This page will help demystify your medical school experience.
A broad, high-level overview of our curriculum
The purpose of this page is to show the overall patterns to what, when, and how you are learning. While we strive to deliver a consistent schedule, there will be exceptions to the information given. For session-specific information, see E.Flo MD (our learning management system).
This information is geared toward the pre-clerkship years, although much of it pertains to all four years of our curriculum.
Our curriculum undergoes constant evaluation and refinement. Changes may occur from year to year in order to improve the educational program. The College of Medicine reserves the right to make policy and regulatory changes at any time.
Glossary of terms
- AHD: Academic Half-Day
- APM: Art and Practice of Medicine
- CBL: Case-Based Learning
- CBSE: Comprehensive Basic Science Exam
- CCW: Clinical Campus Week
- CPE: Community Patient Experience
- FMS: Foundations of Medical Science
- IL: Independent Learning
- IPE: Interprofessional Practice and Education
- LIC: Longitudinal Integrated Clerkship
- LMH: Leadership in Medicine and Healthcare
- LMS: Learning-Management System
- MKA: Mastery Knowledge Assessment
- OSCE: Objective Structured Clinical Examinations
- PD: Professional Development
- SDL: Self-Directed Learning
- SDIL: Self-Directed Independent Learning
- SLC: Student Learning Center
- SL: Service Learning
- VCC: Virtual Clinical Center
- WKC: Weekly Knowledge Check
- WBA: Workplace-Based Assessment
Foundations of Medical Science (FMS)
The Foundations of Medical Science (FMS) courses are designed to equip students with the knowledge, skills, attitudes, character traits, professionalism, and behaviors essential to becoming excellent physicians.
The curriculum is organized by body system, and that is how you will be assessed, too.
Body systems are taught in the following order, increasing in developmental complexity:
-
- Hematopoetic
- Urinary/renal
- Cardiovascular
- Respiratory
- Integumentary
- Musculoskeletal
- Endocrine
- Reproductive
- Digestive
- Behavioral
- Neurological
- Complex immune
Every body system is complemented by relevant threads:
Anatomy (including embryology)
Cellular and molecular science (e.g., biochemistry)
Ethics
Genetics
Health equity
Histology
Information literacy
Immunology
Interprofessional education
Microbiology and infectious disease
Nutrition
Pathology
Pharmacology
Physiology
Population and community health
Professional identity formation
Radiology
The backbone of FMS courses is a combination of the Art and Practice of Medicine (APM) and Case-Based Learning (CBL).
MS1, MS2
Class format:
-
-
Large groups
-
Workshops
-
Anatomy lab small groups (4 students)
-
Format of learning materials:
-
-
PPT
-
PDFs
-
Rise guides
-
Educational applications
-
Location of learning materials:
- MKA
- Pin tests
- WKC
- Assignments
Art and Practice of Medicine (APM)/Clinical Skills
The Art and Practice of Medicine (APM) is a longitudinal component of the pre-clerkship curriculum that covers foundational skills required of a physician, including history-gathering with an emphasis on empathetic communication and professionalism, physical examination, clinical reasoning, written documentation, and oral presentation. In APM, students explore applied medical ethics, health equity concepts, and evidence-based medicine within clinical patient care.
MS1, MS2
The APM course is delivered in multiple locations on the health professions campus in the Spokane Medical Education Department (SMED) building and the virtual clinical center (VCC). Students work in both large- and small-group rooms, as well as simulated patient care environments.
APM is the clinical skills course of the curriculum focusing on active learning and simulated patient care practice. Faculty and students partner together to promote a student-centered learning environment that fosters growth and development through directed feedback and self-reflection. Students engage in various hands-on activities supporting application of learned skills through small-group interactions, physical examination practice, role play, simulated and real patient encounters, large-group discussions, and peer evaluation and review.
APM is assessed in a holistic manner capturing student performance through many different evaluation methods. These include participation in course work, skills-based and global assessments, and monitoring professional attributes. All of these components together determine successful student progression through the APM curriculum.
Case-Based Learning (CBL)
Case-Based Learning (CBL) is a student-led, faculty-facilitated, small-group learning environment where students explore clinical cases. Each clinical case provides an opportunity to apply knowledge constructs from across the curriculum. The list of cases has been selected to cover common and important (do not miss) medical conditions. These cases are intended to link basic science concepts with clinical concepts, develop clinical reasoning, and promote contextualization of patient care as it relates to societal challenges, health care disparities, health systems, and ethics.
