1Clean and identify the contents of the posterior triangle of the neck.
2Perform a deep dissection on one side of the neck to examine the sympathetic trunk and prevertebral muscles.
3Review the bony anatomy of the superior thoracic aperture and identify its contents.
4Clean and identify the structures in the root of the neck on both sides of the body.
5Clean and identify the external features and neurovascular supply of the larynx and thyroid gland.
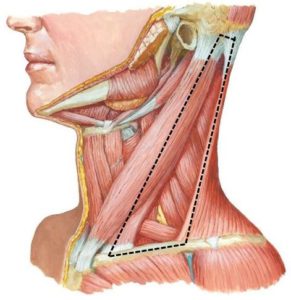
Posterior Triangle of Neck
Identify and clean the external jugular vein.
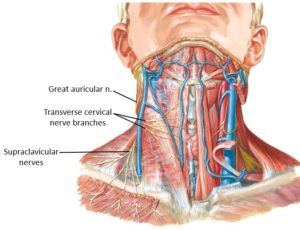
Erb’s Point (Nerve Point of Neck)
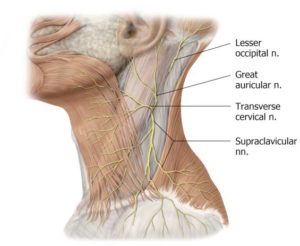
The cutaneous nerves of the neck emerge along the posterior border of the sternocleidomastoid at a common location = the midpoint between the mastoid process of the temporal bone (superiorly) and the sternum and clavicle (inferiorly). This spot is known as Erb’s point (Nerve point of the neck). See Figure 29.3. The nerves that emerge at Erb’s point pierce the investing fascia and enter the superficial fascia. These are all cutaneous nerves.
The sensory nerves of the neck are the lesser occipital, great auricular, transverse cervical, and supraclavicular nerves.
These sensory nerves, along with the ansa cervicalis (motor only) and phrenic nerve (mixed—motor and sensory), are derived from the cervical plexus (ventral rami of spinal nerves C-1 to C-4).
Examine Figures 29.2 and 29.3 before you dissect!
Dissect along the posterior border of the SCM at the Nerve (Erb’s) Point to locate these nerves:
Probe along the posterior border of the SCM to locate these nerves.
■The lesser occipital nerve (C-2) ascends along the posterior border of the SCM to the scalp. This nerve will be difficult to find.
■The great auricular nerve (C-2 and C-3) ascends toward the auricle (external ear), posterior and parallel to the external jugular vein.
■The transverse cervical nerve (C-2 and C-3) crosses the SCM deep to the external jugular. Its branches penetrate the platysma muscle to reach the skin. It is the major sensory nerve of the neck.
■The supraclavicular nerves (C-3 and C-4) descend to the top of the clavicle and shoulder.
Carefully clean the anterior border of the trapezius muscle.
The boundaries of the posterior triangle are now visible.
The tough investing fascia is the “roof” over the posterior triangle. Use the open/close scissors technique with patience to do your best to remove it.
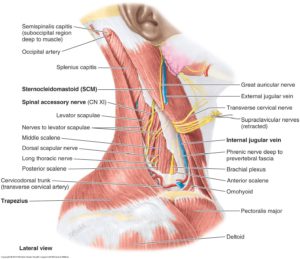
■The spinal accessory nerve enters the deep surface of sternocleidomastoid up high, just below the skull. After innervating the SCM, the spinal accessory leaves the posterior border of the muscle and crosses the posterior triangle.
■Find the spinal accessory nerve (CN XI) entering the deep surface of the reflected SCM (last lab)—trace it as it leaves the SCM and heads across the posterior triangle to the anterior border of the trapezius. It is tortuous as it crosses the neck. It travels through the posterior triangle along an imaginary line drawn between the ear lobe and acromion (summit of shoulder). See Figure 29.4.
Clinical correlation
The spinal accessory nerve is vulnerable to injury in the posterior triangle. Can you predict the consequences if it were injured here?
