1Identify the bony walls and foramina of the orbit.
2Open the orbit via a superior approach on both sides and dissect its contents.
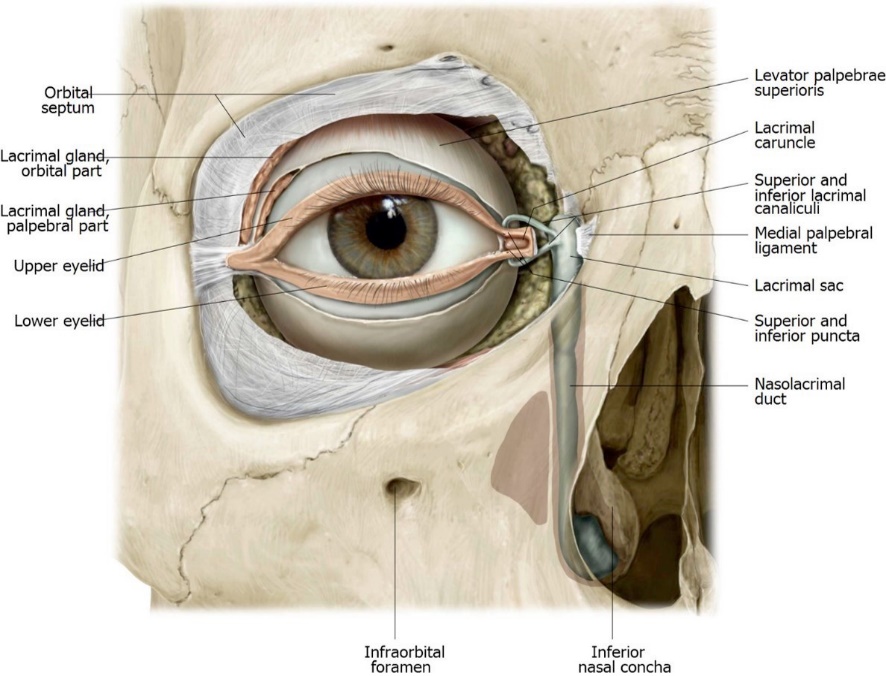
3Find the lacrimal gland in the cadaver and study the lacrimal apparatus on a model.
4Dissect the orbit from an anterior approach on both sides to study the eyelids and the structures in the floor of the orbit.
5Examine the auricle and study the external acoustic meatus.
6Open the roof of the tympanic cavity and examine it using a pen light and magnifying glass.
7Trace the course of the facial nerve in the facial canal.
Orbit
We will dissect the orbit from two approaches:
1from the superior, by removing the orbital plate of the frontal bone, and
2from the anterior, by removing or reflecting the eyelids.
In both approaches, we will focus on different structures and different tasks on the two sides of the head.
Osteology
Bony Walls and Foramina of the Orbit
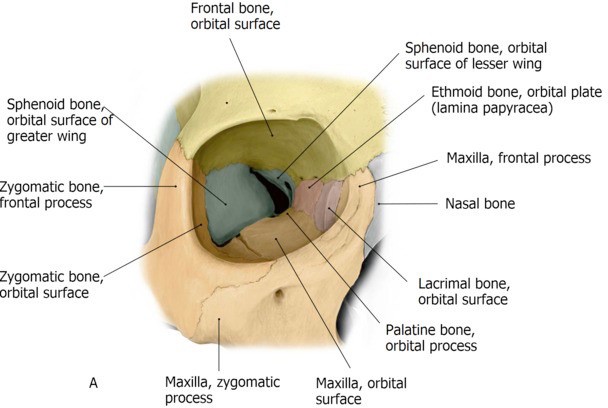
SKULL TIME: Before beginning the dissection, review the bony walls of the orbit and the foramina in the orbit that transmit nerves and vessels. Visualize the orbit as a four-sided pyramid—wide anteriorly and narrow posteriorly. Seven bones contribute to the orbital walls.
■Medial Wall
■Lacrimal bone
■Nasolacrimal canal
■Orbital plate of ethmoid bone [a.k.a. lamina papyracea]
■Anterior and posterior ethmoidal foramina
■Lateral Wall
■Zygomatic bone
■Greater wing of sphenoid bone
■Roof
■Frontal bone (orbital plate)
■Supra-orbital foramen (or notch)
■Floor
■Maxilla
■Infraorbital fissure (on the floor of the orbit) and infraorbital foramen (on the face)
■Zygomatic bone
■Apex of Orbit
■Lesser wing of sphenoid bone
■Superior and inferior orbital fissures
■Optic canal
Important Relationships of Orbit to Other Regions of the Head
■Above the orbit is the anterior cranial fossa
■Below the orbits are the maxillary air sinuses
■Medial to the orbits are the ethmoidal air cells: Separated only by the “paper thin” orbital plate of the ethmoid bone (lamina papyracea)
Both sides: Open the superior aspect of BOTH orbits.
Strip the dura mater from the floor of the anterior cranial fossa with forceps or a hemostat. With a chisel and hammer lightly score (crack) the thin orbital plate of the frontal bone. Use forceps or bone rongeurs to remove the bone fragments.
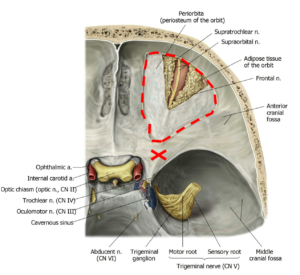
Now chip away the apex of the orbit by removing the lesser wing of the sphenoid bone.
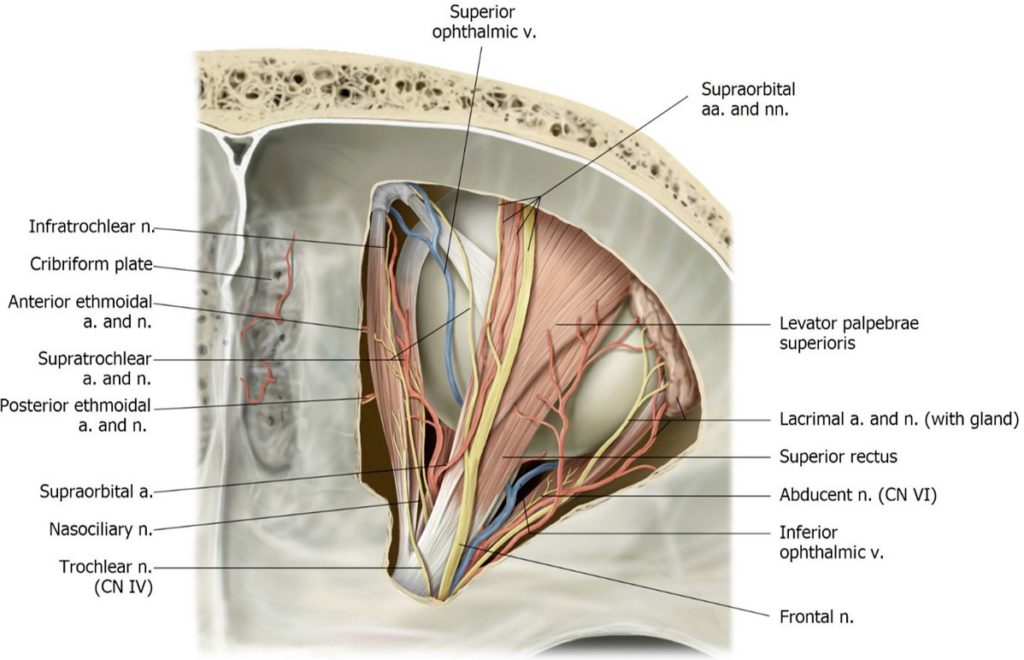
The cone-shaped orbit is now open from above, but it is covered by the periorbita (a layer of periosteum).