See the Case-Based Learning (CBL) Student guide for more information.
MS1, MS2
Class format:
-
-
Small-groups (8–9 students)
-
Format of learning materials:
-
-
iBooks (epubs)
-
Location of learning materials:
-
-
Your case is in the Books app on your iPad.
-
Case files are beamed to iPads four times a week:
-
Friday afternoon (preview of next week’s case)
-
Monday, Wednesday, and/or Friday, right before the CBL session
-
-
Cases are also available on E.Flo MD right before the CBL session.
-
- WBA. Facilitators assess participation, development, collaborative skills, professionalism, clinical reasoning, etc.
- MKA
- WKC
- Assignments for missed sessions
The MedTech team has some additional information about how to use the technology used in CBL:
Leadership in Medicine and Healthcare (LMH)
Leadership in Medicine and Healthcare (LMH) courses span all four years of our program. These courses are designed to equip future physicians with vital leadership skills that will enable them to lead teams and organizations, facilitate change and lead transitions, and progress in their own professional identity. Students have opportunities to apply leadership skills in all of their small-group learning experiences in the program, and we have heard from alumni that these skills have been helpful in residency.
All four years
Class format:
-
-
Large-group lectures and small group discussions
-
Asynchronous Rise modules
-
Asynchronous lessons
-
Format of learning materials:
-
-
PPT
-
PDF
-
Rise guides
-
Location of learning materials:
- Reflection
- Specific assignments
- Final LMH capstone project for pre-clerkship and clerkship years
Medschlr
Scholarship and Discovery (Medschlr) is a longitudinal series of courses that introduces students to what it means to be a scholar in the field of medicine. Medschlr 500 introduces students to epidemiology, statistics, study designs, and research ethics as students participate in journal club and practice identifying, applying, and appraising scientific evidence.
All medical students participate in scholarship through the Foundations of Scholarship and Discovery courses. They have the opportunity to delve deeply into one topic or into multiple topics of interest. The focus may be on traditional research or on other types of research, such as arts and humanities, medical education, rural health initiatives, bioengineering, leadership, etc. Working independently or as part of a multidisciplinary research team, students gain firsthand experience designing and conducting original research, including developing research questions, collecting and analyzing data, and interpreting findings. This prepares students for career research and promotes a habit of lifelong learning for all physicians.
While students are working independently, they have regular check-ins with their advisors (different than the supervisor of their project), at the mid-point of the course and at the end, to support their progress. Students meet in small groups to give a status update on their learning plan, discuss pitfalls and challenges they have encountered, report discoveries, and present any data or other information generated.
- 500AB: MS1, winter and spring
- 520/540: Based on individual student pathway
Class format:
-
- Large-group lectures and small-group discussions
- Asynchronous Rise modules
500AB:
-
- Medschlr Exam (500 Only)
- Assignments
- WBA (500 only)
520/540:
-
- Independent learning: Oral presentation
- Group check-in: Supervisor and advisor feedback forms
Additional Program Requirements
The following components are part of Foundations of Medical Science but occur with less frequency than the others.
Clinical Campus Week (CCW)
Students go to their clinical campuses for one week each term (in the first 5 terms of medical school). These weeks are designed for students to familiarize themselves with their regional campus communities, build relationships with their campus team members and with clinical partners, develop their professional identities in the clinical environment, and explore a societal theme that is significant to healthcare delivery in Washington State.
MS1, MS2
Class format:
-
-
Guest speakers/lecture
-
Clinical observation
-
Small-group projects/presentations
-
Location of learning materials:
-
-
Student handbook
The assessment method depends upon the CCW.
-
- Reflection
- I-PAT
- WBA
Community Patient Experience (CPE)
Students see real patients in a clinical setting for a half-day once per term in four of the terms in the pre-clerkship.
Reflection assignment.
Independent Learning (IL)
Independent Learning (IL) is defined as required activities outside of formal education settings, including assigned readings (often pre-class activities designed to prepare the student for an educational session), online modules, educational videos, assignments, and other required activities.