■Note the omohyoid muscle with its superior and inferior bellies. This muscle crosses both the anterior and posterior triangles.
Clean the prevertebral fascia in the floor of the posterior triangle as it covers the prevertebral muscles and extends over the brachial plexus.
Identify, from anterior to posterior:
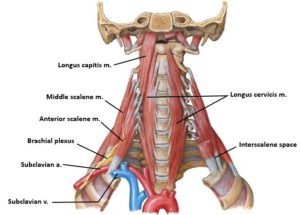
■Anterior and middle scalene muscles
■Phrenic nerve on the surface of the anterior scalene muscle
Identify the “interscalene space” between the anterior and middle scalene muscles, and the first rib. The brachial plexus and subclavian artery squeeze through this space. See Figure 29.5.
Clinical correlation
Compression of the brachial plexus and/or the subclavian artery in the interscalene space is one cause of Thoracic Outlet Syndrome.
Verify that the subclavian vein does not pass through the interscalene space; it passes anterior to the anterior scalene muscle, just behind the clavicle.
Clinical correlation
The scalene muscles (anterior, middle, and posterior) can be used as accessory breathing muscles since their distal attachments are to the first two ribs.
Root of the Neck
This is also called the “cervicothoracic” region because it is the junction between neck and thorax. So, get ready to stroll down memory lane and review a little thoracic anatomy!
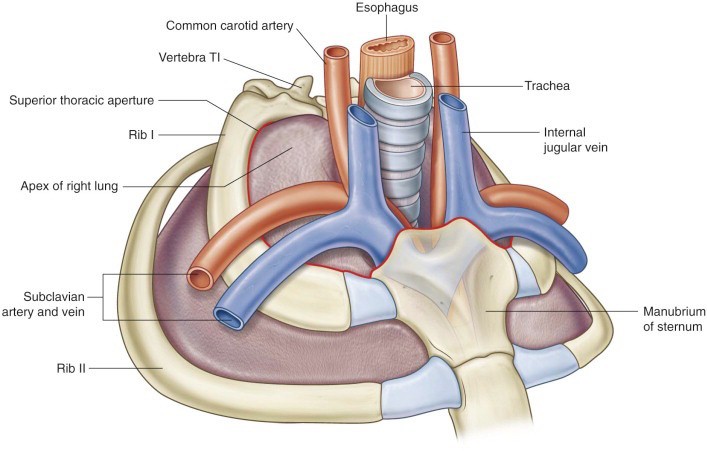
REVIEW: Boundaries of the Superior Thoracic Aperture
■T-1 vertebra
■First ribs
■Manubrium of sternum / Suprasternal notch
Which structures occupy the superior thoracic aperture? See Figure 29.6. Recall that the cervical pleura (and pleural cavity!) extends into the neck through the aperture.
Root of Neck: Deep Dissection
This should be done only on the RIGHT side.
Right side (deep dissection): Perform the following dissection procedures on the right side of the neck.
■Cut the omohyoid muscle at its central tendon and reflect its bellies.
■Cut the internal jugular vein just above its union with the right subclavian vein. Reflect the vein superiorly or remove it completely.
■Cut the common carotid artery just above the clavicle.
■Reflect or remove the subclavian vein.
■Observe the subclavian artery and brachial plexus passing through the gap between the anterior and middle scalene muscles.
■Clean the anterior scalene muscle by removing the prevertebral fascia. Identify the phrenic nerve on the anterior scalene, passing inferiorly into the thorax.
■Detach the anterior scalene muscle from the first rib. Reflect it superiorly.
Where does the subclavian artery originate on the left and on the right? Their sources are different.
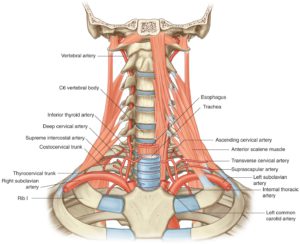
Part 1 of Subclavian Artery
From the origin of the artery to the medial border of the anterior scalene muscle. Identify these branches from Part 1.