You should see the large flat frontal nerve just deep to the periorbita. Use scissors to carefully cut away the periorbita.
The orbit contains quite a bit of fatty tissue to cushion the eyeball. Use small forceps to pick away the fat.
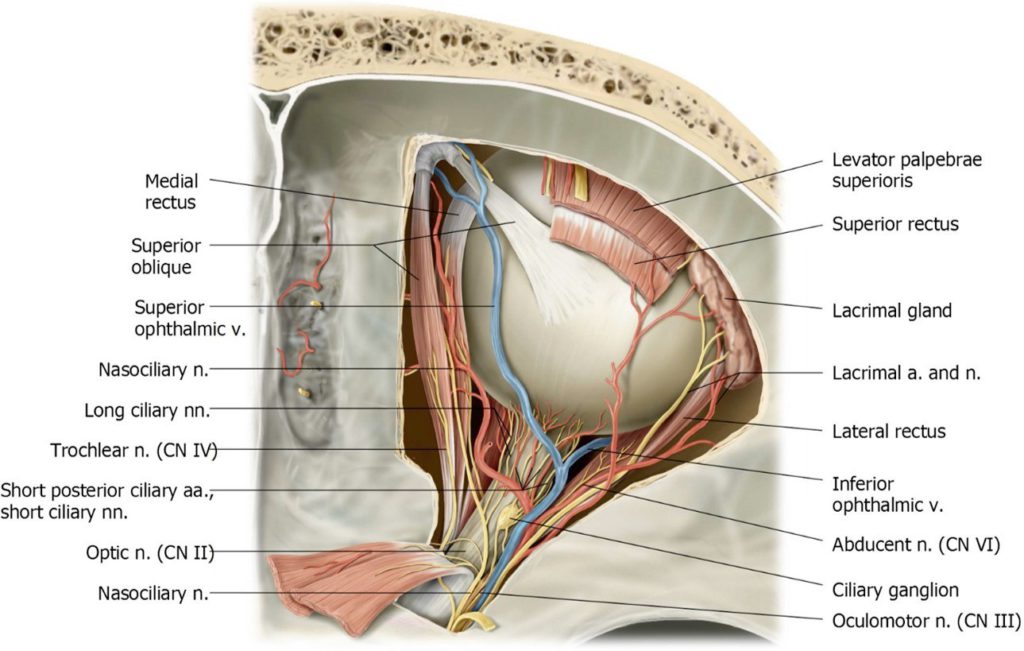
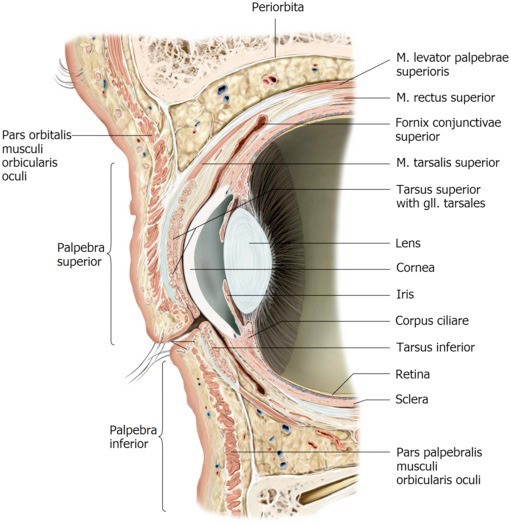
Figure 27.3.
Superior Structures of the Orbit
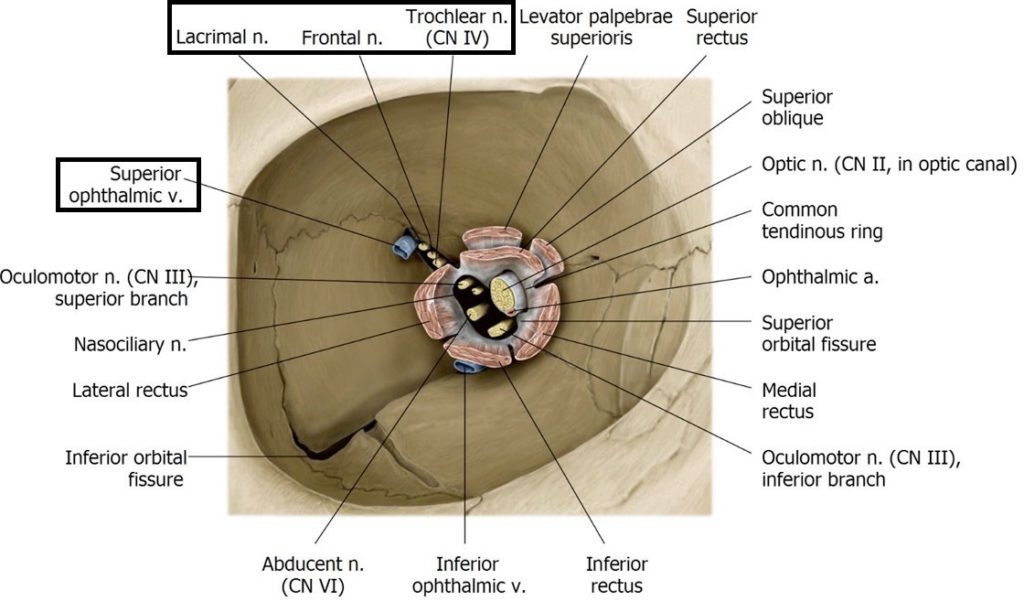
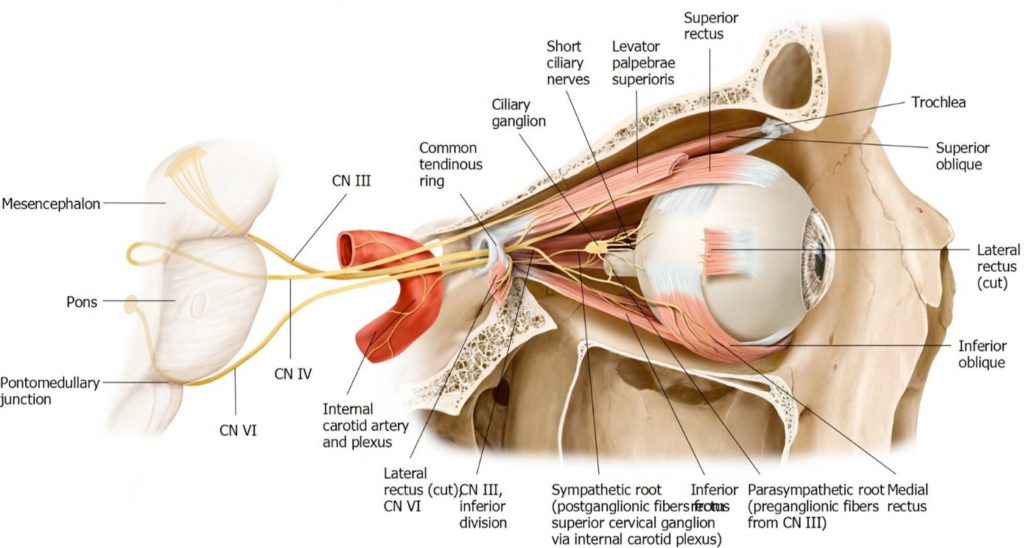
Let’s now consider that most structures enter the orbit posteriorly. Most of the extra-ocular muscles originate at the orbit’s apex.
