- Optional Reading
- The Developing Human: Clinically Oriented Embryology, 12th ed., chapter 12, Development of genital system section through Anomalies of uterine tubes, uterus, and vagina.
The adult organs that will be discussed in this chapter are the gonads and the accessory sex organs.
- Male
- Female
In the male, the gonad is the testis in the scrotum, and the accessory organs include sperm-carrying ducts plus glands. The testis contains the tunica albuginea and the seminiferous tubules (with intervening connective tissue and interstitial cells), and the rete testis. The accessory tubes include the efferent ductules, ductus epididymis, ductus deferens, and ejaculatory ducts. The glands are the seminal vesicles, prostate, and bulbo-urethral glands.
In the female, the gonad is the ovary in the pelvis. In the ovary are follicles consisting of the oocyte and the follicular cells (with connective tissue and theca cells between the follicles). The accessory organs include the uterine tube, uterus, and vagina.
Even though the chromosomal sex of the embryo is determined at the time of fertilization, the gonads do not develop male or female anatomic characteristics until Week 7. Therefore, the development of the gonad prior to Week 7 is referred to as the indifferent stage.
Development of the gonads
Stage of the indifferent gonad
In both sexes, the gonads begin development within the intermediate mesoderm in the 5th week. A portion of the intermediate mesoderm evaginates into the coelom to form the genital ridge (or gonadal ridge). It is located adjacent to the mesonephric kidney in the lumbar region. The mesonephric tubules and duct lie lateral to the genital ridge. The mesonephricduct is also referred to as the Wolffian duct.
Three sources will contribute to the gonad:
1
Epithelium of the genital ridge (a.k.a. coelomic epithelium or mesothelium)
2
Mesenchyme within the ridge
3
Primordial germ cells: Give rise to the sex cells: the oogonia and spermatogonia
Shortly before primordial germ cells arrive, epithelium thickens and penetrates the mesenchyme to form irregularly shaped primitive (primary) sex cords, connected to the surface epithelium.
The primordial germ cells first appear during Week 3 within the endoderm of the yolk sac near the connecting stalk.
After folding of the embryonic disc
They reside in the walls of the hindgut.
The germ cells migrate through the dorsal mesentery of the hindgut to the genital ridges.
They enter the primitive cords.
Shortly after this, the male and female conditions diverge.
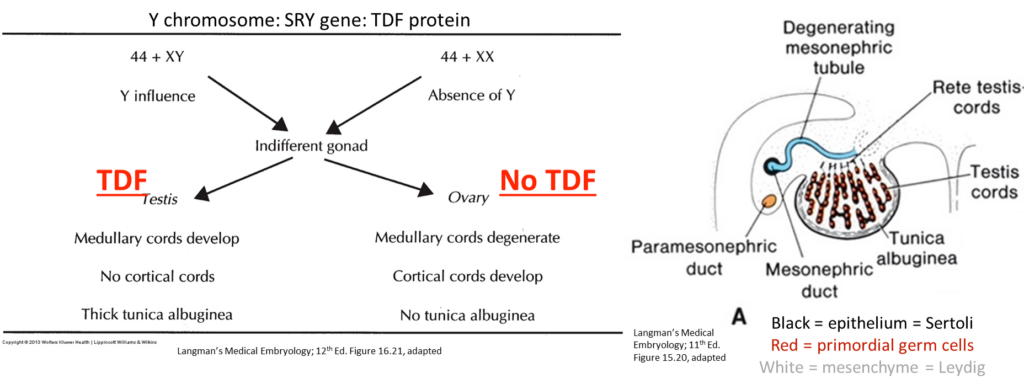
Testis
- Seventh week: A testis-determining factor (protein) is expressed in cells of the indifferent gonad, encoded by the SRY gene (sex-determining region of the Y chromosome gene). Under the influence of this protein, specific cells of the indifferent gonad begin to differentiate into Sertoli cells (supporting cells in the testis). Genetic females lack the SRY gene and therefore do not produce testis-determining factor.
