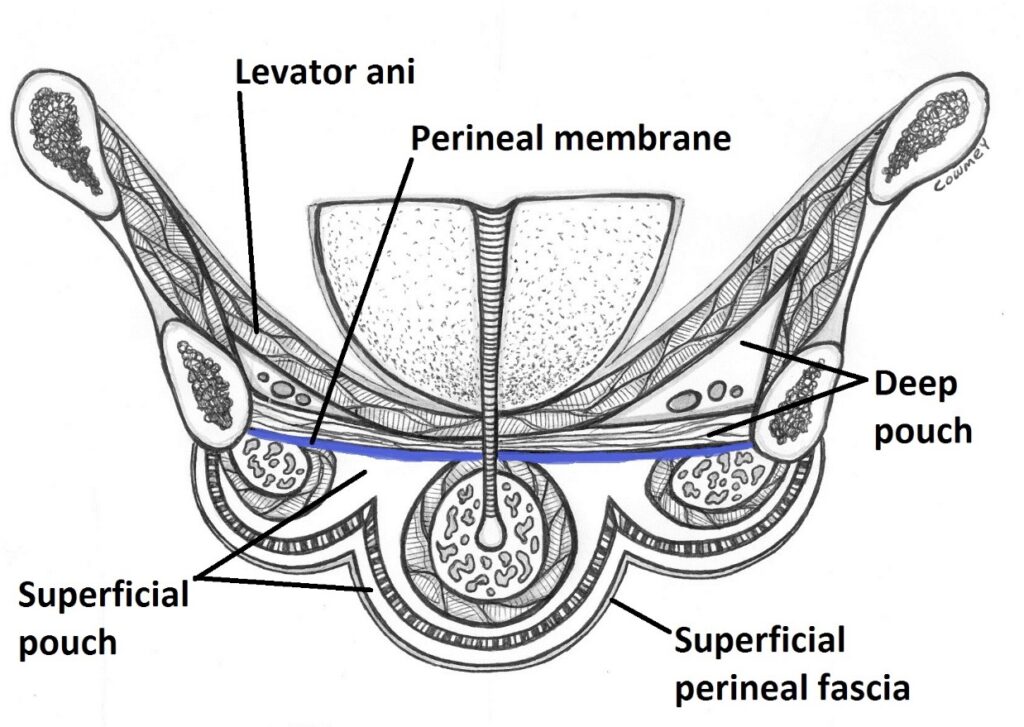
Perineal pouches
- Inferior (external) boundary: Superficial perineal (Colle’s) fascia
- Superior (deep) boundary: Perineal membrane
- Posterior boundary: Closed by the fusion of fascia along the posterior border of the UG triangle
- Lateral boundaries: Left and right ischiopubic rami
The presence of deep perineal fascia creates two compartments within the superficial pouch:
-
- Between Colle’s fascia and deep perineal fascia is a superficial compartment of the superficial pouch. The superficial compartment has no contents. This potential space communicates above with the potential space in the abdominal wall between Scarpa’s fascia and deep fascia on the abdominal muscles.
- Between deep perineal fascia and perineal membrane is a deep compartment of the superficial pouch. The deep compartment is closed. It contains skeletal muscles and erectile bodies.
The deep pouch is a bit nebulous and hard to visualize in the cadaver and in radiologic images. There is some controversy surrounding the composition of its contents.
-
- The upper (superior) part of the deep pouch is adjacent to the levator ani muscle (pelvic diaphragm) and is triangular when viewed in coronal section and contains fat.
- The lower part of the deep pouch is flattened and contains skeletal and smooth muscle.
- Anterior and lateral: The deep pouch is closed by the pubic bones and ischiopubic rami.
- Superior boundary (roof): The underside (inferior surface) of the levator ani muscles. The roof slopes from lateral to medial, so it is taller laterally.
- Inferior boundary (floor): Perineal membrane, pierced by the urethra and vagina.
- Posterior: The upper part (fatty part) communicates with the anal triangle, specifically with the fat-filled left and right ischio-anal fossae.
Clinical correlation
Urine leaking from a ruptured urethra in the bulb of the penis can leak into the superficial compartment of the superficial pouch if the deep perineal fascia is disrupted. This is called extravasation of urine (see Figure 6).
UG triangle in females
The urogenital triangle in the female contains the external genitalia and the contents of the superficial and deep perineal pouches.
Female external genitalia
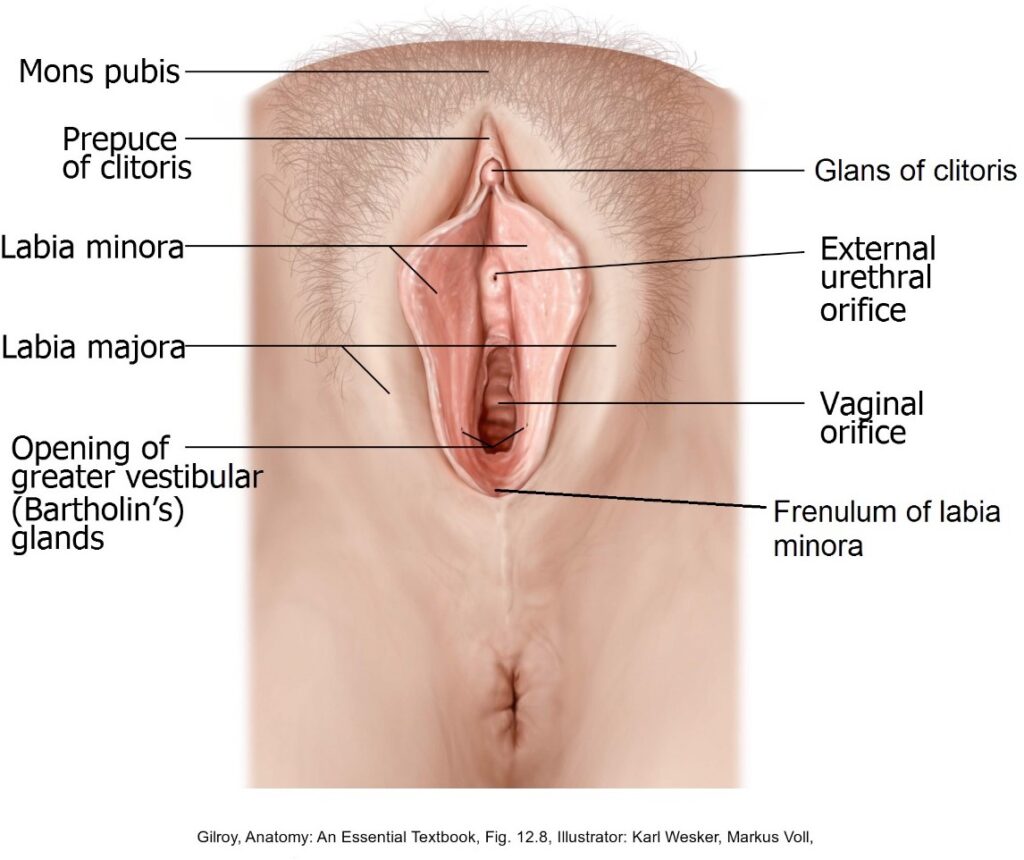
The parts of the female external genitalia are collectively called the vulva.