The rectus muscles originate from a structure called the common tendinous ring (ring of Zinn) that encircles the bony apex of the orbit.
Most structures that enter the orbit posteriorly do so through the center of the tendinous ring.
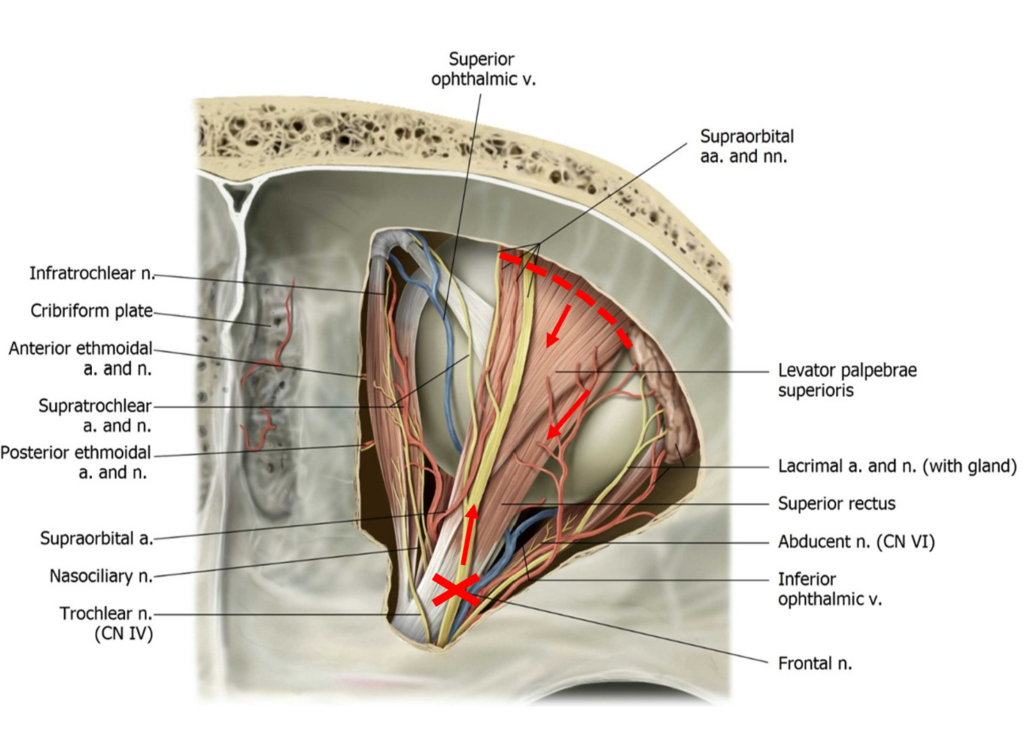
Three structures DO NOT—they enter the orbit above the tendinous ring, so these are structures that you will identify first as you dissect the orbit from a superior approach. These structures are:
What is the function of the LPS muscle?
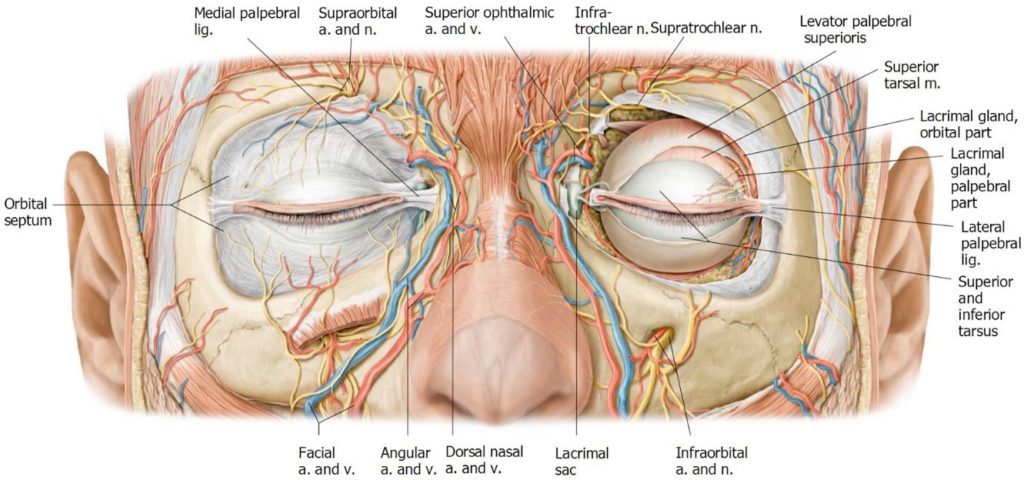
Coursing along the superior margin of the lateral wall of the orbit, above the lateral rectus muscle, see if you can identify the thin, flat lacrimal nerve heading toward the lacrimal gland. See Figure 27.5. The thin, tortuous lacrimal artery travels with the lacrimal nerve.
What are the functions of the frontal and lacrimal nerves?
Which division of the trigeminal nerve gives rise to the frontal and lacrimal nerves?
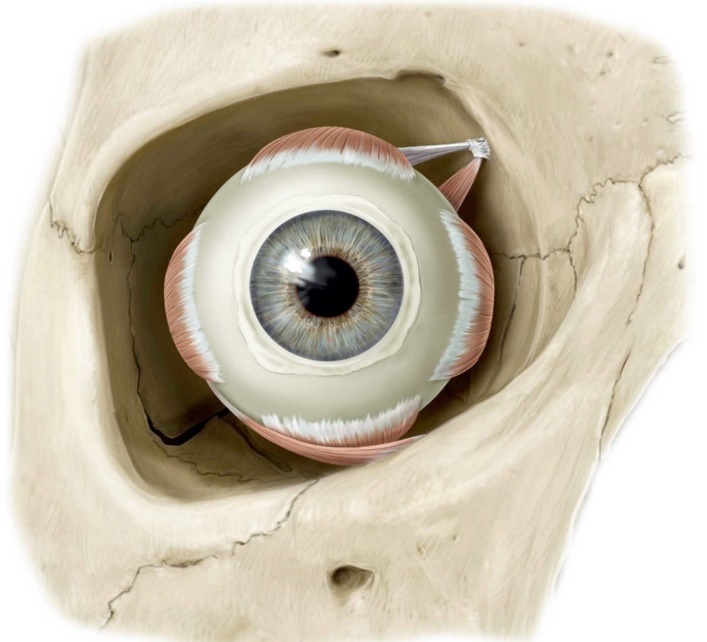
Extraocular Muscles
With forceps, elevate the LPS. Below and parallel to LPS, you will now see the superior rectus muscle.
Along the medial edge of the exposed orbit, locate the fleshy belly of the superior oblique muscle. At the upper medial corner of the orbit, the tendon of the superior oblique suddenly turns medially onto the superior surface of the eyeball. It does so through a pulley made of cartilage called the trochlea (you won’t see this without chipping away bone from the upper medial corner of the orbit).