-
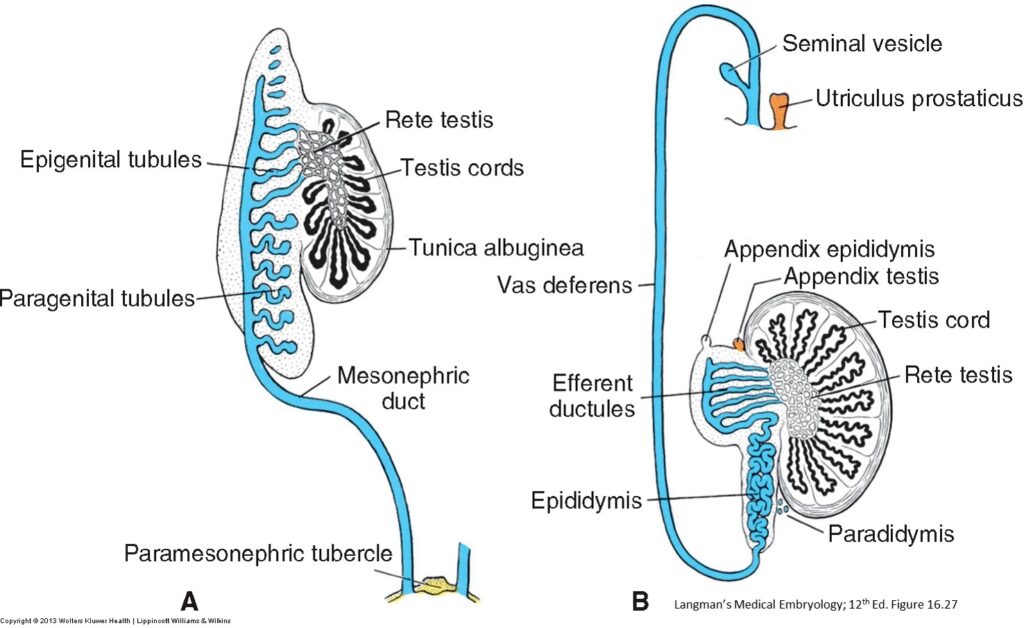
- Primary sex cords persist, proliferate, and penetrate deep into the genital ridges to form the testis cords.
- During further development: testis cords separate from the coelomic epithelium, as a fibrous tunica albuginea capsule appears between the two.
- No sex cells remain in the surface epithelium.
- Toward the center of the genital ridges, some of the testis cords break up into tiny strands that will become the rete testis.
- At this point the testis cords are in close proximity to the mesonephric kidney tubules and duct.
Testis cords
seminiferous tubules and the rete testis
Primordial germ cells within the cords
spermatogonia
Other cells in the cords, originally from the coelomic epithelium
Sustentacular (Sertoli) cells
Mesenchyme between the testis cords
loose connective tissue and interstitial (Leydig) cells
(which secrete testosterone in 8th week to influence sexual differentiation of genital ducts and external genitalia).
These testis cords remain solid until puberty, then hollow out and become the actual seminiferous tubules under the influence of testosterone.
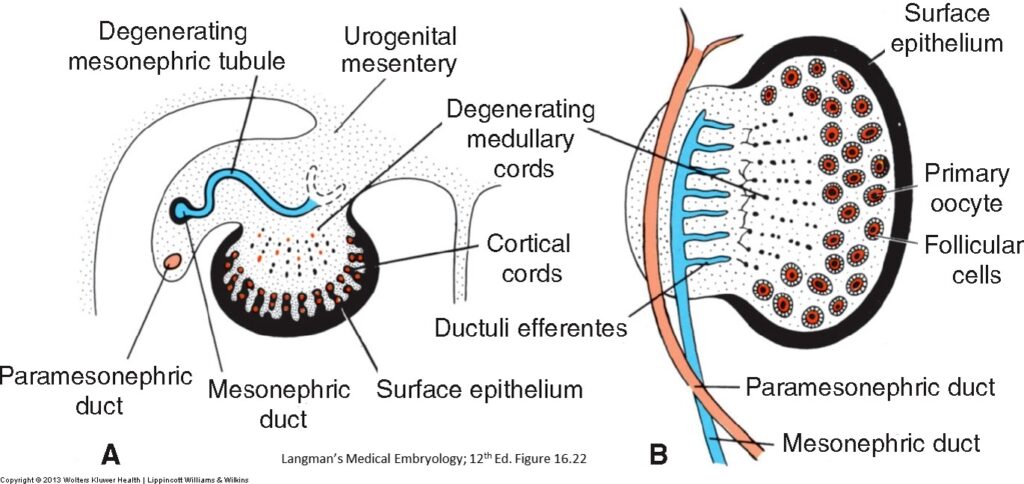
Ovary
- In the absence of the Y chromosome and SRY gene, female development occurs.