-
Mons pubis
The subcutaneous fat pad that covers the pubic bones and symphysis.
-
Labia majora
Filled with fat and connective tissue(and each contains the distal attachment of the round ligament of the uterus). Superiorly they fuse with the mons pubis. Their lateral surfaces have pubic hair; their medial surfaces are smooth.
- The pudendal cleft is the space between the labia majora.
-
Labia minora
Folds of skin with no fat. Their lateral surfaces contact the labia majora. In the anatomic position, their medial surfaces touch one another.
- The vestibule is the cavity between the labia minora.
- The labia minora are united below by the frenulum of the labia minora (clinicians call this the fourchette; French, fork).
- Superiorly the labia minora continue as thin folds that form a hood over the body of the clitoris = this is the prepuce of the clitoris.
-
Vestibule
The cleft between the labia minora into which these structures open:
- The external urethral orifice is inferior to the clitoris and superior to the vaginal orifice.
- The vaginal orifice (also called the introitus) is inferior to the urethral orifice. The periphery of the orifice may have remnants of a membrane called the hymen. The hymen is often ring-shaped and completely surrounds the vaginal orifice, or it may be crescent-shaped and surround only part of the orifice. In some cases the hymen may fully cover the vaginal orifice (imperforate hymen). It is composed of connective tissue and covered by a stratified squamous epithelium.
- The ducts of the greater vestibular glands (Bartholin’s glands) open into the vestibule on each side of the vagina.
- The ducts of the para-urethral glands (Skene’s glands) open into the vestibule on each side of the urethra. Some also open into the urethra itself. These lubricating glands are the homologues of the male prostatic glands and are located adjacent to the urethra along the anterior wall of the vagina. This area may correspond to the presumed erogenous zone known as the “G-spot,” described by Dr. Gräfenberg in 1950—well characterized in the media, but controversial in medical literature.
-
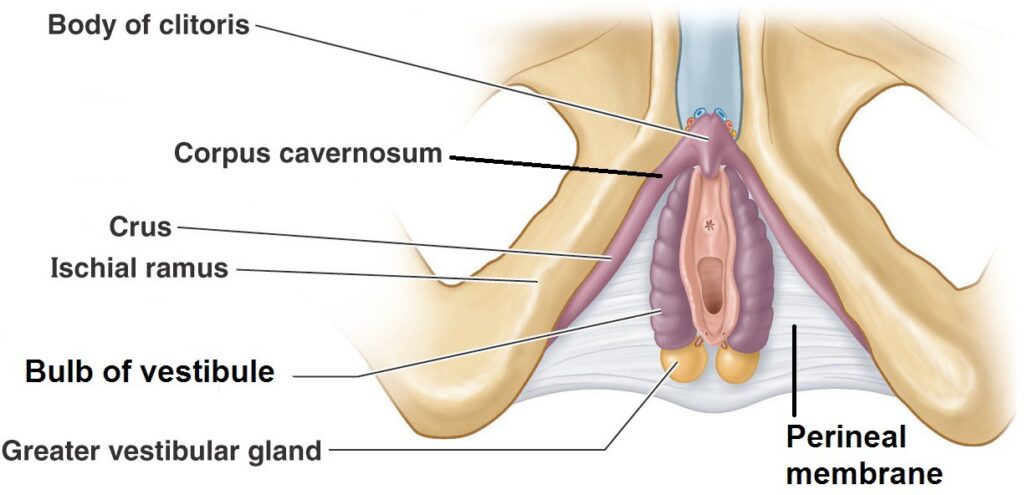
Clitoris
An erogenous organ mostly covered by the prepuce. It contains erectile bodies that enlarge during sexual arousal due to engorgement with blood. These are:
-
Two corpora cavernosa, the tapered proximal ends of which are the crura. Each crus attaches to an ischiopubic ramus and is fused to an ischiocavernosus muscle.
-
The two corpora cavernosa unite distally in the midline to form the single body of the clitoris.
-
The glans of the clitoris is the knob-shaped portion of the body at its distal free end, usually visible in the vulva.
innervation
The dorsal nerves of the clitoris (from the pudendal nerves) innervate this highly sensitive organ.

Blood supply
Blood supply is via the deep and dorsal arteries of the clitoris, terminal branches of the internal pudendal arteries. Venous drainage is via dorsal veins of the clitoris.
-
Bulbs of the vestibule
The bulbs are elongated masses of erectile tissue located on either side of the vestibule, deep to the labia minora. They are covered by the bulbospongiosus muscles.
-
Greater vestibular glands (Bartholin's glands)
- Oval masses about the size of a pea located posterior and deep to the vestibular bulbs. Their ducts open into the vestibule. Engorgement of the vestibular bulbs during sexual excitation compresses the glands, causing them to secrete fluid that lubricates the vestibule and vaginal orifice.
- If the vaginal orifice is viewed as a clock face, the greater vestibular glands are at 4 and 8 o’clock.
Clinical correlation
Blockage of ducts of the greater vestibular glands causes swelling and pain = a Bartholin’s gland cyst. These are common in women of childbearing age. They are treated by lancing or by placing a thin catheter in them to drain the cyst and prevent re-occurrence.