Interprofessional Practice and Education (IPE)
There is an abundance of evidence demonstrating that effective team-based patient care is associated with improved outcomes, for individual patients as well as the population. Since effective teamwork is best learned by interacting with a variety of team members, our interprofessional education (IPE) thread provides six opportunities across the pre-clerkship for medical students to learn about, with, and from students from up to ten other healthcare professions. The design of session content is based on the InterProfessional Education Collaborative (IPEC) core competencies related to values and ethics, roles and responsibilities, interprofessional communication, and teams and teamwork.
MS1, MS2
Class format:
-
-
Small-group collaboration
-
Case-based practice
-
Location of learning materials:
-
-
Zoom
-
- Reflection
- I-PAT
- Survey
Professional Development (PD)
It is important for physicians to be life-long learners. Physicians have a duty to keep informed to better serve their patients and are also required by law to complete a certain number of Continuing Medical Education (CME) credits to maintain their licensure. Our professional development requirements help students develop this habit of keeping informed. Students choose any topic of interest to them.
Students are required to attend at least one Professional Development of their choosing, one or more hours in length, every term in the first and second year of the curriculum (MED FMS 501–513).
Assignments.
Self-Directed Learning (SDL)
Per accreditation with the LCME: “The faculty of a medical school ensure that the medical curriculum includes self-directed learning experiences and unscheduled time to allow medical students to develop the skills of lifelong learning. Self-directed learning involves medical students’ self-assessment of learning needs; independent identification, analysis, and synthesis of relevant information; appraisal of the credibility of information sources; and feedback on these skills.”
Self-Directed Independent Learning (SDIL)
Self-Directed Independent Learning (SDIL) is dedicated time set aside during the third year for students to focus on aspects of their education including completing assignments, reading about patients, studying for exams, attending educational conferences, and career exploration. During dedicated SDIL time, students are not expected to complete required clinical work and/or participate in scheduled rotations with providers.
Service Learning (SL)
Service-Learning is a teaching and learning strategy that integrates meaningful community service with instruction and reflection to enrich the learning experience, teach civic responsibility, and strengthen communities. The service-learning component of our program promotes a commitment to social responsibility, provides advocacy to our local community, allows for self-reflection on values, and promotes sensitivity to issues of culture, diversity, equity, and social justice.
Get more information at Service Learning.
- Final presentation in FMS 512.
- Students are required to participate in a minimum of four sessions, totaling at least 12 hours of service with a single community organization or program.
- Check-ins throughout Year 1 and Year 2 before the presentation.
- WBA related to the presentation.
Clerkship
Med Clin 521–524: Longitudinal Integrated Clerkship (LIC)
Med Clin 521–524 will introduce students to building the knowledge, skills, and professional attitudes that are required for the practice of medicine.
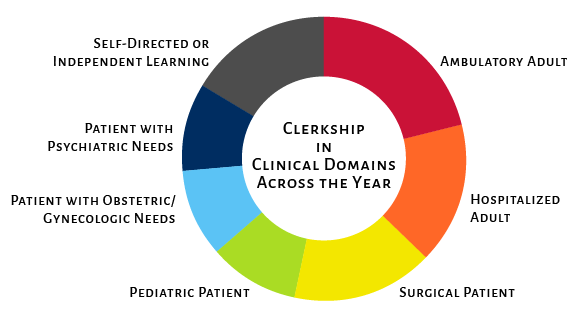
Students will work in six different care domains.
Ambulatory Adult
- Supervised care of adult patients over the age of 18. Learning will occur in affiliate clinics and ambulatory care centers and the supervising faculty preceptors will be internal medicine physicians, family medicine physicians, or specialist physicians.
Hospitalized Adult
- Supervised care of adult patients over the age of 18. Learning will occur in affiliate hospitals and the supervising faculty preceptors will be internal medicine physicians, family medicine physicians, or specialist physicians.
Surgical Patient
- Supervised care of adult or pediatric patients presenting with surgical needs. Learning will occur in affiliate clinics, ambulatory care centers, hospitals, emergency rooms, and surgery suites or centers. The supervising faculty will be surgeons or surgery sub-specialists or anesthesiologists.
Pediatric Patient
- Supervised care of pediatric patients under the age of 18. Learning will occur in affiliate clinics, ambulatory care centers, and hospitals. The supervising faculty preceptors will be pediatricians, family medicine physicians, or pediatric specialist physicians, with opportunities in select circumstances to engage in care with interprofessional preceptors and in community care sites.