- Primary sex cords do not persist because there is no testis determining factor: They break up and degenerate.
- The thick surface epithelium still contains germ cells and continues to proliferate into a second generation of cords: Secondary sex cords migrate a short way into the mesenchyme in the 7th week.
- In the 3rd month, the secondary sex cords split up into isolated spherical clusters of cells called follicles.
- Each follicle consists of a single oogonium (derived from a primordial germ cell), surrounded by a ring of smaller follicular cells derived from the surface epithelium that nourish the oocyte and help to produce the female sex hormones.
- Together the oogonia and follicular cells constitute a primordial follicle.
Mesenchyme within the embryonic ovary
the connective tissue between the follicles, as well as the connective tissue and theca cells of the ovarian medulla
(Theca cells surround the ovarian follicles and produce androgens that are converted into estrogens, the female sex hormones.)
Summary: Differences of male and female gonadal development
- Male: Primary sex cords persist and become seminiferous tubules.
- Female: Primary cords regress; surface epithelium produces new, secondary cords and become follicles.
- Testis cords and follicles form as independent ingrowths from the coelomic epithelium that contains the germ cells.
- Tunica albuginea develops in testis, forming a thick capsule around the organ.
- No tunica albuginea develops in ovary—this would hinder ovulation.
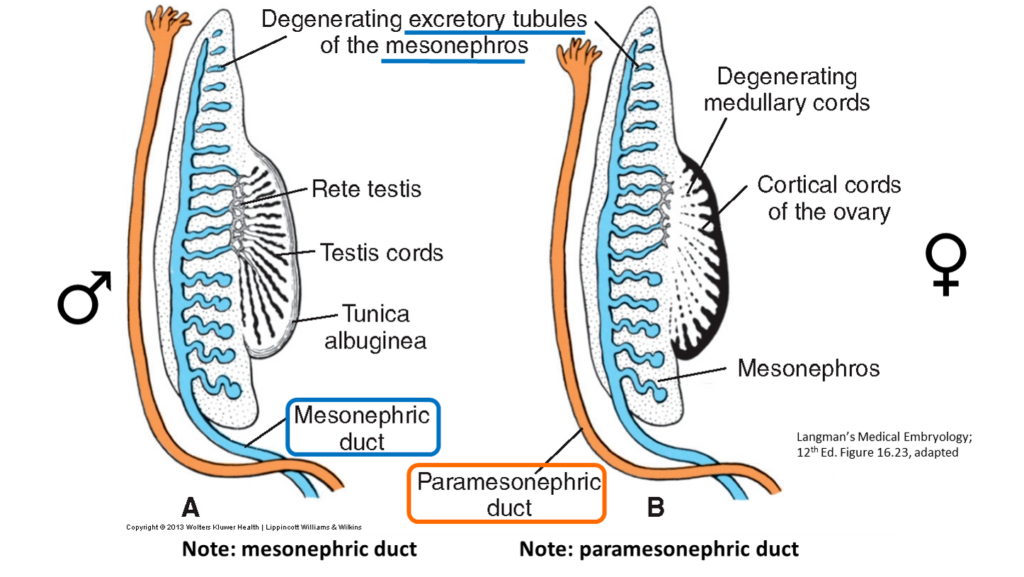
Development of accessory sex organs: Ducts and glands
Indifferent stage
In the sexually indifferent stage of both sexes, two longitudinally running ducts lie lateral to each gonad:
Overview
In each sex, only one of the two ducts persists to convey the sex cells. The other duct will degenerate completely, except for non-functioning vestiges.
- Male
- Female
-
Retains only the mesonephric system.
-
Mesonephric tubules nearest the testis connect to the testis cords; will become the efferent ductules.
-
Mesonephric duct part nearest efferent tubules elongates and convolutes to become the epididymis duct.
-
Most of the length of mesonephric duct becomes the ductus deferens.
