- Optional Reading
- Clinically Oriented Anatomy, 8th ed., Overview of mediastinum section through Clinical box: Heart.

Would a review be helpful?
We already covered the location of the pericardium and heart, the pericardium, and the external anatomy of the heart in the introduction to the thoracic cavity.
Internal anatomy of heart
Overview of chambers
The adult heart consists of four chambers: right and left atria and right and left ventricles. It is completely divided into right and left sides. The right side of the heart receives deoxygenated blood from veins, which is then pumped through the pulmonary trunk and pulmonary arteries to the lungs. After oxygenation in the lungs, blood returns to the left atrium through four pulmonary veins, two from each lung. Blood leaves the left atrium and enters the left ventricle, after which it is then pumped through the aorta to all tissues of the body.
The two upper chambers are the thin-walled atria. These are separated from each other by an interatrial septum. In the gross lab note that the internal surfaces of the atria have both smooth and rough parts: the smooth parts receive blood from veins while the rough parts are the ear-shape structures called auricles. (Clinicians refer to the auricles as the “atrial appendages.”)
The lower chambers are the thicker ventricles, separated from each other by the interventricular septum. For purposes of studying the flow of blood through the heart and for understanding the embryonic development of the internal heart, it is important to think of each ventricle as having two distinct parts: inflow portions and outflow portions.
The inflow portions of the left and right ventricles receive blood directly from the corresponding atria via the atrioventricular orifices. The inflow portions are thus located directly below the atrioventricular valves: the right inflow portion is below the tricuspid valve and the left inflow portion is below the mitral valve. In the gross lab observe that the inflow portions are rough in texture = they contain jagged fascicles of cardiac muscle called trabeculae carneae and nipple-like projections called papillary muscles.
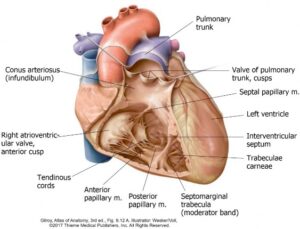
The outflow portions of the left and right ventricles receive blood from the inflow portions and eject it from the heart through the pulmonary and aortic valves into the great arteries leaving the heart. The outflow portion of the right ventricle is located just below the pulmonary valve and it directs blood through the valve into the pulmonary trunk. The outflow portion of the left ventricle is located below the aortic valve and it sends blood through the valve into the ascending aorta. Note in the gross lab that the outflow portions of the ventricles are smooth in texture and they receive special names: the outflow portion of the right ventricle is called the infundibulum or conus arteriosus, while the outflow portion of the left ventricle is called the aortic vestibule.
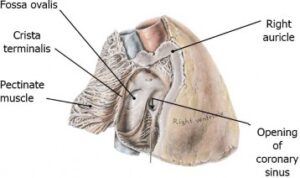
This chamber receives blood from the superior vena cava and inferior vena cava. Adjacent to the opening of the IVC is a flap of tissue called the valve of the IVC (Eustachian valve), a remnant of a fetal structure that directed incoming blood in the IVC toward the foramen ovale in the fetus. The coronary sinus, which receives the venous blood from cardiac veins of the heart, also enters the right atrium. The valve of the coronary sinus (Thebesian valve), a flap of tissue adjacent to the opening of the coronary sinus, may prevent backflow of blood when the atrium contracts. The interior of the right atrium is divided into two parts by a ridge called the crista terminalis. The area posterior to the crista terminalis is the sinus venarum, into which the two vena cavae open. The walls of the sinus venarum are smooth. The anterior half of the atrium is the right auricle. In contrast to the posterior half of the chamber, the walls of the auricle are rough and exhibit numerous muscular ridges called pectinate muscles; these extend into the auricle from the crista terminalis.
The interatrial septum separates the atria. It is characterized by a depression on the right side that is located above the orifice of the inferior vena cava. This is the fossa ovalis, which represents the embryonic location of the foramen ovale. Foramen ovale allows the blood to flow from right atrium to left atrium before birth and represents an important shunt for fetal circulation.