■Vertebral artery: Ascends through the transverse foramina of cervical vertebrae and through the foramen magnum. What is the fate of the vertebral arteries inside the skull?
■Internal thoracic artery: An old friend in the thorax. You will only see its stump since it was cut with the rib cage in an earlier dissection. Flip the detached chest wall over and trace its course deep to the ribs.
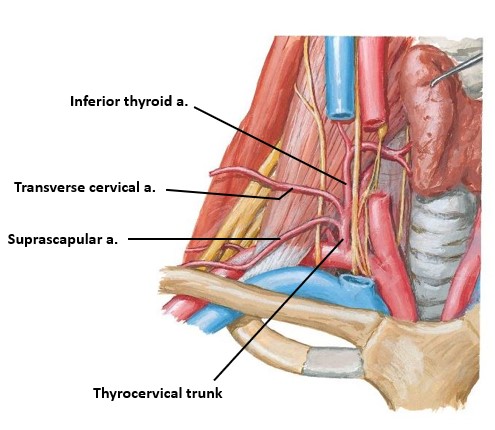
■Thyrocervical trunk: Highly variable. The “typical” pattern has three major branches (See Figure 29.8):
1Suprascapular artery: Supplies scapular muscles that move the upper limb.
2Transverse cervical artery: Has a superficial branch that supplies the trapezius and a deep branch (called the dorsal scapular artery) that supplies the levator scapulae and rhomboid muscles.
3Inferior thyroid artery: Supplies the thyroid and parathyroid glands.
Part 2 of Subclavian Artery
Behind the anterior scalene muscle. A few small unimportant branches.
Part 3 of Subclavian Artery
Between the lateral border of the anterior scalene and Rib #1.
Most often, this part has no branches. If it does, it is a variant artery called the dorsal scapular artery. This is the displaced deep branch of the transverse cervical artery, from the thyrocervical trunk.
What becomes of the subclavian artery distal to the first rib?
Right side (deep dissection): Reflect the cut end of the right common carotid artery (or remove a segment of it) and carefully clean the prevertebral fascia behind it.
With your hand, grab the “visceral unit” of the neck (pharynx, larynx, thyroid) and push it to the left. Behind the carotid sheath and visceral unit are a couple more prevertebral muscles:
■Longus capitis and longus cervicis (aka: longus colli) muscles. These muscles are located along the anterior surface of the vertebral column, behind the pharynx. See Figure 29.5. The longus capitis and longus cervicis muscles flex the head and flex the neck, respectively.
Clinical correlation
The clinically important retropharyngeal space is anterior to these muscles, between them and the pharynx.
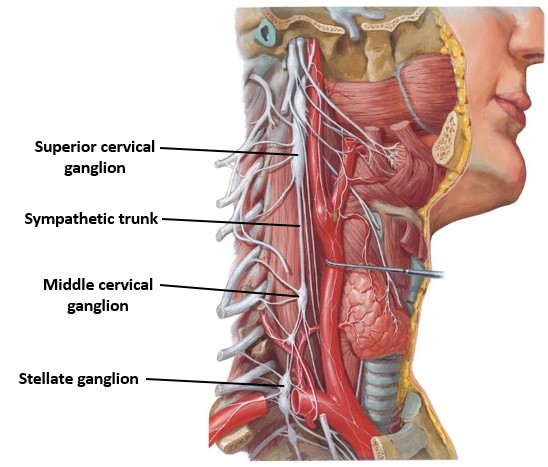
The sympathetic trunk is deep to the carotid sheath and prevertebral fascia and courses along the surface of the longus capitis and cervicis muscles. It is a thin structure in the neck with few ganglia—not like the “beaded” appearance it had in the thorax. See Figure 29.9.
■Clean the sympathetic trunk by gently teasing it out of the prevertebral fascia anterior to the longus capitis.