-
Seminal vesicle: Forms from an outbudding of the mesonephric duct near its entry into the primitive urogenital sinus.
-
The most distal portion of the mesonephric duct becomes the ejaculatory duct.
-
-
The prostate and bulbo-urethral glands arise as outgrowths from the urethra.
-
The testis descends, and the male genitalia achieve their final relative positions (described in the Descent of the gonads chapter).
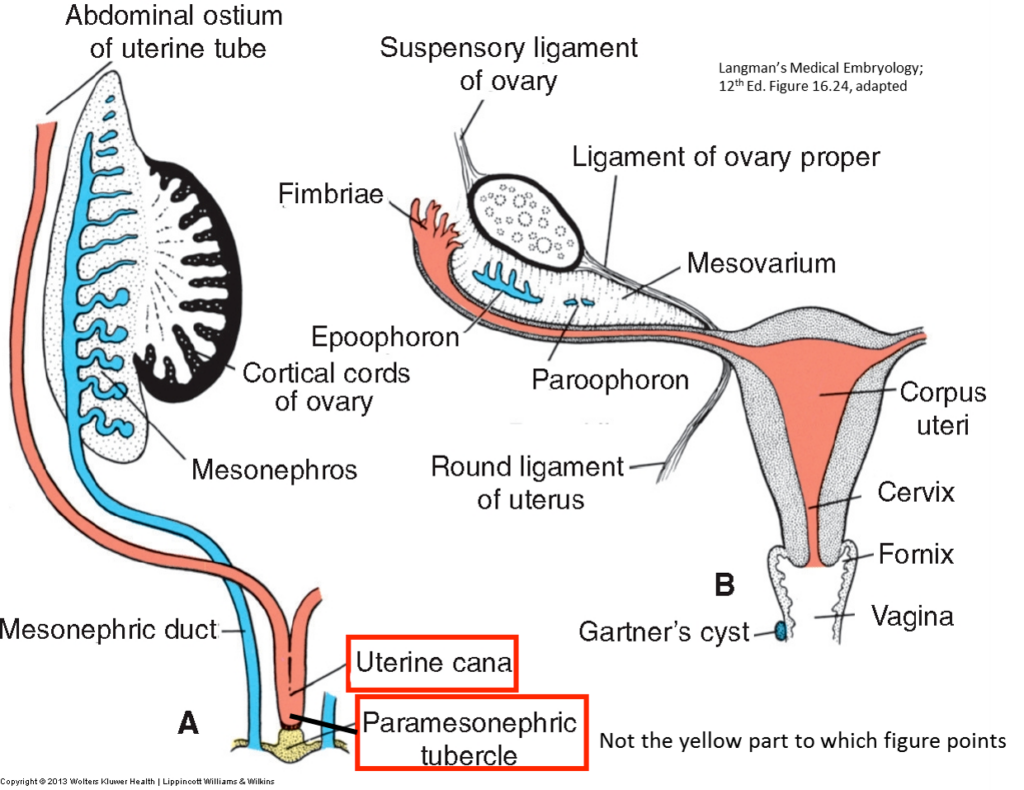
- Retains only the paramesonephric duct.
- Proximal end of paramesonephric duct has a funnel- shaped ostium that is open to the peritoneal cavity.
- Lies lateral to the mesonephric duct throughout most of its extent, however, its caudal part runs medially.
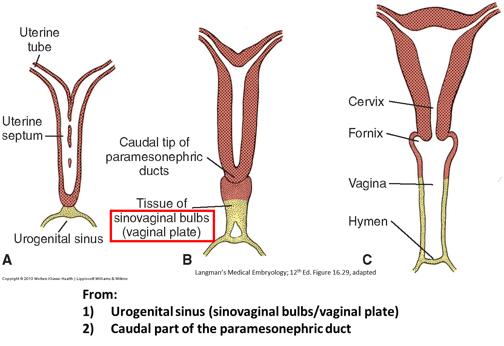
- Caudal parts of the right and left paramesonephric ducts fuse in the midline to form the uterovaginal primordium.
- Caudal tip of this fusion (paramesonephric tubercle) abuts the posterior wall of the urogenital sinus.
- Ovary descends into the pelvis into its final position because it is blocked by the caudal part of the paramesonephric duct and its mesentery, the broad ligament of the uterus.