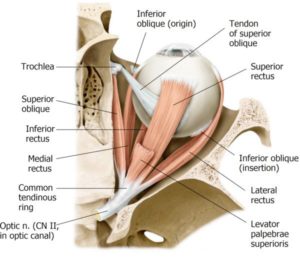
Below and parallel to the superior oblique, locate the medial rectus muscle. Traveling along the lateral wall of the orbit, locate the lateral rectus muscle.
The other two extra-ocular muscles, the inferior rectus and inferior oblique, are on the floor of the orbit and can’t be seen from this view.
The trochlear nerve is very thin and hard to identify in the cranial cavity. In the orbit, it can be identified best as it enters the superior surface of the superior oblique muscle. Probe along the superior border of the muscle and see if you can find the flat, white trochlear nerve penetrating the muscle.
Both sides: Cut and reflect superior muscles and nerves.
Select ONE orbit for concentration on muscles and nerves.
You may be able to identify the thin, white superior division of the oculomotor nerve penetrating the inferior surfaces of the superior rectus and levator palpebrae superioris muscles, after they have been reflected.
Identify the optic nerve in the center of the orbit.
Is the optic nerve really a nerve? In the strictest sense, it is not, since it is an extension of the CNS, and surrounded by all three layers of meninges. Recall that the cell bodies of special sensory neurons within the optic nerves are located in the retinas.
Locate these three structures which cross the superior surface of the optic nerve, and course from lateral to medial in the orbit:
1Ophthalmic artery—tortuous and thin
2Superior ophthalmic vein (large, flat, pale, and collapsed)
3Nasociliary nerve: as it reaches the medial wall of the orbit, it gives off the anterior and posterior ethmoidal nerves. The nasociliary nerve continues into the medial upper eyelid as the infratrochlear nerve.
Clean the lateral rectus muscle. Probe the medial surface of the muscle and locate the abducens nerve entering the muscle. It is white and flat.
Ciliary Nerves, Vessels, and Ganglion
Follow the optic nerve forward to the eyeball and see if you can see some delicate ciliary nerves and vessels coursing with it into the eyeball. Use the magnifying glass!!
Note
If the ophthalmic artery is in the way, it can be removed from this orbit.
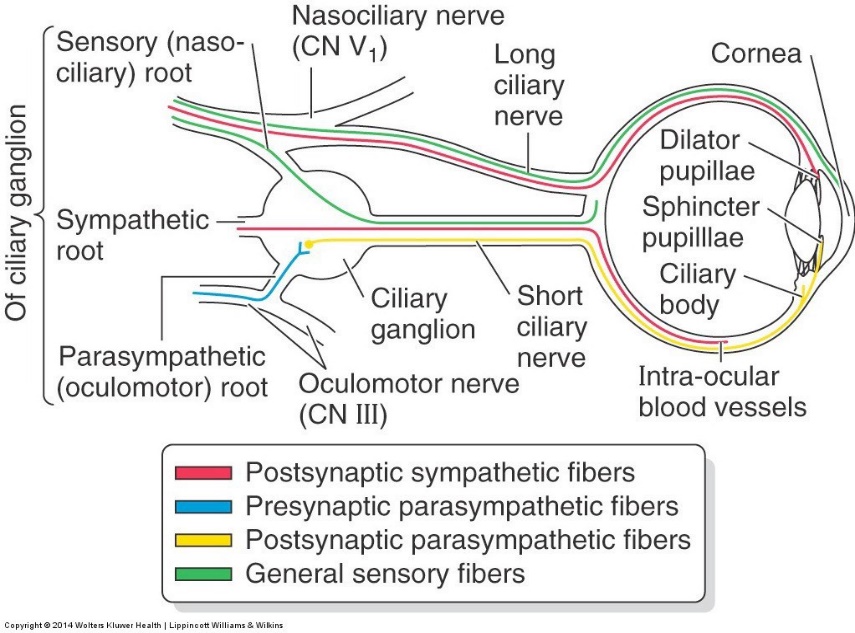
It is very difficult to locate the ciliary ganglion (a parasympathetic ganglion within the orbit) and to distinguish the two ciliary nerves—but you should have a look nonetheless and develop a conceptual understanding of the components within the long and short ciliary nerves.
Following is a rundown:
■Long ciliary nerves [branches of the nasociliary nerve (V1)]: located on the medial side of the optic nerve. They carry:
1Post-Ganglionic sympathetic fibers from the superior cervical ganglion to the eyeball (dilate the pupil) and
2Somatic afferent fibers that transmit general sensation from the eyeball (e.g. = touch and pain from the cornea).
■Short ciliary nerves (branches of the ciliary ganglion): The ganglion is about the size of a pinhead, just lateral to the optic nerve, between it and the lateral rectus muscle. It is connected to the inferior division of the oculomotor nerve. Short ciliary nerves carry:
1Post-Ganglionic sympathetic fibers to the eyeball (dilate the pupil)
2Post-Ganglionic parasympathetic fibers (cell bodies in the ciliary ganglion) to the eyeball (constrict the pupil and cause the lens to “round up”), and
3Somatic afferent fibers from the eyeball that later join the nasociliary nerve.
■The ciliary ganglion is one of the parasympathetic ganglia of the head. It receives preganglionic fibers from the Oculomotor nerve (specifically, the inferior division of CN III).
■Ciliary arteries are small and tortuous and branch from the ophthalmic artery.
Chalk Talk
Sketch (with color-coding) and discuss the nerve fiber types in the long and short ciliary nerves. Consult Figure 27.9.
Side two: Dissect the OTHER orbit with a focus on vessels.
For this side you can remove the frontal nerve, and then completely remove the posterior stumps of the levator palpebrae superioris and superior rectus.
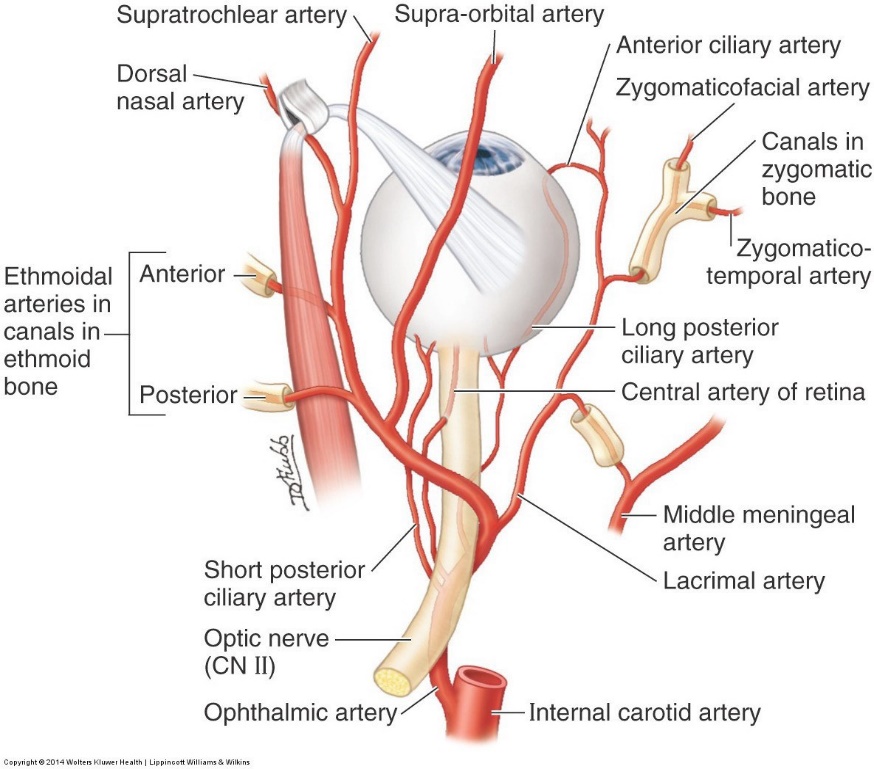
Ophthalmic artery
If you have removed the roof of the optic canal, lift the optic nerve and identify below it the ophthalmic artery branching from the internal carotid artery. Trace the ophthalmic artery (crossing the optic nerve from lateral to medial) forward; clean and locate as many branches as you can.