Patient with Obstetric/Gynecologic Needs
- Supervised care of patients seeking Obstetrics or Gynecological care. Learning will occur in affiliate clinics, ambulatory care centers, hospitals, emergency rooms, labor suites, and surgery suites or centers. The supervising faculty are obstetricians, gynecologists, internal medicine physicians, family physicians, midwives, or OB/GYN sub-specialists.
Patient with Psychiatric Needs
- Supervised care of patients with behavioral or psychiatric needs. Learning will occur in affiliate clinics, ambulatory care centers, or hospitals. The supervising faculty will be psychiatrists, internal medicine physicians, family medicine physicians, and/or other faculty behavioral health providers [e.g., psychologists, social workers (e.g., LCSW), etc.].
Self-Directed or Independent Learning
- Clinical experiences will occur in the ambulatory and inpatient settings interleaved throughout the entire sequence of LIC courses with a small number of preceptors in each discipline. To support students’ learning during their Longitudinal Integrated Clerkship, we supplement the clinic-based, experiential learning curriculum with an Academic Half-Day (AHD).
Class location:
-
-
Clinical sites at regional campuses and in weekly half-day sessions.
-
Location of learning materials:
Academic Half-Day (AHD)
Students in their Longtitudinal Integrated Clerkship (LIC) come together each Wednesday afternoon for the Academic Half-Day: scheduled workshops, skills labs, and lectures designed to enhance student’s knowledge on common procedures and encounters they will experience in their clerkship years. Students also give case presentations that align with the predetermined themes. Facilitators are mostly community-based physicians and medical professionals, with the occasional visit from the Virtual Clinical Center (VCC) and our vice chairs.
At the regional campus, in a classroom, lab, or Virtual Care Center, depending on the topic.
Year 4
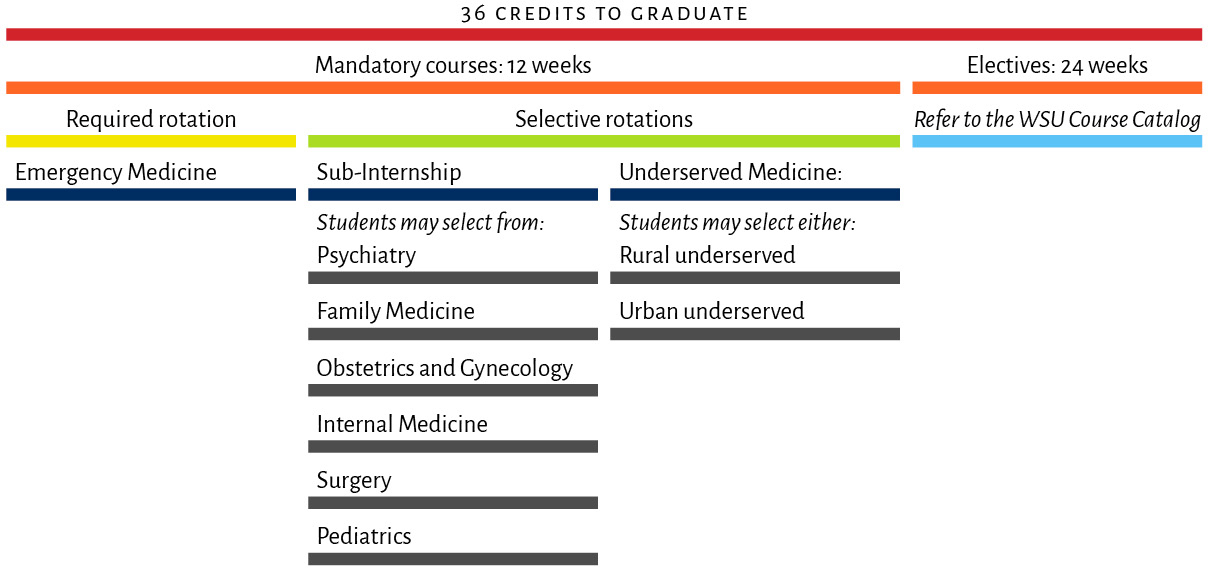 In order to graduate, students must complete 36 credits (1 week = 1 credit) in their 4th year. Twelve of those credits will be fulfilled with required courses listed in the mandatory course drop-down menu. The other 24 credits provide flexibility for students to bolster their residency applications, gauge interest in subspecialties, and complete away rotations. Only 12 credits maximum of the 24 credit electives required to graduate can be completed in a virtual or non–patient care rotation. An elective rotation is a rotation a student can choose—either clinical, non-clinical, or research—that when added to mandatory courses make up the total body of study required to complete the MD degree program requirements.