- Proximal funnel of the paramesonephric duct becomes the infundibulum of the uterine tube.
-
- Central portion of the paramesonephric duct becomes the ampulla and isthmus of the uterine tube.
- Uterovaginal primordium (fused distal parts of paramesonephric ducts) expands to form the uterus and the superior one-third of the vagina.
- The mesonephric tubules and duct degenerate in the female.
- Ovulation is now into the peritoneal cavity, and the ovum is then picked up by the infundibulum of the uterine tube.
Vagina
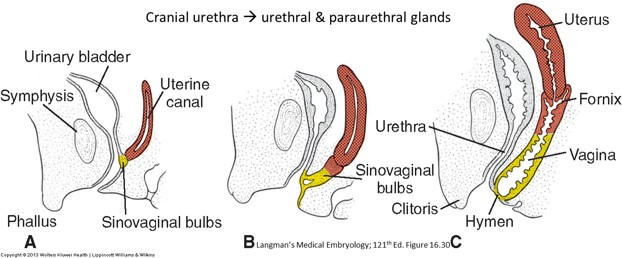
- Uterovaginal primordium abuts the dorsal surface of the distal part of the urogenital sinus. This part of the UG sinus will become the vestibule, which will contain the orifices of the urethra and vagina.
- Where they are in contact, there is a swelling in the urogenital sinus wall: the sinus tubercle.
- From this, a solid evagination of endoderm grows caudally out of the urogenital sinus: the sinovaginal bulb (a.k.a. vaginal plate).
- The sinovaginal bulb expands and hollows out to form the inferior two-thirds of the vagina.
- The superior third of the vagina, including the fornices, arise from the uterovaginal primordium.
- The vagina thus has a dual embryonic origin: upper 1/3 from paramesonephric ducts; lower 2/3 from urogenital sinus (which can be traced back developmentally to the hindgut!).
- The lumen of the vagina remains separated from the urogenital sinus by a membrane = the hymen. This usually persists postnatally and later becomes perforated.
- Males have a homologue of the vagina, the tiny dimple in the prostatic urethra called the prostatic utricle. This is likely a remnant of the sinus tubercle.
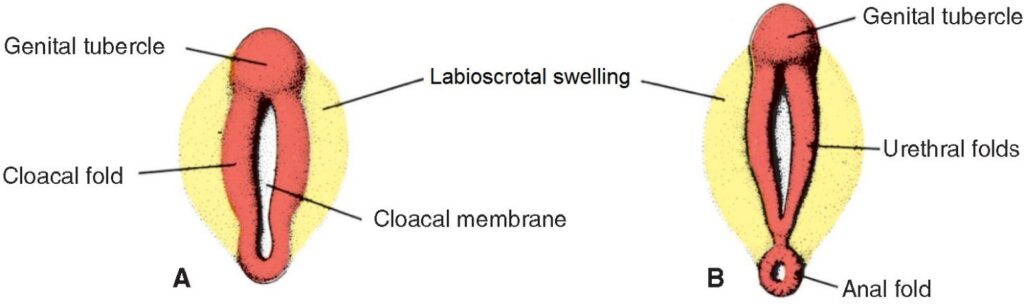
Development of the external genitalia
You will recall that the external genitalia are in the perineum, specifically in the urogenital triangle. Like the gonads and internal genitalia, the external genitalia in embryos begin their development similarly in both sexes, i.e., early on they have an indifferent stage.
Indifferent stage
-
The cloaca (the embryonic “sewer”) has an orifice located in the primitive perineum. Up until the 7th week this orifice is closed by a cloacal membrane. Recall that the cloaca becomes partitioned by a vertical wall of growing mesenchyme called the urorectal septum (Chapter 17). The anterior part of the cloaca becomes the urogenital sinus (future bladder, urethra, and vestibule [in females]), while the posterior cloaca becomes the anorectal canal (future rectum and anal canal). Upon reaching the surface ectoderm, the caudal tip of the urorectal septum gives rise to the perineal body—this divides the cloacal membrane into a urogenital membrane and anal membrane.
-
During the 3rd week, mesenchyme proliferates around the cloaca, producing external ridges called cloacal folds. The division of the cloaca partitions these into anterior urethral folds and posterior anal folds (these are not important to our current story). A mass of mesenchyme called the genital tubercle (phallus) forms where the left and right urethral folds meet anteriorly. This is the future penis or clitoris.