Female superficial perineal pouch
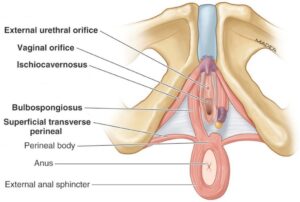
In addition to the clitoris, bulbs of the vestibule, and greater vestibular (Bartholin’s) glands, which have already been discussed, the superficial pouch in females contains skeletal muscles (paired = left and right):
-
- Ischiocavernosus muscles: Insert into the crura of the clitoris. These muscles are thought to support the erect clitoris and maintain erection by compressing veins to restrict outflow of blood.
- Bulbospongiosus muscles: Cover the bulbs of the vestibule. They function to constrict the orifice of the vagina (closing the vagina to protect it), support the clitoris, and compress Bartholin’s glands to empty them.
- Superficial transverse perineal muscles: Insert into the perineal body (described later) in the midline of the perineum and act to produce tension to support the perineum and pelvic viscera.
innervation
All of the above muscles are innervated by the pudendal nerve. The same goes for the male.
Female deep perineal pouch
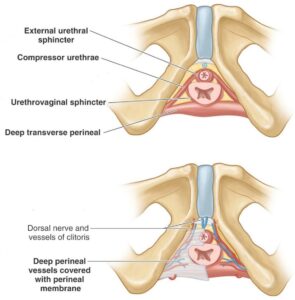
(See Figure 10.) This poorly defined compartment above the perineal membrane contains the urethra and vagina and two muscles, also innervated by the pudendal nerve:
-
- Deep transverse perineal muscles: Contains a mix of skeletal and smooth muscle. Functions similar to the superficial transverse perineal muscles in supporting the perineum and pelvic viscera.
- External urethral sphincter: Surrounds the urethra above the perineal membrane and compresses it to maintain urinary continence. Contraction can also interrupt the stream of urine during micturition. Children learn to control this voluntary sphincter through “toilet training”. Some of its muscle fibers encircle the vagina and function to constrict the vaginal lumen.
- The dorsal nerves and arteries of the clitoris, terminal branches of the pudendal nerves and internal pudendal arteries, course through the deep pouch on their way to the dorsal surface of the clitoris.
UG triangle in males
Male external genitalia
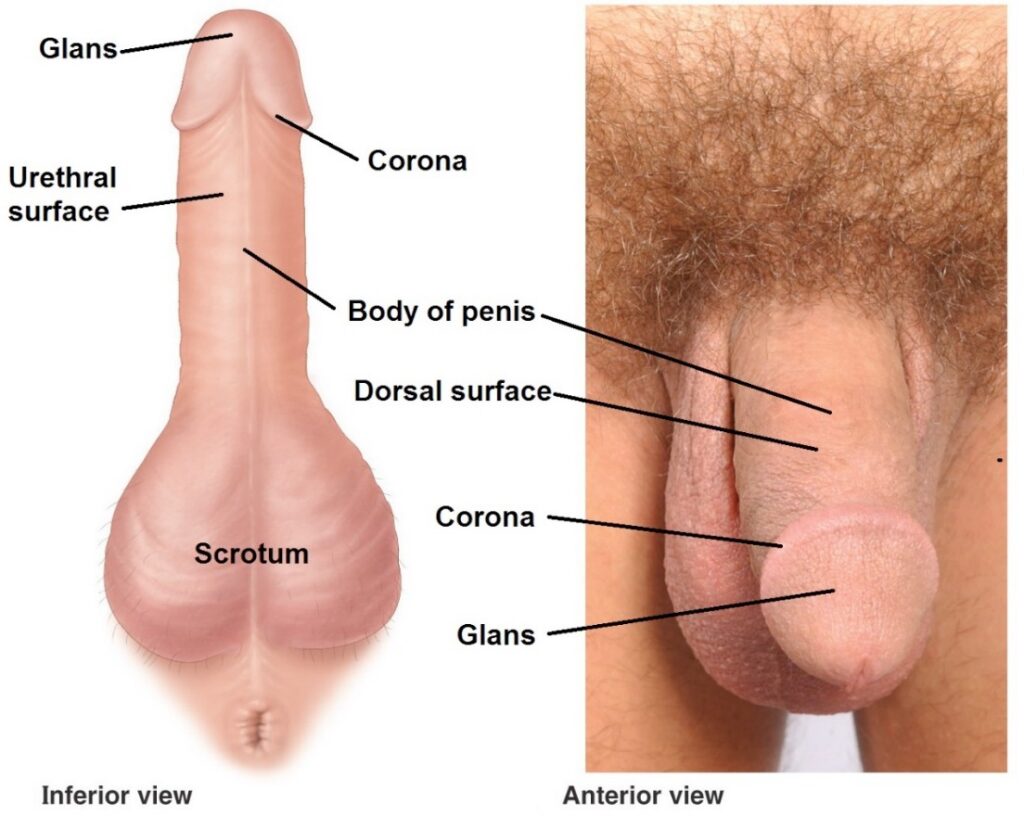
Penis
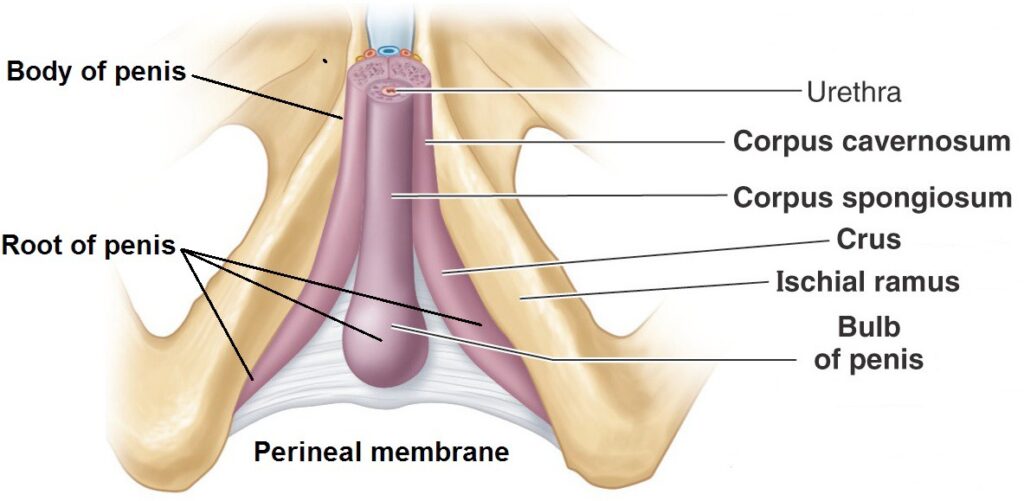
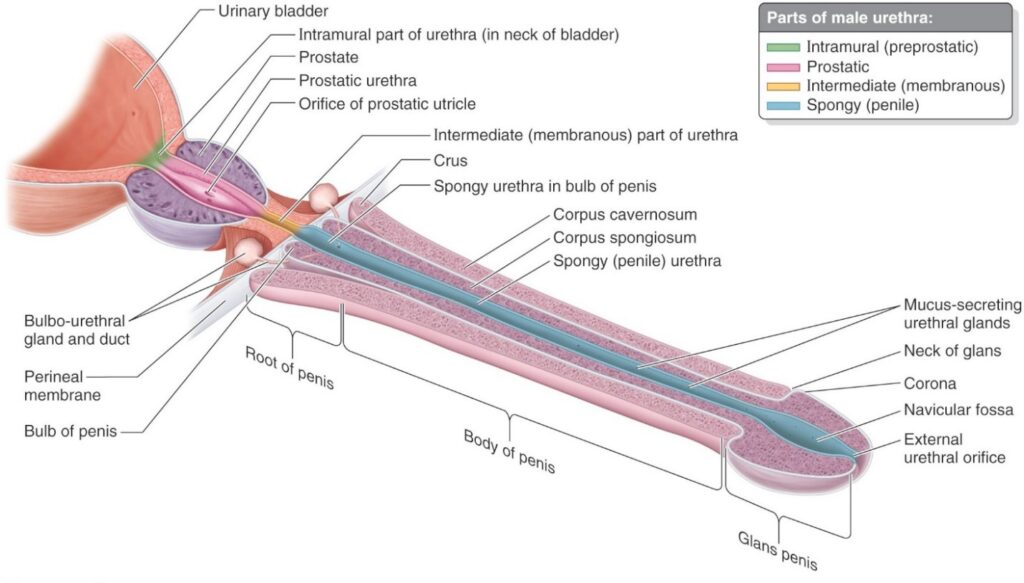
The penis is the male organ of copulation. Since it contains the urethra (unlike the clitoris), it also serves as a spigot for urine and semen. The penis has 3 parts:
- The penis has dorsal and urethral surfaces. Oddly, the anatomically correct position is achieved only when the penis is fully erect.
- In the uncircumcised penis, a double-layer of skin passes from the shaft over the glans, and back again to the shaft, forming a hood of penile skin. This is the prepuce or foreskin. It can be retracted to display the entire glans.
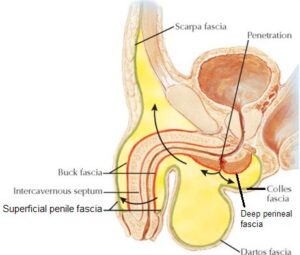
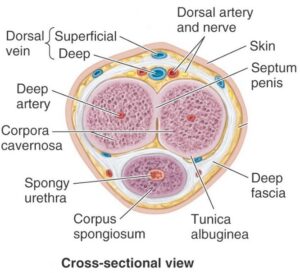
- Penile fascia:
- Just deep to the thin penile skin is the superficial penile fascia. This is continuous with the superficial perineal fascia (Colle’s fascia) and the dartos in the scrotum.
- Below the superficial penile fascia is the deep penile fascia (Buck’s fascia). It is continuous with the deep perineal fascia, but does not dip down into the scrotum. This strong fascia binds together the three erectile bodies of the penis.It ends at the neck and does not cover the glans.
- Below the deep fascia is the tunica albuginea—a fibrous capsule that encases the erectile bodies of the penis. It has a median septum between the two corpora cavernosa.
The penis is supported from the body wall by two ligaments:
-
- The suspensory ligament is a band of deep fascia that connects the dorsal surface of the penis to the pubic symphysis and is continuous with the deep penile (Buck’s) fascia. It is short and taut and supports the erect penis.
- The fundiform ligament is a sling around the proximal shaft of the penis, continuous above with the membranous layer of superficial fascia (Scarpa’s). It is long and loose and supports the flaccid penis.
innervation
Sensory innervation is via the dorsal nerves of the penis, from the pudendal nerves.

Blood supply
The blood supply is via deep and dorsal arteries of the penis. These are the terminal branches of the internal pudendal arteries. Dorsal veins of the penis drain the blood.
- Erection of the penis and clitoris
The erectile bodies of the penis and clitoris contain a meshwork of fibrous trabeculae derived from the tunica albuginea. Between the trabeculae are spaces resembling tiny collapsed veins. These cavernous spaces fill with blood during sexual arousal. The erectile bodies receive their blood supply from tiny corkscrew- shaped helicine arteries, branches of the deep and dorsal arteries of the penis/ clitoris. In their coiled configuration, there is little blood flow through the arteries.
Parasympathetic stimulation relaxes smooth muscle in helicine arteries. As they fill with blood they “straighten out” and blood flows into the cavernous spaces and distends the erectile bodies. Swelling of the penis and clitoris (technical term = tumescence) compresses the veins draining the erectile bodies, mainly the deep dorsal vein of the penis/clitoris. This helps maintain the erection.
Scrotum
The scrotum has thin, darkly pigmented skin, hairs, and no fat.
-
- The dartos is the superficial fascia of the scrotum—continuous with the superficial perineal fascia and superficial penile fascia. It contains smooth muscle fibers that insert into the skin. Cool temperatures cause the dartos muscle to contract—producing wrinkling of the scrotal skin that conserves heat. The dartos muscle relaxes when the scrotum is warm—which smooths out the scrotal skin to dissipate heat.
- An external midline scrotal raphé in the skin indicates fusion of embryonic primordia. An internal septum divides the scrotum into two compartments.