News Flash!
The optic canal contains two structures: the optic nerve (CN II) and the ophthalmic artery.
You can remove the nasociliary nerve if needed.
The branching pattern of the ophthalmic artery is variable (of course!) but here’s a rundown of the branches in order, from proximal to distal (you should be able to identify the branches with *):
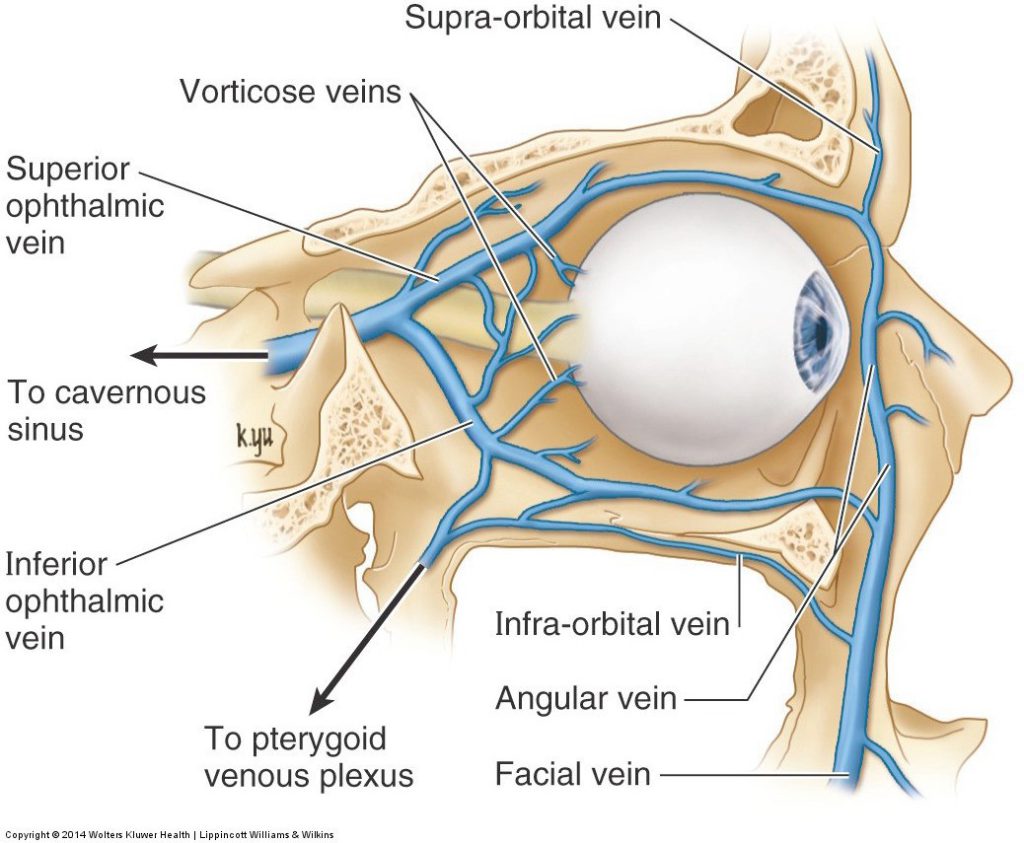
Superior Ophthalmic Vein
It also crosses from lateral to medial, between the superior rectus muscle and optic nerve. You may not recognize it, as it is usually pale in color, collapsed, and somewhat tortuous. See Figure 27.7.
Trace the vein posteriorly and see if you can locate it entering the cavernous sinus.
Clinical correlation
The superior ophthalmic vein is technically an emissary vein since it connects veins outside the skull (e.g. = on the face and forehead) with a venous sinus inside the skull (the cavernous sinus). The vein is valveless, so infections could pass into the skull from the face or scalp through this route.
Anterior Approach to Orbits
Before dissecting—evert (fold) the donor’s upper eyelid away from the eyeball and identify the two parts of the conjunctiva: bulbar (on the sclera of the eyeball) and palpebral (lining the internal surface of the eyelids).
Clinical correlation
The conjunctiva is a clinically important mucous membrane. Infection is called conjunctivitis (“red eye”).
■The two parts of the conjunctiva meet superiorly and inferiorly deep to the eyelids at the superior and inferior conjunctival fornices. Foreign bodies can get into the conjunctival fornices (mud, sand, glass) and contact lenses can get “lost” there too!
■The upper and lower eyelids come together medially near the root of the nose. This “inner corner” is called the medial angle or medial canthus. Lodged between the eyelids, near the medial canthus, note a reddish mound of tissue = the lacrimal caruncle. If you can’t see this on the donor, have a look at your own eyes in the mirror!
The lacrimal caruncle contains modified skin and glandular tissue. What is its function? The “Sandman” knows!
Side 1: Remove the eyelids on ONE side.
On ONE side of the head, use scalpel and scissors to remove the upper and lower eyelids. Probe in the upper lateral part of the exposed orbit to find the lacrimal gland.
Chalk Talk
Sketch and discuss the flow of tears from the lacrimal gland, across the eyeball, and into the lacrimal sac. Where does the nasolacrimal duct drain? Think back to when you studied the respiratory system and see if you can remember the specific area the duct opens into.
Remove fat and connective tissue from around the eyeball.
■Mobilize the eyeball and identify the attachments of the rectus muscles to the eyeball—they attach around the eyeball 90 degrees apart.
This anterior view is best for visualizing the inferior oblique muscle. Note its attachment to the floor of the orbit. Lift the eyeball and find the inferior rectus muscle. How is it related to the inferior oblique?
Can you see the inferior division of the Oculomotor nerve passing forward in the floor of the orbit? It innervates the inferior oblique and inferior rectus, as well as the medial rectus.
Side 2: On the OTHER side, with the eyelids intact, dissect the upper eyelid.
Carefully remove the thin skin from the upper eyelid with a SHARP scalpel to reveal the palpebral part of the orbicularis oculi muscle. The orbicularis oculi also have a large orbital part that encircles each orbit. The superficial fascia of the eyelids has a thin layer of loose connective tissue with no fat.
Tarsal plates are dense connective tissue in which tarsal glands are embedded. Tarsal plates give shape and strength to the eyelids. The tarsal plate is largest in the upper eyelid. The tendon of the levator palpebrae superioris muscle inserts into the superior border of the tarsal plate in the upper eyelid. With scissor or a sharp scalpel, remove the thin palpebral part of the orbicularis oculi to find the superior tarsal plate.