-
A second set of folds develops lateral to the urethral folds. These are called labioscrotal swellings.
-
By the end of the 6th week, it is not possible to differentiate males from females by their perineal anatomy. The external genitalia in males and females are usually fully differentiated by the 12th week.
- Male
- Female
- Testosterone produced by the testes masculinizes the external genitalia.
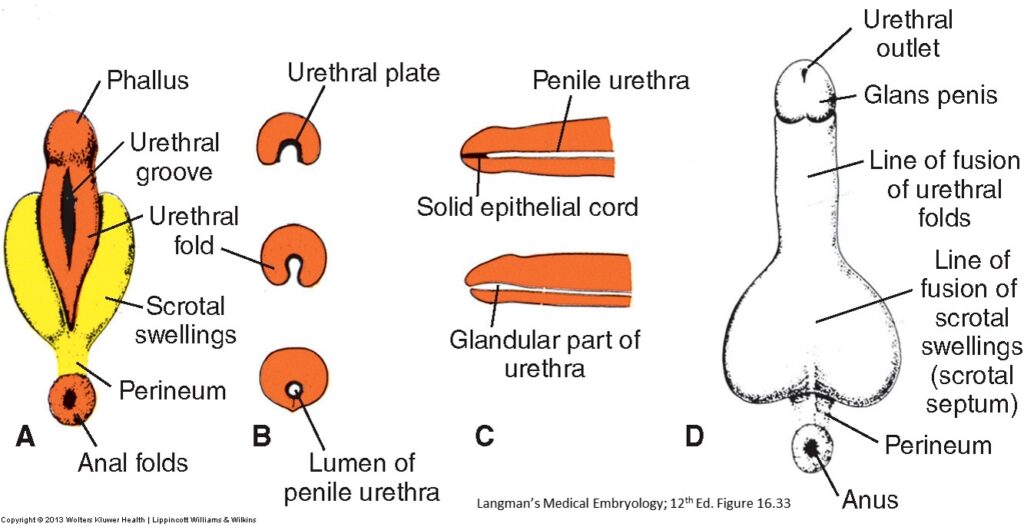
- The genital tubercle (phallus) elongates and the urogenital membrane ruptures. Together these cause the distal part of the urogenital sinus to expand onto the ventral surface of the genital tubercle, producing a urethral plate made of endoderm. The urethral folds expand around the urethral plate—they fuse in the midline along the ventral surface of the phallus, internalizing the urethral plate in the phallus. This becomes the spongy urethra and the fused urethral folds produce the urethral surface of the penis. A midline ridge in the skin on the urethral surface (penile raphé) indicates where the urethral folds fused.
- At the tip of the phallus (glans penis), ectoderm grows inward toward the urethral plate. This rod of ectoderm canalizes, as does the endoderm in the urethral plate, to form the lumen of the spongy urethra. Thus, the spongy urethra has a dual embryonic origin, and the epithelium in the distal part, just inside the external urethra orifice, is derived from ectoderm—this part is the navicular fossa.
- The labioscrotal swellings in males grow medially and fuse to form the scrotum. A prominent scrotal raphé is visible on the skin in the midline, indicating the line of fusion.