- The scrotum contains the testes and epididymis and their coverings = the three layers of spermatic fasciae (external, cremasteric, and internal).
- The lymphatic drainage of the scrotum follows that of the rest of the perineum. The testes within the scrotum however have a different lymphatic drainage. Do you remember this?
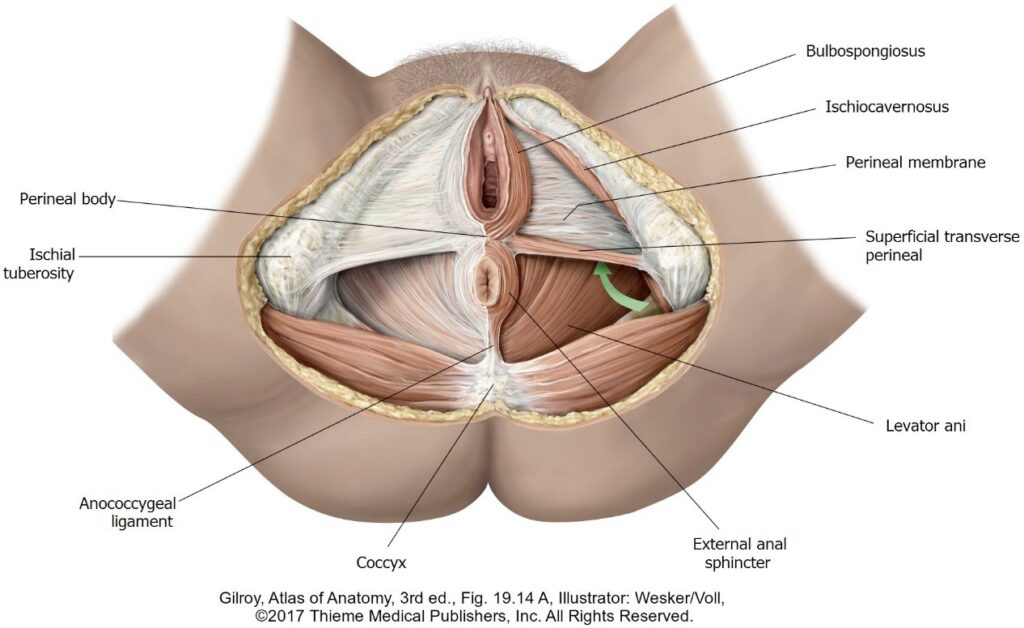
Male superficial perineal pouch
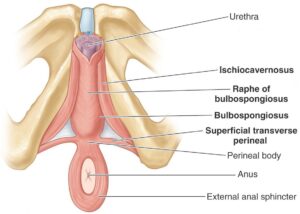
Contains the root of the penis (discussed earlier), proximal part of the spongy urethra (called the bulbar part by clinicians),and skeletal muscles. The pendulous part of the penis hangs down away from the perineum, so only its “root” is technically contained in the superficial pouch. The muscles in the superficial pouch have the same names as those in the female, but are generally more robust. See Figure 14.
-
- Ischiocavernosus muscles: Originate from the ischiopubic rami and insert on the crura of the penis. They support the erect penis and maintain the erection by compressing veins to restrict the outflow of blood.
- Bulbospongiosus muscles: The left and right muscles unite in the midline (in a tendinous raphé) over the bulb of the penis. They function in the male to support the penis and compress the bulb—this squeezing action ejects the last few drops of urine or semen from the urethra.
- Superficial transverse perineal muscles: Originate from the ischial tuberosities and insert into the perineal body in the midline of the perineum. They support the perineum and pelvic viscera.
Male deep perineal pouch
- Deep transverse perineal muscles: Support the perineum and pelvic viscera.
- External urethral sphincter: Surrounds the urethra above the perineal membrane. It compresses the urethra to maintain urinary continence. Contraction can also interrupt the stream of urine during micturition.
- The part of the male urethra passing through the deep pouch is the intermediate (membranous) part. The equivalent part in females has no name.
- The dorsal nerves and arteries of the penis course through the deep pouch.
- Males have glands located in the deep pouch. These are the bulbo-urethral glands (Cowper’s glands). They are the counterparts of the female greater vestibular (Bartholin’s) glands (in the superficial pouch in females). These function to lubricate the male urethra during sexual arousal—producing the “pre-ejaculate”. Their ducts penetrate the perineal membrane to empty into the spongy urethra in the bulb of the penis.
Male urethra
The male urethra has 3 or 4 parts (depending on the source). We will name three:
Perineal body
- A mass of fibromuscular tissue situated in the center of the perineum at the intersection of UG and anal triangles in both sexes. Located between the vagina and anal canal in the female, and the scrotum and anal canal in males. See Figure 18 for the location of the perineal body.
- The perineal body is larger and more clinically important in the female. Being a point of attachment of most muscles in the perineum, as well as the levator ani, it is a stabilizing point of the perineum involved in maintaining perineal integrity—helping to support the anal canal and vagina.
Clinical correlation
Episiotomy is a clinical procedure where the posterior or posterolateral wall of the vaginal canal and adjacent perineum is incised during delivery of a baby, presumably to avoid overstretching and uncontrolled tearing of the perineum.
Episiotomies are warranted in some cases, but debate about the usefulness of routine episiotomy has led to their decline. If episiotomy is done in the midline, the incision could disrupt the perineal body.