The right ventricle occupies most of the sternocostal surface. The walls of the myocardium of the inflow part of the ventricle exhibit features similar to those in the left ventricle: trabeculae carneae and papillary muscles. One of the trabeculae carnae in the right ventricle forms a bridge-like band of cardiac muscle called the septomarginal trabecula (a.k.a. moderator band). It connects the interventricular wall with the anterior wall of the ventricle. The right bundle branch, part of the conducting system of the heart, traverses this structure. The infundibulum (conus arteriosus) is located superiorly in the chamber and is the outflow part of the right ventricle. The walls of the infundibulum are smooth.
Because the heart pumps blood in one direction, it is provided with valves that prevent regurgitation (backflow) of blood from areas of higher pressure to those with lower pressure.
The right AV or tricuspid valve surrounds the orifice between the right atrium and right ventricle. This valve consists of three cusps (anterior, posterior, and septal) named according to their position. There are three corresponding papillary muscles in the right ventricle. Tough bands of tissue called tendinous cords (chordae tendineae) arise from the apex of each papillary muscle and extend to the cusps. Each cusp receives chordae tendinae from two papillary muscles. The papillary muscles contract when the ventricles contract, placing tension on the fibrous cords which hold the cusps tight and prevent them from being everted into the atrium during ventricular contractions (this would lead to regurgitation of blood into the right atrium).
The pulmonary valve is a semilunar valve that is situated between the right ventricle and the pulmonary trunk. It consists of three cusps, named anterior, right, and left. The pulmonary valve prevents regurgitation of blood into the ventricle after ventricular contraction ceases and the blood begins to flow back toward the ventricle.
The left atrium is also divided into two parts, but without a demarcation line like the one seen in the right atrium. The posterior region of the atrium that receives the four pulmonary veins carrying oxygenated blood from the lungs has a smooth surface. The anterior portion of the left atrium contains the ear-like auricle. This region contains pectinate muscle and is the rough part of the atrium.
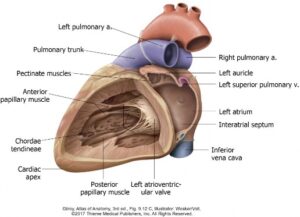
The left ventricle lies in front of the left atrium. Its cavity is circular in profile when viewed in cross-section, whereas the right ventricle is semilunar (C-shaped). The myocardium is thickest in the left ventricular wall. Rough trabeculae carneae and two stout papillary muscles line the interior of the inflow part of the left ventricle. The outflow portion of the left ventricle is smooth and is named the aortic vestibule. Above the vestibule is the aortic orifice through which blood is ejected into the ascending aorta.
The mitral valve (left atrioventricular valve) is located between the left atrium and the left ventricle. This valve has two cusps (anterior and posterior) which are connected by tendinous cords and to their respective papillary muscles. The shape of the valve with two cusps is said to resemble a miter (“bishop’s hat”), thus its name.
Blood flow through the aortic orifice is regulated by the aortic semilunar valve, which is similar to the pulmonary valve in having three semilunar cusps. Similar to the pulmonary semilunar valve, the aortic valve prevents the flow of blood back into the left ventricle from the aorta after ventricular contraction ceases. Just above each cusp, the wall of the aorta is swollen a bit, producing a dilatation called an aortic sinus. The sinuses and the cusps are named right, left, and posterior. From the left and right aortic sinuses originate the right and left coronary arteries that supply the heart with its blood.

The IV septum is placed in an oblique orientation, such that its anterior part is toward the left, while its posterior part is to the right. The IV septum bulges into the cavity of the right ventricle (this can be seen easily in a cross section). Most of the IV septum is very thick = this is the muscular part of the IV septum. The upper portion however is much thinner. This clinically important part is called the membranous part of the IV septum.