■Use blunt dissection to trace the internal carotid artery as high in the neck as possible. Retract the carotid to one side to find the large impressive superior cervical ganglion at C-2—the highest point of the sympathetic trunk. All of the postganglionic sympathetic neurons that supply the head have their cell bodies here.
The other ganglia of the sympathetic trunk in the neck are variable.
■A middle cervical ganglion may be present opposite the lower border of the larynx (C-6)
■Trace the sympathetic trunk through the superior thoracic aperture into the thorax. The large stellate ganglion (cervicothoracic ganglion) is situated on the head of the first rib—posterior to the subclavian artery. See Figure 29.9.
Root of Neck: Superficial Dissection
Do this on the LEFT side. Leave veins intact on this side of the neck.
Left side (superficial dissection): Clean the left venous angle (junction of left subclavian and internal jugular veins) and identify the thoracic duct entering it.
The thoracic duct typically drains to the left venous angle, entering it on its posterior side. To reach the venous angle, the thoracic duct passes deep to the carotid sheath.
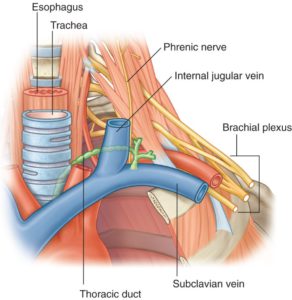
Identify the esophagus as it passes through the superior thoracic aperture. Remember that the thoracic duct is posterior to the esophagus in the mediastinum. The thoracic duct inclines to the left as it passes through the superior thoracic aperture. Clean along the left edge of the esophagus at the root of the neck to find the thoracic duct and follow it to the left venous angle. See Figure 29.10.
It is easy to be fooled here because the thoracic duct may be filled with blood and resemble a vein. It often has a “beaded” appearance and may be quite delicate, so clean it with care! The vertebral vein is also in the area (= a tributary of the brachiocephalic vein) and can be confused with the thoracic duct. It descends from the neck.
75% of the body’s lymph is drained by the thoracic duct. Can you describe the regions of the body that are drained?
The other 25% of the body’s lymph (from the right side of the thorax, right side of the head and neck, and right upper limb) is ultimately drained by the short and variable right lymph duct. Where does the right lymph duct terminate?
Neck Viscera
The viscera of the neck include the larynx, esophagus, trachea, thyroid gland, and parathyroid glands.
Identify and palpate these landmarks on the anterior neck.