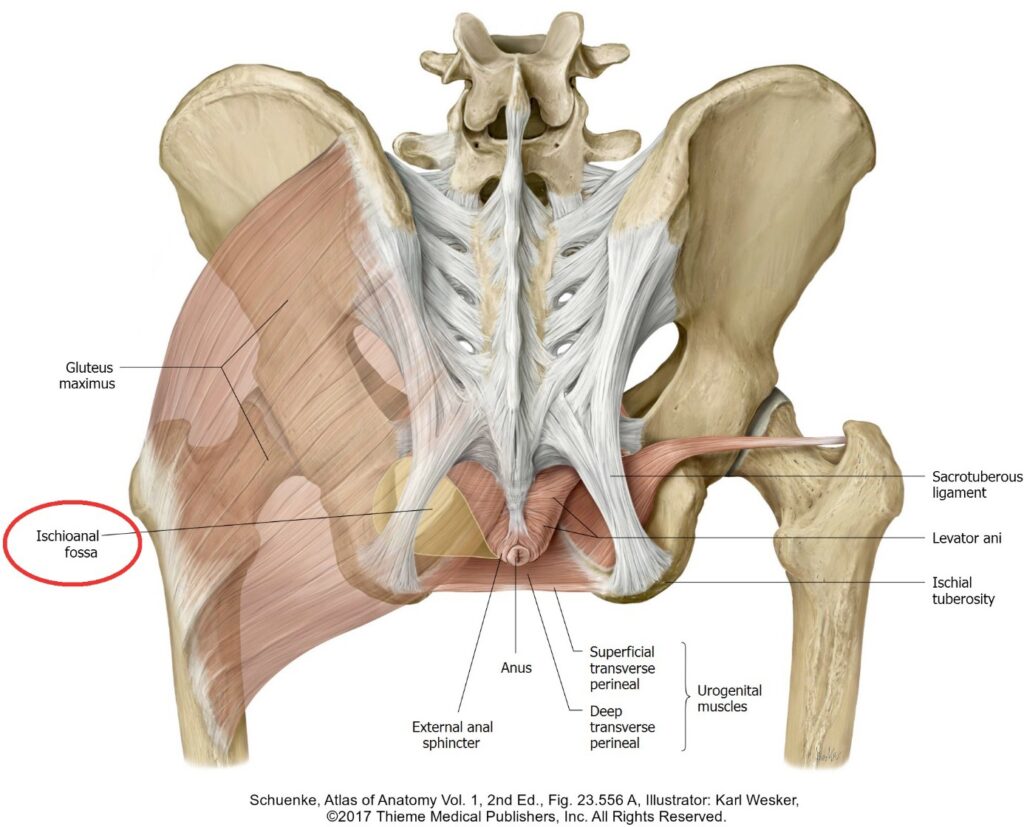
Anal triangle
Contains the anal canal, external anal sphincter, and the left and right ischio-anal fossae. The anal canal opens at the center of the anal triangle at the anus. The anus is within the intergluteal cleft, also called the natal cleft. The roof of the anal triangle is the pelvic diaphragm. The external surface of the anal triangle is covered by skin. There are no pouches in the anal triangle (thank goodness!).
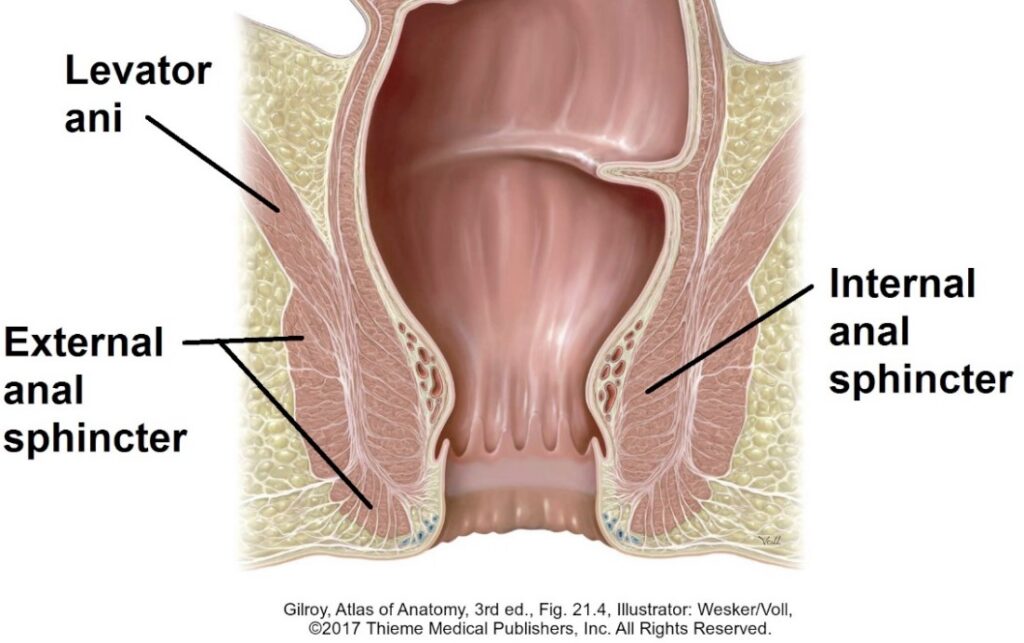
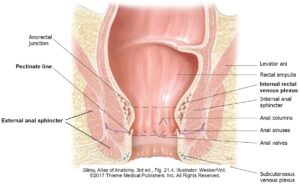
Anal canal
The terminal portion of the GI tube—about 3 cm in length—begins at the pelvic diaphragm at the anorectal junction and terminates at the anus.
Relationships
- Surrounded by the internal and external anal sphincters. The perineal body is anterior and the anococcygeal ligament is posterior. Laterally are the ischio-anal fossae.
Internal features
- The upper half is marked by vertical folds of mucosa called anal columns. The superior margin of the anal columns mark the anorectal junction. The columns contain the terminal branches of the superior rectal artery and a venous tributary of the superior rectal vein. The veins are joined together in a submucosal internal rectal venous plexus.
- The depressions between anal columns are anal sinuses. Glands in the sinuses are compressed by passing feces, causing them to secrete mucus that lubricates the feces to aid in the evacuation of the anal canal.