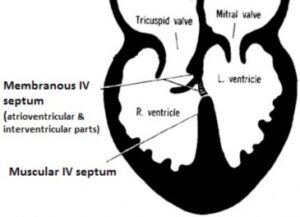
The mitral valve attaches high on the left side of the IV septum, but the septal cusp of the tricuspid valve is attached lower on the right side of the septum. Because of this, part of the membranous IV septum lies between the right atrium and left ventricle. This is the atrioventricular portion of the membranous IV septum. In the gross lab it is thus possible to place the thumb and index finger from the same hand in the left ventricle and the right atrium, respectively, and have the A-V septum separating your digits. The portion below the septal cusp of the tricuspid valve is a true interventricular portion of the membranous IV septum. (See Figure 33.5.)
Clinical correlation
Ventricular septal defects (VSDs) are the most common type of congenital defects of the heart. Because the pressure in the left ventricle is higher than that of the right, if a VSD is present, oxygenated blood is forced from the left ventricle to the right ventricle. Left-to-right shunting of blood increases blood flow to the lungs, which raises pressure in lung arteries and potentially leads to pulmonary hypertension. Since the atrioventricular bundle (Bundle of His), part of the heart’s conducting system, passes through the region of the membranous IV septum, a surgeon must be aware of this when repairing the VSD in this area, in order not to damage the heart’s normal rhythm.
Auscultatory areas
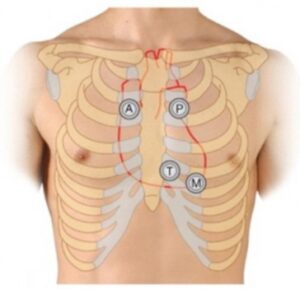
Physically, all four of the heart valves are located close to one another, along a line that runs roughly through the coronary sulcus of the heart. Fortunately, sounds produced when heart valves close are transmitted through the blood as it flows away from the valves toward the chest wall. Thus, there are locations on the chest wall where the sounds associated with the individual valves are heard best. These are known as the auscultatory areas.
Mnemonic
Mnemonics for remembering these (use the first letter of the valve’s name, starting with the aortic valve): “Apple Pie Tastes . . . Mmmm” or “A Pretty Tall Man.”
Blood supply of the heart
Coronary arteries
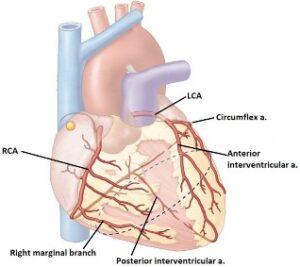
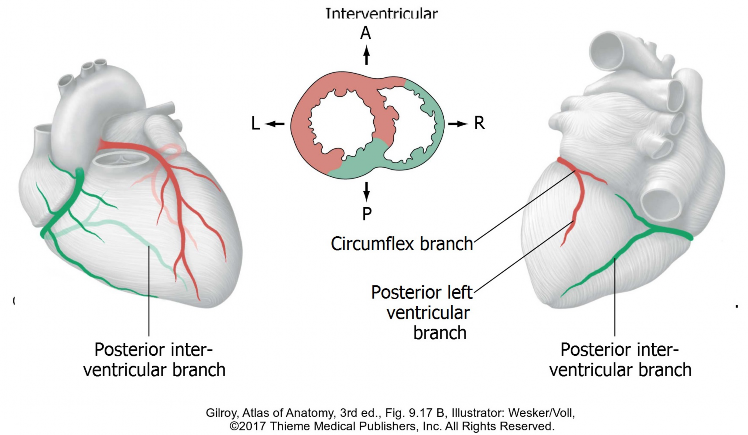
The right coronary artery arises from the right aortic sinus above the right cusp of the aortic valve, and runs downward in the coronary sulcus between the right atrium and the right ventricle. After giving off a right marginal branch, the right coronary artery continues onto the posterior side of the right ventricle as the posterior interventricular branch, also called the posterior descending artery (PDA) by clinicians. This artery runs in the posterior interventricular sulcus, a posterior groove between the two ventricles.