In order to graduate, students must complete 36 credits (1 week = 1 credit) in their 4th year. Twelve of those credits will be fulfilled with required courses listed in the mandatory course drop-down menu. The other 24 credits provide flexibility for students to bolster their residency applications, gauge interest in subspecialties, and complete away rotations. Only 12 credits maximum of the 24 credit electives required to graduate can be completed in a virtual or non–patient care rotation. An elective rotation is a rotation a student can choose—either clinical, non-clinical, or research—that when added to mandatory courses make up the total body of study required to complete the MD degree program requirements.
- Required rotation
- Emergency Medicine
- Selective rotations
- Sub-Internship:
- Students may select from:
- Psychiatry
- Family Medicine
- Obstetrics and Gynecology
- Internal Medicine
- Surgery
- Pediatrics
- Students may select from:
- Underserved Medicine:
- Students may select either:
- Rural underserved
- Urban underserved
- Students may select either:
- Sub-Internship:
The SLC is dedicated to supporting students’ academic excellence and professional growth throughout their academic journey. We offer a variety of personalized resources and services, including:
-
- MD program–specific learning specialists
- A dedicated disability resource professional for accommodation advocacy and support
- Learner support coaches providing individualized learning plans and occasional tutoring
- Workshops on evidence-based learning strategies, study skills, and test-taking techniques
- Personalized Step exam preparation and support
- Pre-Clerkship and clerkship/clinical coaching
- Peer tutoring available across all four years, offering both one-on-one and small group support
- An extensive catalog of learning strategies and Step resources available for asynchronous use and support
Other helpful information
Comprehensive Basic Science Exam (CBSE)
The Comprehensive Basic Science Exam (CBSE) is administered through the National Board of Medical Examiners (NBME) as a standardized assessment opportunity to gauge readiness for STEP. We use these exams as a benchmark for student growth and development longitudinally.
MS1, MS2
Electives
There are a few opportunities to take electives during the pre-clerkship. We currently have one official elective offered multiple times yearly—Community Organizing for Health Equity—and a small variety of other electives offered in the summer between first and second year.
In the 3rd year of the curriculum, there are no elective opportunities, as students are completing their Longitudinal Integrated Clerkship rotations.
In the 4th year of the curriculum, students choose elective rotations (2-week or 4-week) for a total of 24 weeks of electives in Year 4. Students choose electives from more than 100 options, including rotations in most medical specialties and varied health care settings, domestic and international away rotations, research activities, and virtual courses. Students may also design their own rotation to take with administrative approval.
MS2, MS4
Evaluation
The Evaluation team collects and synthesizes feedback from students, faculty, and staff regarding implementation of all aspects of the MD program. Feedback regarding systems and threads is routinely summarized and reported as a part of course evaluations.
- Pulse surveys
- Large-group teacher evaluation
- Small-group teacher evaluation
- CCW, APM SGFE/CBL B SGFE/LGTE 3/FMS 503 Course/LMH 503 Course/MEDSCHLR 500B Course/MEDSCHLR 500B SGFE/T3 Mistreatment/MS1 Annual
- Readiness for Clerkship
- General student survey
Objective Structured Clinical Examinations (OSCE)
The Objective Structured Clinical Examinations (OSCE) utilize multiple stations to simulate clinical experiences. Stations are designed to evaluate clinical reasoning, communication skills, clinical skills, etc.
Direct Observations occur twice in MS1, as well as fuller OSCEs in MS2, MS3, and MS4.
MS1, MS2, MS3, MS4
At the Virtual Care Clinic (VCC).
Workplace-Based Assessment (WBA)
- Performance-based opportunity for students to refine their clinical skills
- Faciliators will have a rubric to assess different aspects of your performance—rubrics will differ based on the experience
- Students will be given these rubrics prior to the assessment to prepare
Questions?
Please get in touch with questions! If you aren’t certain which department to contact, don’t worry—we’ll route your message to the right place. Our inboxes are monitored all day during the week, and we’ll respond within 1–2 days.