■Hyoid bone
■Thyroid cartilage with laryngeal prominence (“Adam’s apple”)
■Cricoid cartilage
■Cricothyroid membrane
Trachea
Locate the trachea in the midline of the neck. Palpate the tracheal rings of cartilage.
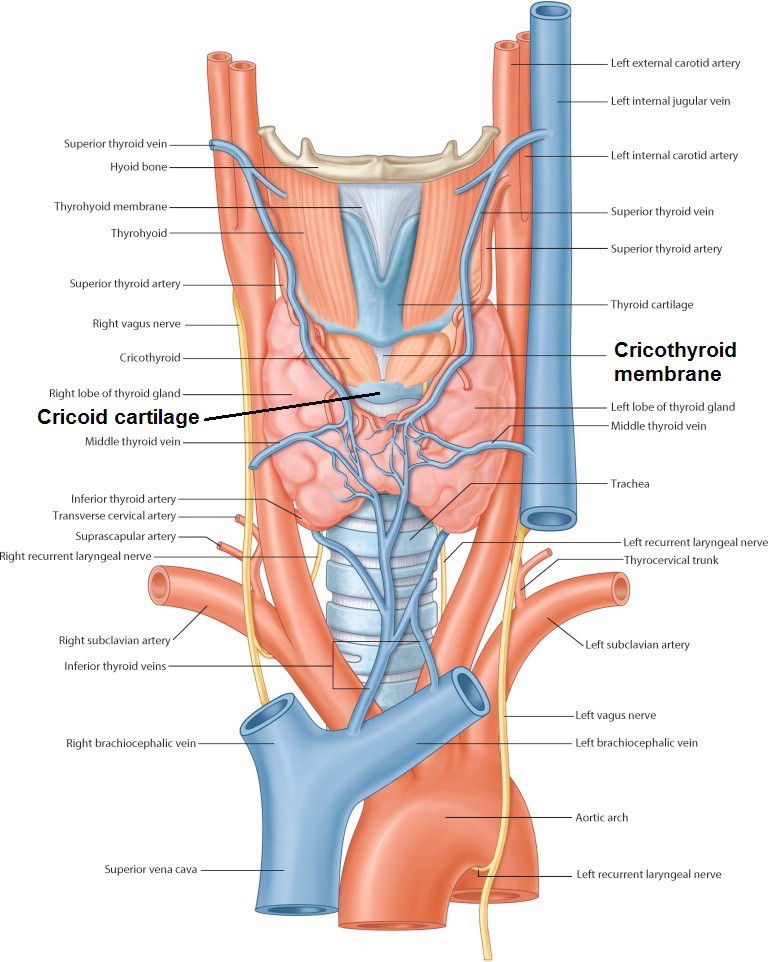
Anterior to the trachea you may see a network of veins: the inferior thyroid veins. They descend to become tributaries of the left brachiocephalic vein. See Figure 29.11.
Clinical correlation
An emergency airway in the trachea (tracheostomy) is not advised because vessels are in the way.
Furthermore, an extra artery to the thyroid gland, called the thyroid ima artery (from the brachiocephalic artery), if present, may be directly over the trachea. These are rare (<10% of folks have one).
Clinical correlation
Palpate the cricothyroid membrane and realize this is the preferred site of an emergency airway (cricothyrotomy = “crike”) because it is subcutaneous and usually has no vessels in the way.
Superior Laryngeal and Recurrent Laryngeal Nerves
Palpate the hyoid bone: body and greater horns. Move your fingers below the hyoid and feel the “mushy”, soft thyrohyoid membrane.
Left side (superficial dissection): Probe through the tissue lateral to the thyrohyoid membrane to find the superior laryngeal nerve.
We searched for this in the last lab—if you haven’t found it yet, here’s your second chance!
This nerve continues through the thyrohyoid membrane as the internal laryngeal nerve (internal branch of the superior laryngeal nerve)—it supplies the mucosa of the upper larynx (Remember = “Guardian of the Airway” = cough reflex). It is accompanied by the superior laryngeal artery, a branch of the superior thyroid artery.
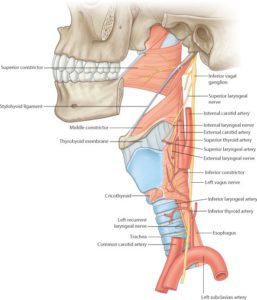
Trace the internal laryngeal nerve backwards from the thyrohyoid membrane—if you are super skilled you may find the thin external laryngeal nerve descending to the cricothyroid muscle. The external laryngeal is the other branch of the superior laryngeal nerve. It accompanies the superior thyroid artery. See Figure 29.12.
Summary
The superior laryngeal nerve branches from the vagus high in the neck. It descends to the larynx, where it divides into internal and external branches. The superior laryngeal nerve supplies the mucosa of the upper half of the larynx and one muscle of the larynx = the cricothyroid.
Now clean the left and right tracheo-esophageal grooves inferior to the thyroid gland, on both sides.