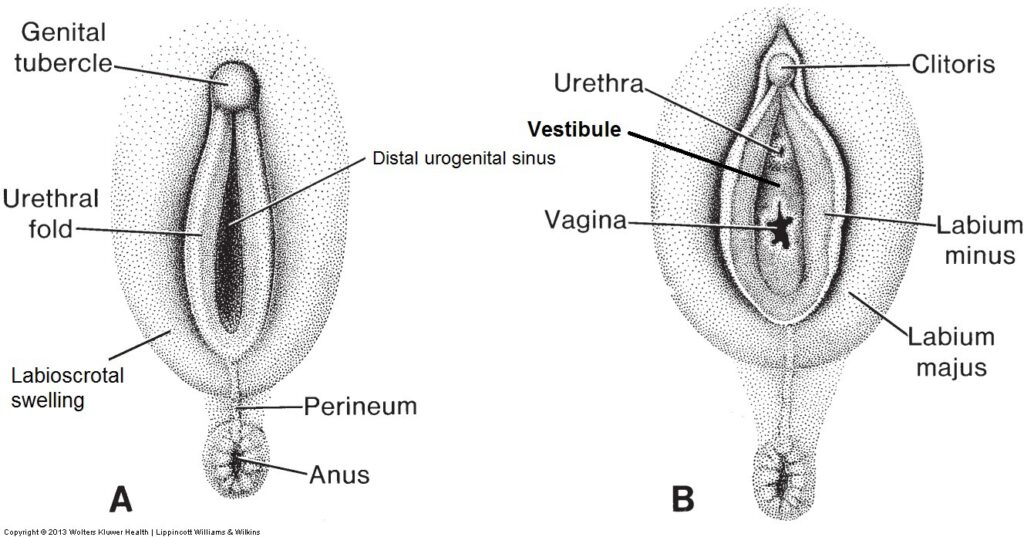
- Absence of testosterone in female embryos has three major effects:
- The phallus elongates less,
- The distal part of the urogenital sinus does not extend onto the phallus, and
- The urethral folds and labioscrotal swellings do not fuse.
- The genital tubercle (phallus) becomes the clitoris.
- The distal part of the urogenital sinus does not elongate on to the clitoris. Instead, it forms the vestibule. A urethral plate does not form—the clitoris therefore does not contain any part of the female urethra. The external urethral orifice opens within the vestibule, inferior to the clitoris.
- The urethral folds do not completely fuse. They form the labia minora. Anteriorly they fuse to form the prepuce of the clitoris. Posteriorly they fuse to form the frenulum of the labia minora (Fourchette).
- The labioscrotal swellings to not fuse—they form the labia majora.
Clinical correlation
Failure of the urethral folds to fuse properly can produce an abnormal opening of the spongy urethra on the urethral surface of the penis, rather than at the tip of the glans. Called hypospadias, it is the most common congenital defect of the penis. Most presentations of hypospadias occur near the glans penis.
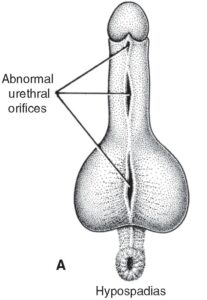
A urethral opening on the dorsum of the penis is called epispadias.
This condition is much rarer, resulting from an abnormal relationship between the genital tubercle and urethral plate. It can also be associated with defects of bladder formation (exstrophy of the bladder).
Table 38.1. Comparison chart of fetal structures to adult structures
|
Embryonic primordium |
Definitive structure in the male |
Definitive structure in the female |
Non-functioning remnants in the male | Non-functioning remnants in the female |
|---|---|---|---|---|
|
Indifferent gonad with
|
Testis with
|
Ovary with
|
|
|
| Mesonephric (excretory) tubules | Efferent ducts |
|
Paradidymus |
Epo- and paroophoron |
| Mesonephric (Wolffian) duct |
Epididymis Ductus deferens Ejaculatory duct Seminal vesicle Ureter Renal pelvis and calyces, collecting ducts |
Ureter Renal pelvis and calyces, collecting ducts |
Appendix of epididymis | Gartner’s duct |
| Paramesonephric (Müllerian) duct |
Uterine tube Uterus Superior portion of vagina |
Appendix of testis | Hydatid of Morgagni | |
| Urogenital sinus |
Prostate Bulbourethral gland Urinary bladder Male urethra |
Inferior portion of vagina Greater and lesser vestibular glands Urinary bladder Female urethra |
Prostatic utricle | |
| Genital tubercule (Phallus) | Corpus cavernosum of penis | Clitoris, glans of clitoris | ||
| Genital folds |
Corpus spongiosum of the penis Glans of penis |
Labia minora Vestibular bulb |
||
| Genital swellings | Scrotum | Labia majora | ||
| Gubernaculaum |
Proper ovarian ligament Round ligament of uterus |
Gubernaculum of testis | ||
| Paramesonephric tubercle | Seminal colliculus | Hymen |
(ADAPTED) SCHUENKE, ATLAS OF ANATOMY VOL. 2 , 2ND ED., TABLE 6.54A ©THIEME MEDICAL PUBLISHERS, INC. ALL RIGHTS RESERVED.