Tarsal glands are arranged vertically in rows within the tarsal plates. Their ducts open along the margins of the eyelids near the eyelashes. Tarsal glands make an oily substance that
1waterproofs the edges of the eyelids to prevent tears from seeping onto the face, and
2is mixed with tears to prevent their rapid evaporation.
Summary: the layers of the eyelids from superficial to deep:
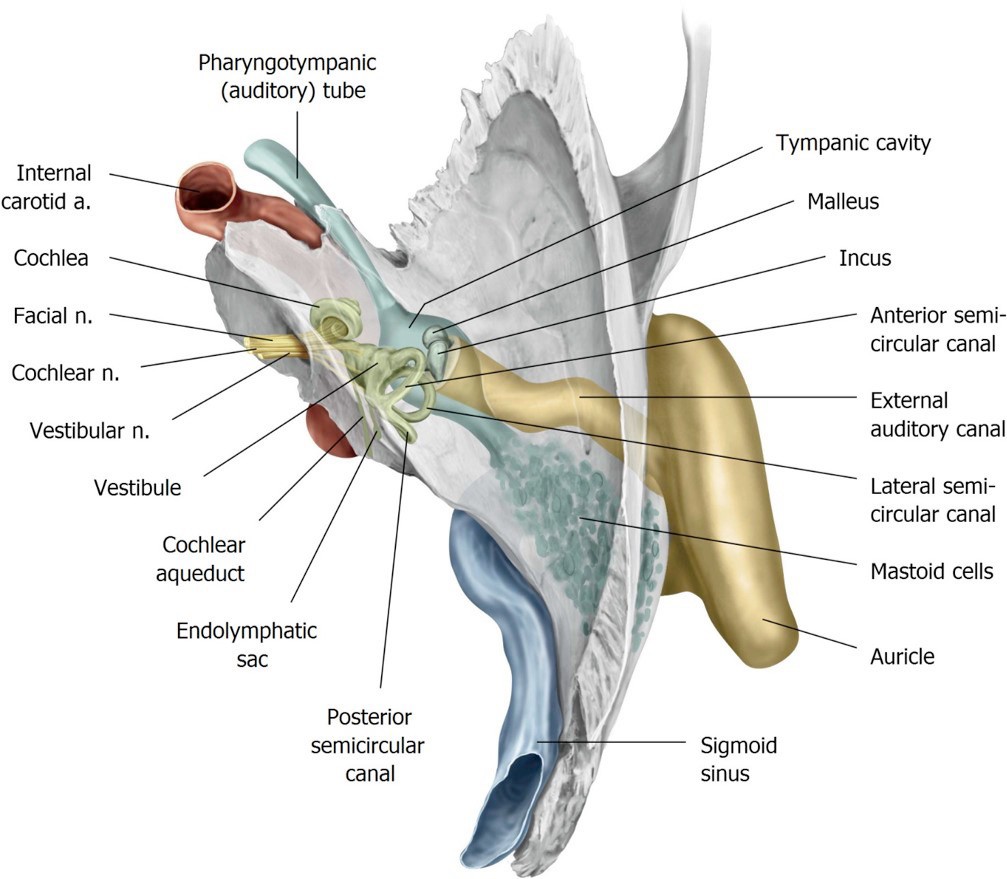
The Ear
In gross anatomy we will focus on the external and middle portions of the ear.
SKULL REVIEW: Grab a skull and locate the following bony parts:
■Temporal bone: squamous, tympanic and petrous parts
■External acoustic meatus
■Internal acoustic meatus
■Stylomastoid foramen
■Mastoid process of temporal bone
■Foramen lacerum
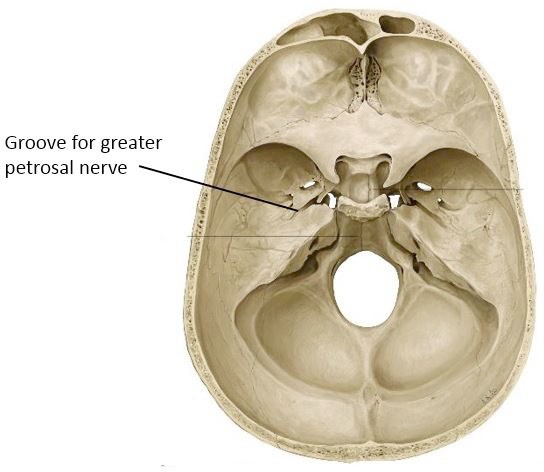
■Groove for the greater petrosal nerve (a crack in the bone, extending from the petrous temporal bone to the foramen lacerum)
External Ear
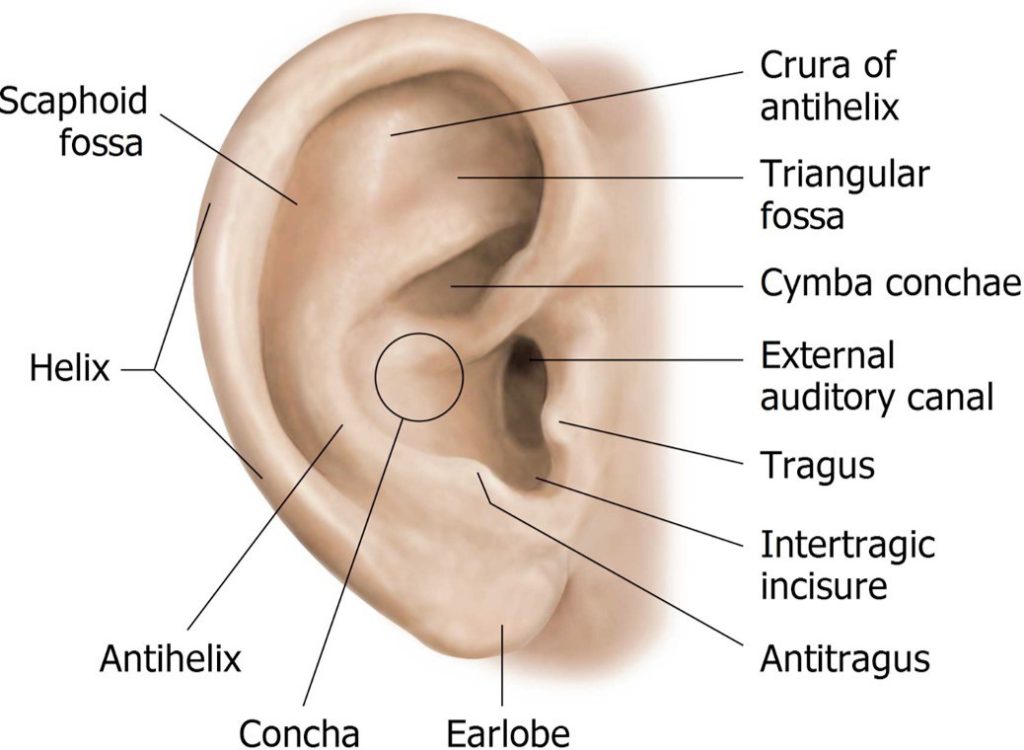
Examine the auricle (aka = pinna) and name its parts.