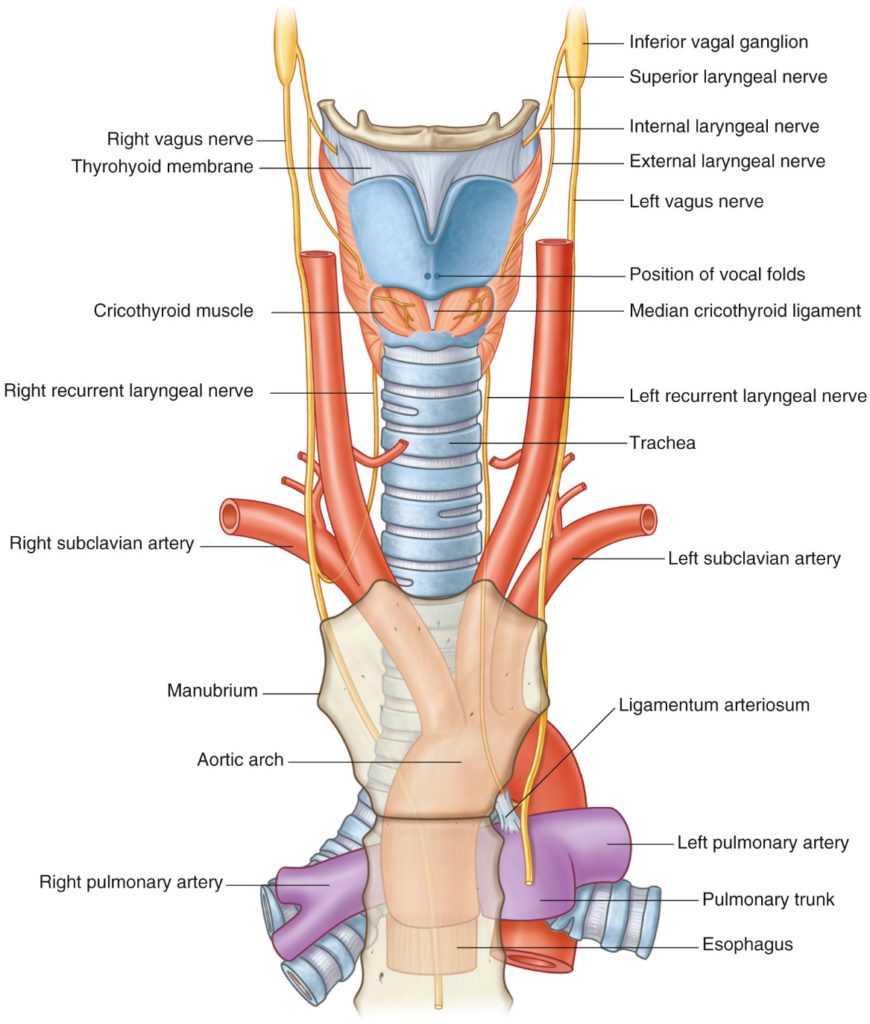
Find the recurrent laryngeal nerves ascending in the tracheo-esophageal grooves (left one loops under the arch of the aorta and the right one recurs around the right subclavian artery). The recurrent laryngeal nerves supply the mucosa of the lower half of the larynx and all intrinsic muscles of the larynx (except the cricothyroid). See Figure 29.13.
Thyroid and Parathyroid Glands
Reflect the sternohyoid and sternothyroid muscles superiorly.
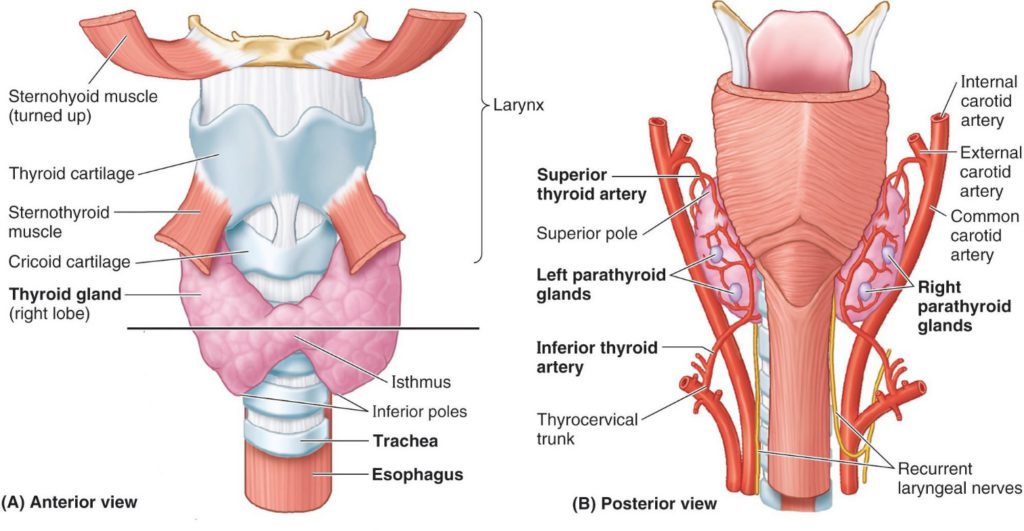
Inspect the thyroid gland and note its left and right lobes (each w/superior and inferior poles) and the isthmus crossing the trachea (not always present). See Figure 29.14.