The left coronary artery originates from the left aortic sinus above the left cusp of the aortic valve. It passes posterior to the pulmonary trunk and is a very short vessel. Just distal to its origin, the artery bifurcates into an anterior interventricular branch (called the left anterior descending artery = LAD, by clinicians) and a circumflex branch. The anterior interventricular branch descends in the anterior interventricular sulcus towards the apex of the heart. It supplies both the right and left ventricles, and most of the interventricular septum. The circumflex branch continues toward the left in the coronary sulcus and then “bends” (thus the name) on to the posterior wall of the heart. If it reaches the posterior interventricular sulcus, it may give rise to the posterior interventricular artery. This variation is called the left dominant pattern of blood supply.
Coronary artery dominance
Coronary artery dominance is determined by which of the coronary arteries (right or left) gives rise to the posterior interventricular artery. The right dominant pattern is most common (~70%).
Clinical correlation
Coronary artery dominance has clinical implications in disease stats (myocardial ischemia and infarction) and in surgery (coronary artery bypass grafting).
- Left ventricle
- Left atrium
- Anterior wall of right ventricle
- Anterior part of IV septum
- Atrioventricular (AV) bundle and left and right bundle branches (conducting system).
- Right ventricle
- Posterior IV septum (in a right dominant pattern)
- Posterior wall of left ventricle (in a right dominant pattern)
- Right atrium
- Interatrial septum
- Sinu-atrial (SA) and atrioventricular (AV) nodes (conducting system)
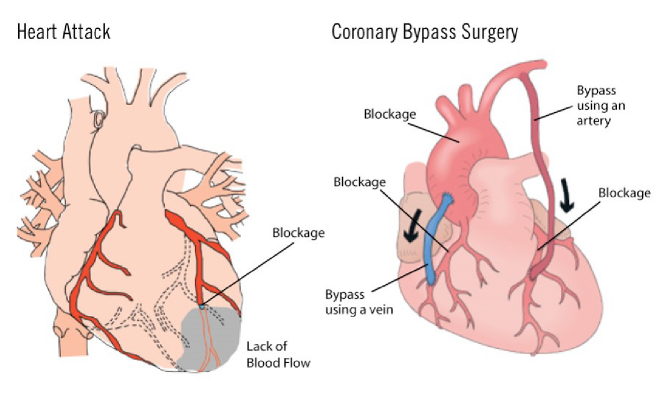
Clinical correlation
Coronary artery bypass graft (CABG) is a type of surgery to improve blood flow to the heart in patients who have narrowed or blocked coronary arteries. A healthy segment of vein (taken from the great saphenous vein in the leg) or artery (internal thoracic artery) is connected (grafted) around the narrowed or block artery. In the case of the artery, the distal part of the internal thoracic (internal mammary) artery is detached from the chest wall and connected to the affected coronary artery distal to the blockage.
Cardiac veins
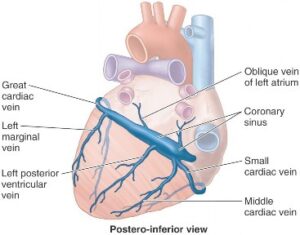
Cardiac veins collect deoxygenated blood from the heart wall. Blood in cardiac veins passes to the coronary sinus, a large vein that empties its contents into the right atrium.
-
- The great cardiac vein commences in the anterior interventricular sulcus. It drains blood upward along the anterior interventricular artery (LAD). The vein passes posteriorly around the heart to enter the coronary sinus.
- The middle cardiac vein passes upward in the posterior interventricular sulcus alongside the posterior interventricular artery.
- The small cardiac vein begins on the anterior surface of the heart where it accompanies the right marginal branch of the right coronary artery.
- Anterior cardiac veins drain blood from the anterior surface of the heart. These are not tributaries of the coronary sinus, instead they drain directly to the right atrium through the heart wall.