Middle Ear
Study a Model of the Tympanic Cavity
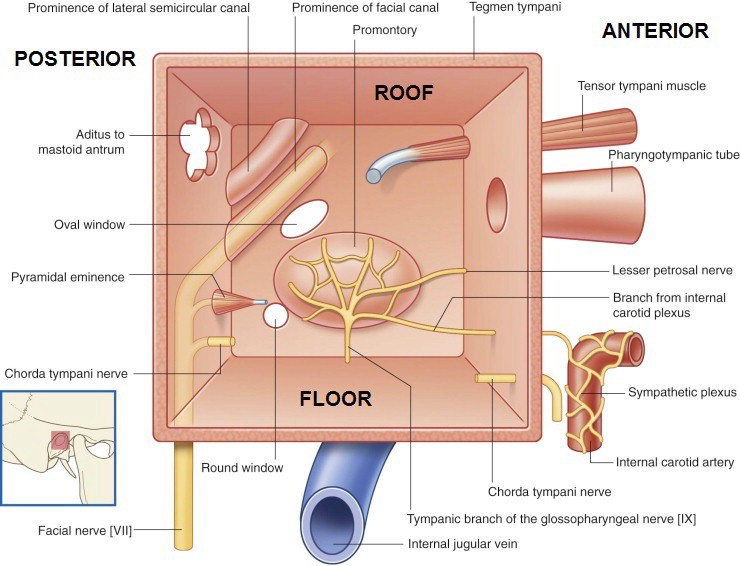
Review the bony walls of the tympanic cavity (and their relationships to nearby structures) using the “BOX” visual analogy.
The walls of the tympanic cavity are made of thin plates of bone.
■Roof: The bony roof is called the Tegmen tympani—separates the tympanic cavity from the middle cranial fossa above.
■Floor: The internal jugular vein is below the bony floor.
■Lateral Wall: The tympanic membrane separates the tympanic cavity from the external acoustic meatus.
■Medial Wall: Separates the tympanic cavity from the internal ear. There are two openings on the medial wall:
■Oval window (closed by the footplate of the stapes)
■Round window (closed by the secondary tympanic membrane)
■Posterior wall: The aditus is an opening on the posterior wall that leads into the mastoid antrum. From the mastoid antrum, many tiny membrane-lined mastoid air cells sprout.
■Anterior wall: Separates the tympanic cavity from the carotid canal containing the internalcarotid artery. The pharyngotympanic (Eustachian) tube opens on the anterior wall of the tympanic cavity.
Where does the other end of the Eustachian tube open?
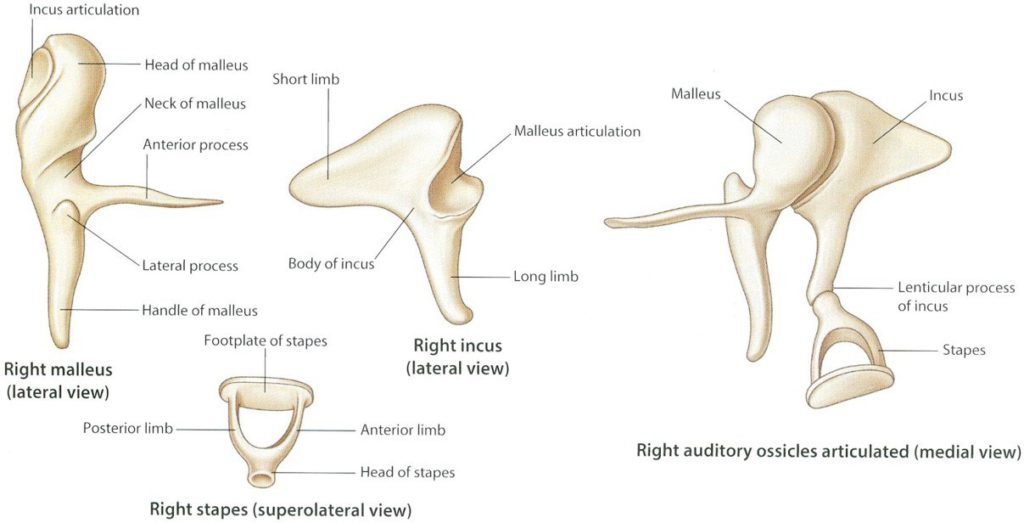
Study a Model of the Auditory Ossicles
Note that the ossicles form a chain across the tympanic cavity, from the tympanic membrane (lateral) to the oval window (medial). The head of the malleus and body of the incus extend up into the epitympanic recess = the part of the tympanic cavity above the tympanic membrane (kind of the like a vaulted ceiling in your Living Room).
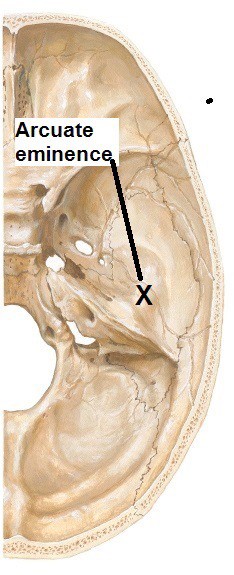
Side one: Open the roof of the tympanic cavity.
Do this on ONE side of the head.
Strip away the dura from one side of the middle cranial fossa
Locate the arcuate eminence—a slight bulge in the floor of the fossa, antero-lateral to the petrous ridge of the temporal bone.
Use a hammer and chisel to fracture the tegmen tympani (roof of tympanic cavity) just anterior to the arcuate eminence. Use bone rongeurs or forceps to remove the tegmen tympani piecemeal. This takes skill and a little luck but should allow you to open the roof of the tympanic cavity. Use a magnifying glass to take a peek inside.