A common anatomic variation is the pyramidal lobe. This is extra glandular tissue that rises up like a pyramid from the isthmus (or from one of the lobes).
This variation occurs along the path of the thyroglossal duct after the thyroid gland has descended from the pharynx during development. A pyramidal lobe may rise as high as the hyoid!
Review the blood supply of the thyroid gland (Figure 29.14):
■Superior thyroid artery = from external carotid
■Inferior thyroid artery = from thyrocervical trunk (subclavian artery)
Elevate the isthmus of the thyroid gland from the trachea and transect it.
Reflect one of the lobes of the thyroid toward the midline and locate the recurrent laryngeal nerve deep to the lobe (Figure 29.15).
Clinical correlation
Note how the recurrent laryngeal nerves ascend behind the lobes of the thyroid gland near the inferior thyroid arteries = IMPORTANT RELATIONSHIPS FOR THE SURGEON.
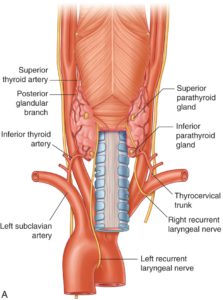
Parathyroid glands are said to relate to the posterior surfaces of the thyroid lobes, but their locations can be variable. These are tough to find in cadavers because of their size, color. and variability (due to embryology!).
The best bet is to look for the superior parathyroid glands behind the superior poles of the thyroid lobes, embedded in the capsule of the thyroid. See Figure 29.15. The superior parathyroid glands are less variable in their locations.
Thyroid gland review
Do you recall its embryology? What are its functions?
Parathyroid gland review
Do you know their embryology? [Hint: They arise from pharyngeal pouches.] What are their functions?
Checklist, Lab #29
Review your dissection and make sure you have identified each of the structures in the checklists that follow.
Bones
Review the boundaries of the superior thoracic aperture
Muscles
Sternocleidomastoid and trapezius muscles
Anterior and middle scalene muscles
Longus capitis and longus cervicis muscles
Nerves
Lesser occipital nerve = WISH LIST (might need to visit a prosection)
Great auricular nerve
Transverse cervical nerve
Supraclavicular nerves
Roots and trunks of brachial plexus (in the interscalene space)
Phrenic nerve (on the surface of the anterior scalene)
Vagus nerve
Left and right recurrent laryngeal nerves
Superior laryngeal branch of Vagus
Internal branch of superior laryngeal (internal laryngeal nerve)
External branch of superior laryngeal (external laryngeal nerve) = WISH LIST—you are a superstar if you can identify it!
Sympathetic trunk
Superior cervical ganglion
Stellate ganglion
Vessels
Subclavian arteries and veins
Vertebral artery
Internal thoracic artery (only a stump will remain)
Thyrocervical trunk
Inferior thyroid artery
Transverse cervical artery
Suprascapular artery
Superior thyroid artery (you found this during the last lab session)
Internal jugular veins
Left and right jugulosubclavian angles (venous angles)
Thoracic duct
Viscera
Trachea w/ cartilage rings
Esophagus
Thyroid gland: Left and right lobes and isthmus
Parathyroid glands = WISH LIST
Retropharyngeal space
Thyroid cartilage w/ laryngeal prominence
Cricoid cartilage
Thyrohyoid and cricothryoid membranes