Innervation and conducting system of the heart
The heart is innervated by both parasympathetic and sympathetic parts of the autonomic nervous system. These nerves serve to modifythe rate and strength of the heartbeat. Their inputs however do not initiate or maintain the heartbeat. Located in the myocardium are specialized cardiac muscle cells that are the intrinsic “pacemakers.” These cells initiate and conduct impulses in an autorhythmic manner throughout the rest of the myocardium.
Conducting system
The conducting system of the heart consists of the sinuatrial (SA) and atrioventricular (AV) nodes, the atrioventricular (AV) bundle (of His), and right and left bundle branches which terminate as Purkinje fibers (subendocardial branches) in the myocardium. All of these conducting components are specially differentiated cardiac muscle cells. They are not nerves!
- Sinuatrial (SA) node
- Atrioventricular (AV) node
The specialized cardiac muscle cells of the SA node are located in the wall of the right atrium, near the entrance of the superior vena cava. The SA node functions in the heart as the pacemaker, which spontaneously generates approximately 70 impulses per minute. The activity of the pacemaker is influenced by the fibers of the autonomic nervous system (speed up or slow down).
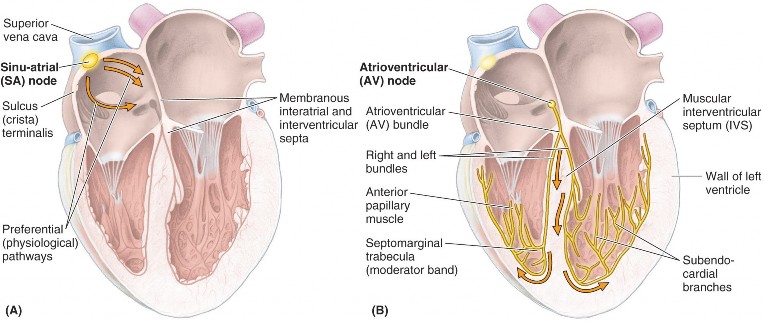
The AV node lies in the interatrial septum near the opening of the coronary sinus and the attachment of the septal cusp of the tricuspid valve. From the interatrial septum, the node extends through the fibrous skeleton of the heart toward the ventricles as the atrioventricular (AV) bundle (Bundle of His). This extension connects the AV node with the ventricles.
In the interventricular septum, the AV bundle divides into right and left bundle branches that pass toward the apex of the heart. The right branch supplies the right ventricle via the septomarginal trabecula (moderator band), whereas the left branch enters the ventricular wall along the trabeculae carneae.
Fibrous skeleton of the heart
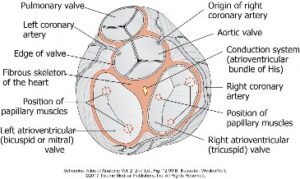
The fibrous skeleton is made of dense connective tissue and is situated within the myocardial layer of the heart wall deep to the coronary sulcus—thus, it is sandwiched between the atria and ventricles. In addition to serving as the scaffolding to which bundles of cardiac muscle tissue attach, the fibrous skeleton contains four fibrous rings to which the cusps of the four heart valves are anchored. Functions of the fibrous skeleton include:
- Framework for the attachment of cardiac muscle bundles.
- Attachment and support of the four heart valves.
- Acts as an insulator that separates the electrical activity of the atria from that of the ventricles.
This isolates electrical and contractile activity in the atria and prevents it from spreading too quickly to the ventricles, so that the blood in the atria fully empties into the ventricles before systole begins. The only part of the conducting system that links the two sets of cardiac muscle (atria and ventricles) is the atrioventricular bundle, which passes through the fibrous skeleton. Electrical signals in the AV bundle are “delayed” slightly due to the resistance in the fibrous skeleton—this delay ensures that the atria have finished contracting before the ventricles do so.
- Tying it all together with Acland