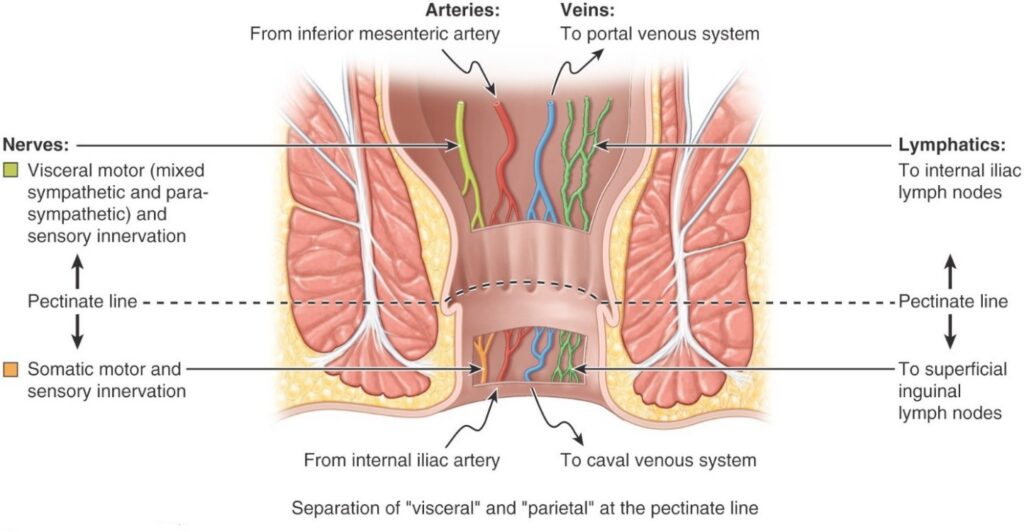
- Each of the anal columns is connected to their neighbors at their base by a fold of mucous membrane called the anal valve. When considered as a whole, all of the anal valves make up a sinuous ridge encircling the anal canal—this is the pectinate line.
- The pectinate line indicates the junction of the superior part of the anal canal (derived from the embryonic hindgut) and the inferior part (derived from the embryonic proctodeum). This is the approximate location of the embryonic anal membrane. Recall that the histology of the anal canal above the pectinate line is mucous membrane, while below it is skin.
- The parts of the anal canal superior and inferior to the pectinate line differ in their embryonic origin, epithelial lining, innervation, vascular supply, and lymphatic drainage. See Figure 17.
Clinical correlation: Hemorrhoids
(Old-timers call these “piles.”)
Above the pectinate line the internal rectal venous plexus drains to the superior rectal vein (portal system). Rising intra-abdominal pressures, as during straining when attempting to evacuate the anal canal (constipation), or portal hypertension, can produce varicose veins in the plexus in the region of the anal columns. These are internal hemorrhoids. They can be quite large, so much so that they protrude out of the anus, and may be painless.
Below the pectinate line a smaller subcutaneous plexus of veins is located near the anus. This drains into inferior anal veins (to IVC = systemic veins). Irritation of the skin in this area (due to diarrhea for example) can cause swelling of the veins, producing external hemorrhoids. They are much more painful than internal hemorrhoids. Why would this be so?
Anal sphincters
- Internal anal sphincter: The circular layer of smooth muscle in the rectum continues into the anal canal and thickens to form the internal anal sphincter. It surrounds the upper half of the anal canal from the pelvic diaphragm to the level of the pectinate line. It is tonically contracted most of the time. The presence of feces in the lower rectum causes reflex relaxation of the internal sphincter due to parasympathetic innervation (autonomic) to allow for emptying of the rectum. If emptying is not wanted, the external anal sphincter can be used to prevent it.
- External anal sphincter: Constructed of skeletal muscle under voluntary control (inferior anal branch of pudendal nerve). It attaches to the perineal body and coccyx and surrounds the entire anal canal. The external anal sphincter has tone during waking hours to aid in fecal continence, and it increases when intra-abdominal pressure increases. Tone can be assessed with digital examination. It relaxes while sleeping. When the sphincter is consciously relaxed, peristalsis in the rectum moves feces through the anal canal during the act of defecation.
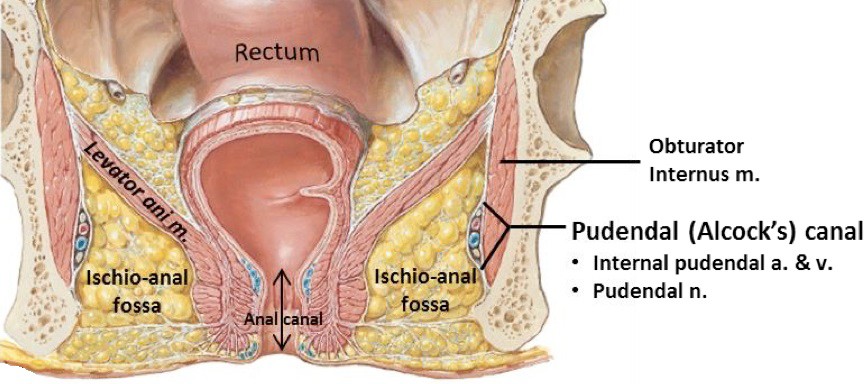
Ischio-anal fossae (formerly called ischio-rectal fossae)
Wedge-shaped spaces on either side of the anal canal. The perineal body and anal canal separate the two fossae, but they do communicate posterior to the anal canal. See Figures 20 and 21. Click on the figures to enlarge them.
Boundaries
- Inferior: Skin.
- Superior and medial: The sloping inferior surface of the levator ani.
- Lateral: Fascia covering the obturator internus muscle. Because of the attachment of the levator ani half way up the lateral pelvic wall, half of the obturator internus borders the pelvic cavity above and the other half borders the ischio-anal fossa below.
- Posterior: Sacrotuberous ligament and gluteus maximus muscle.
- Anterior: Each fossa extends forward into the deep perineal pouch in the UG triangle. This triangular space is the anterior recess of the ischio-anal fossa. It is limited by the pubic bones anteriorly. The anterior recesses are the superior, fat-filled parts of the deep perineal pouch.
contents
- Mainly a large adipose body. This is semi-liquid at body temperature, allowing the anal canal to expand when feces are passed.
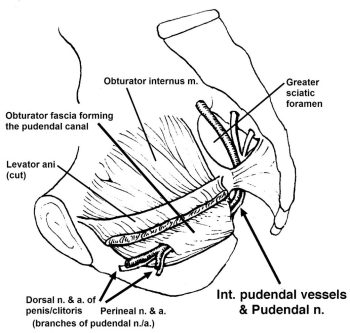
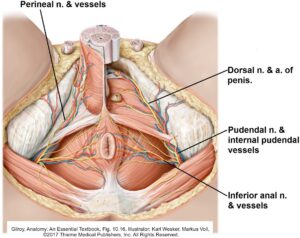
- Pudendal canal (Alcock’s canal): Formed by a layer of obturator fascia that rolls-up in a tube in the lateral wall of the ischio-anal fossa. This provides a tunnel through the adipose body for the passage of the internal pudendal artery and vein and the pudendal nerve.