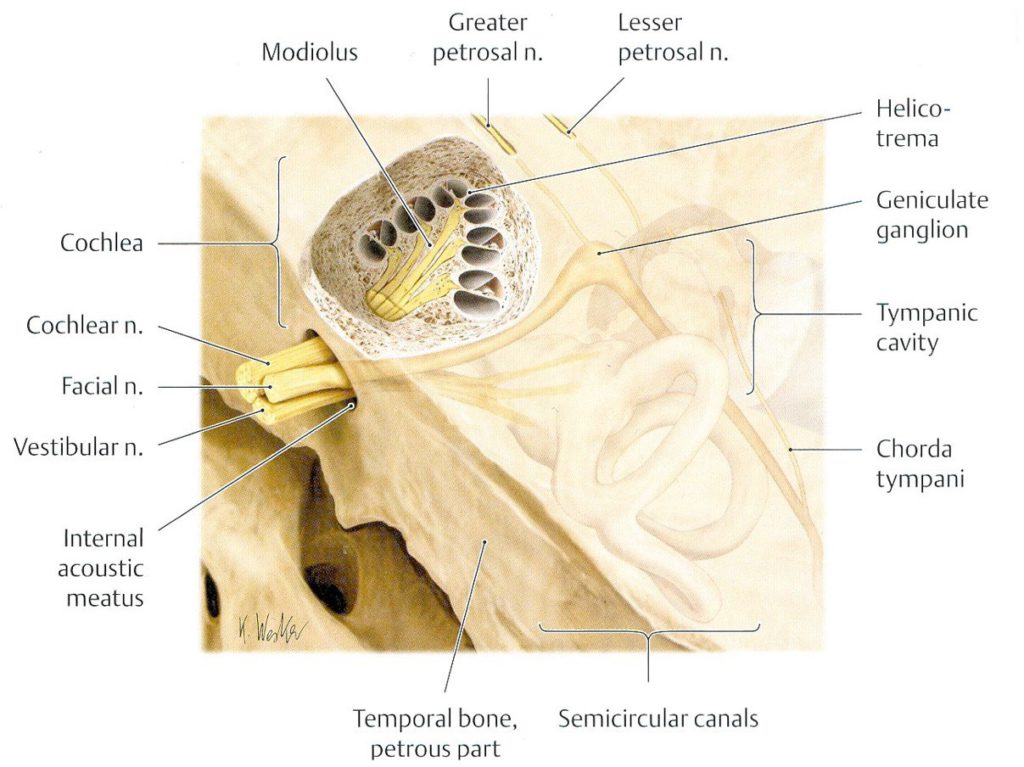
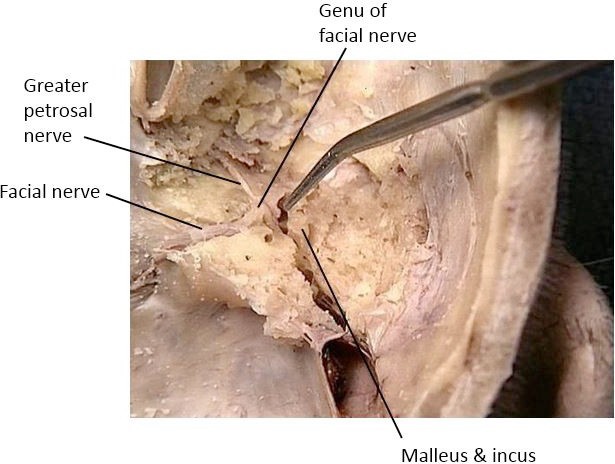
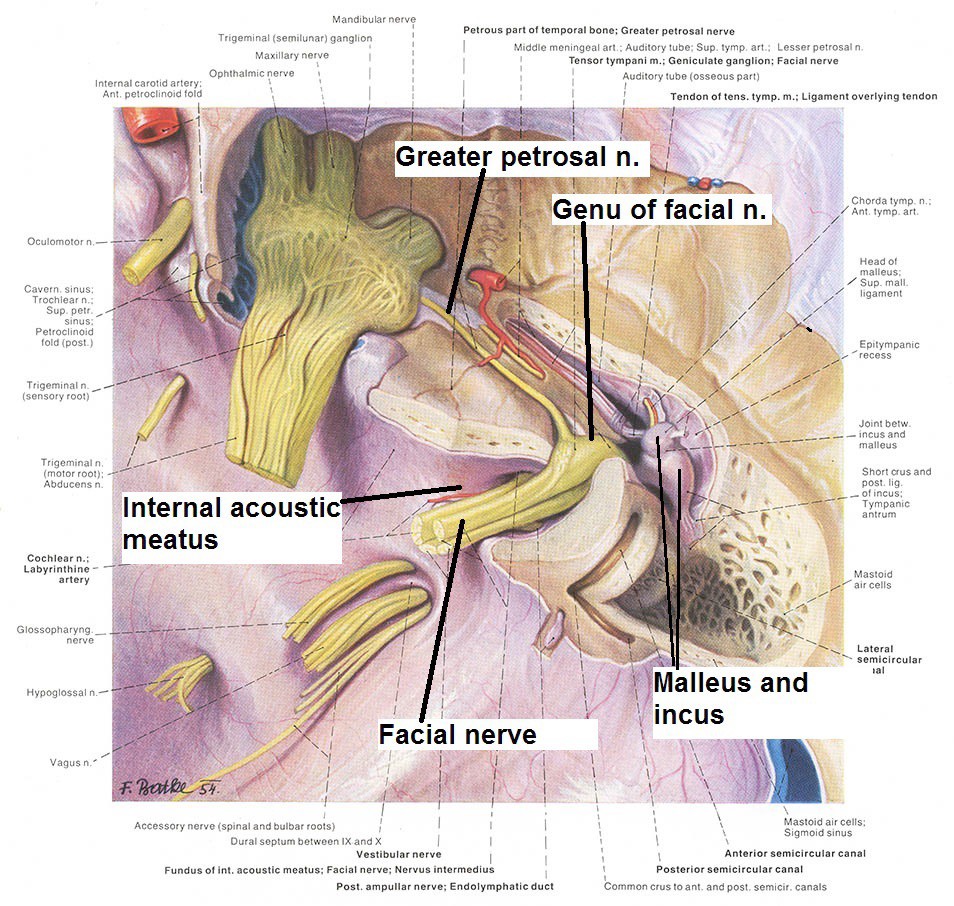
Now that the tympanic cavity and facial canal are open, identify the following with the help of a magnifying glass and pen light.
■Facial nerve—after passing through the internal acoustic meatus it enters the facial canal and heads laterally, Before reaching the tympanic cavity it bends sharply posteriorly, making an almost 90 degree turn. This is the genu of the facial nerve and is the location of the geniculate ganglion (the sensory ganglion of the facial nerve)
■Greater petrosal nerve leaving the facial nerve at the genu. It moves anteriorly to enter the floor of the middle cranial fossa. What is the function of the greater petrosal nerve (what nerve fiber types does it carry)? Consult the “Conley-gram” drawing of the facial nerve for review.
■You will also see the vestibulocochlear nerve entering the internal acoustic meatus.
Be sure to take a stroll around the lab to look at other teams’ work.
Opening the tympanic cavity and facial canal is very difficult,
and it takes a little bit of luck.
Don’t be discouraged!
Checklist, Lab #27
Review and make sure you have identified each of the structures below.
Review the bony anatomy of orbit and foramina associated with orbital walls—structures listed earlier.
Review the bony anatomy associated with the middle ear—structures listed earlier.
Review your dissection and make sure you have identified each of the structures in the checklists that follow.
Muscles
Superior, inferior, medial, and lateral rectus muscles
Superior and inferior oblique muscles
Levator palpebrae superioris muscle
Orbicularis oculi muscle—a muscle of facial expression
Nerves
Optic
Oculomotor (superior and inferior divisions are wish list items)
Trochlear
Ophthalmic (V1)
Lacrimal
Frontal
Supra-orbital and supratrochlear
Nasociliary
Abducens
Vessels
Ophthalmic artery
Lacrimal artery
Supra-orbital artery
Superior ophthalmic vein
Other
Ciliary ganglion (wish list item—you are a superstar if you can locate it)
Eyelids
Bulbar and palpebral parts of conjunctiva
Superior/inferior conjunctival fornices
Lacrimal gland
Tarsal plate (upper eyelid)
Lacrimal apparatus: on the model
Lacrimal puncta
Lacrimal canaliculi
Lacrimal sac
Nasolacrimal duct
External Ear
Auricle
Helix and antihelix
Concha
Tragus
Lobule
External acoustic meatus
Tympanic membrane
Middle ear dissection
Malleus and incus
Facial nerve in facial canal
Genu of VII (location of Geniculate ganglion)
Greater petrosal nerve (wish list item—get a for the day by finding this gem of a nerve)
On ear models
Tegmen tympani
Promontory
Oval window and round window
Mastoid air cells
Eustachian (Pharyngotympanic) tube
Tympanic membrane
Auditory ossicles
Malleus: Head and handle
Incus: Head, short and long processes
Stapes: Head, crura, and base (footplate)