- The inferior anal (rectal) nerve splits from the pudendal nerve at the entrance (posterior end) of the pudendal canal. It crosses the ischio-anal fossa from lateral to medial, innervating the external anal sphincter, the lower half of the anal canal, and the peri-anal skin.
Clinical correlation
Blocked mucous glands in the anal sinuses of the anal canal can become infected. Spread of infection into the wall of the anal canal produces a peri-anal abscess. Severe cases can perforate the anal canal and sphincters and enter the adjacent ishio-anal fossa. Fat is a feast for bacteria! Most peri-anal abscesses require surgical incision and drainage.
Summary tables
Table 1. Summary table: Innervation of perineum
|
Nerve |
Function |
|---|---|
|
Pudendal nerve (S-2, S-3, and S-4)—major branches listed below: |
|
|
Motor to external anal sphincter Sensory to lower half of anal canal and peri-anal skin |
|
Motor to all muscles in superficial and deep pouches Sensory to posterior scrotum/labia |
|
Sensory to penis/clitoris |
|
Ilioinguinal nerve (L-1) and Genitofemoral nerve (L-1and L-2) |
Sensory to anterior scrotum/labia, mons pubis |
The pudendal nerve has a circuitous route from pelvis to perineum.
Here’s a flow chart:
Ventral rami of S2–S4 fuse to produce the pudendal nerve in the pelvic cavity
[Greater sciatic foramen]
Around the spine of ischium
[Lesser sciatic foramen]
Enters ischio-anal fossa
Gives off inferior anal nerve
[Enters pudendal canal]
Divides into terminal branches (perineal nerve and dorsal nerve of penis/clitoris)
Terminal branches enter UG triangle
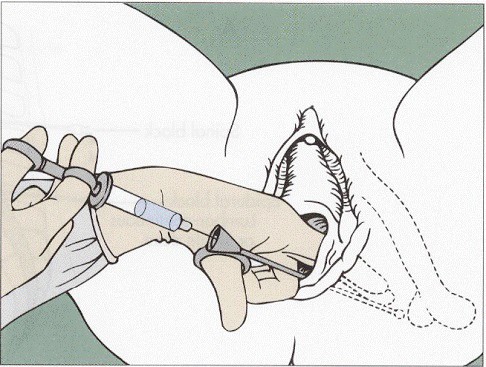
Clinical correlation: Pudendal nerve block
To ease the pain of vaginal delivery or perineal surgery, the pudendal nerve can be blocked with an anesthetic administered through the perineal skin (transcutaneous) or through the vaginal wall (transvaginal). The landmark for the needle tip is adjacent to the ischial spine, since the pudendal nerve loops around the spine as it passes from the greater sciatic foramen into the lesser sciatic foramen. However, this won’t block sensation to the anterior parts of the perineum. Why? (Hint: see Table 1.)
Clinical correlation: Pudendal neuralgia (Cyclist’s Syndrome)
Compression of the pudendal nerve due to prolonged sitting (as in a bicycle seat) can injure the nerve, occurring in the vicinity of the ischial spine or in the pudendal canal. This can cause severe pain in the perineal skin. Pudendal neuralgia can occur in other ways too—giving birth or falling hard on the buttocks.
Table 2. Summary table: Blood supply of perineum
|
Artery |
Regions/Structures supplied |
|---|---|
|
Internal pudendal artery (branch of internal iliac artery): Major branches listed below |
|
|
Inferior anal artery |
Lower anal canal, anal sphincters, peri-anal region |
|
Perineal artery |
Superficial pouch, posterior scrotum/labia |
|
Deep artery ofpenis/clitoris |
Corpora cavernosa of penis/clitoris |
|
Dorsal artery of penis/clitoris |
Deep pouch, skin of penis/clitoris, glans of penis/ clitoris, spongy urethra |
|
External pudendal artery (branch of femoral artery) |
Mons pubis, anterior scrotum/labia |
Table 3. Summary table: Venous drainage of perineum
|
Vein |
Regions of venous drainage |
|---|---|
|
Internal pudendal vein (tributary of internal iliac vein)
|
Muscles of superficial and deep pouches, lower half of anal canal, anal sphincters, peri-anal region |
|
External pudendal vein (tributary of great saphenous vein) |
Skin of penis/clitoris, scrotum/labia |
|
Deep dorsal vein of penis/clitoris
|
Erectile tissues of penis/clitoris |
|
Superior rectal vein (tributary of inferior mesenteric v.) |
Upper half of anal canal |
Table 4. Summary table: Lymphatic drainage of perineum
|
Nodes |
Regions of drainage |
|---|---|
|
Inferior mesenteric nodes (near aorta) |
Upper half of anal canal (lymphatics follow superior rectal artery) |
|
Internal iliac nodes |
Deep perineal pouch |
|
Superficial inguinal nodes |
Most of perineum: penis, clitoris, scrotum, labia, superficial pouch, lower anal canal, anal sphincters, vestibule, lower vagina |
Clinical correlation
Tumors, lesions, and infections in the perineum can cause enlarged superficial inguinal nodes in the groin. Additionally, lymph from the gluteal region and the superficial tissues of the entire lower trunk inferior to the umbilicus (abdominal wall and back) also drains to the superficial inguinal nodes. Holy smoke . . . these nodes receive lymph from a large region of the body!
Remember
Lymphatic drainage of the testes DOES NOT follow the drainage of the scrotum.
Table 5. Summary table: Homologous structures in the perineum
Thought question
What does homologous mean?
|
Female |
Male |
|---|---|
|
Body of clitoris |
Corpora cavernosa of penis |
|
Labia majora |
Scrotum |
|
Labia minora |
Urethral surface of penis |
|
Vestibule |
Spongy (penile) urethra |
|
Bulbs of the vestibule |
Bulb of penis and corpus spongiosum |
|
Greater vestibular (Bartholin’s) glands |
Bulbo-urethral (Cowper’s) glands |
|
Para-urethral (Skene’s) glands |
Prostatic glands |