1Identify the parts of the small and large intestines.
2Dissect the superior and inferior mesenteric arteries and their branches.
3Identify the hepatic portal vein and its major tributaries.
4Open the jejunum, ileum, and cecum to view their internal features.
Before you cut: Review the parts of the Small and Large Intestines
Which parts of the small and large intestines are retroperitoneal? Which parts are intraperitoneal (suspended by a mesentery)?
Mesenteries:
■The first part of the duodenum is supported by the lesser omentum (specifically, by the hepatoduodenal ligament).
■The jejunum and ileum are supported by the mesentery (to avoid ambiguity, it is best to refer to this as the mesentery of the small intestine).
■The transverse colon is supported by the transverse mesocolon.
■The sigmoid colon is supported by the sigmoid mesocolon.
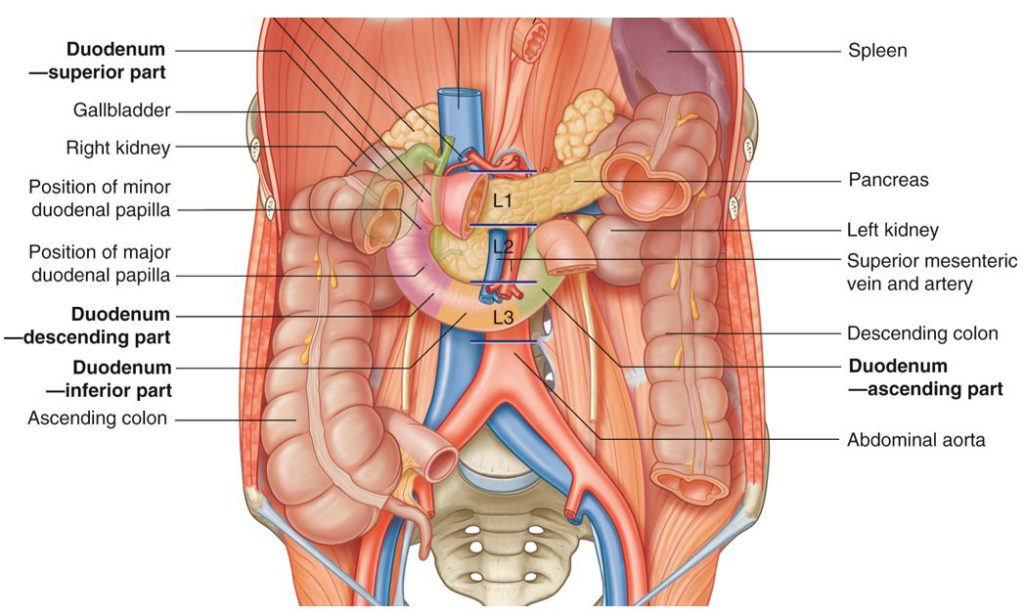
Review the anatomy of the pancreas and duodenum:
■The pancreas has a head, body, tail, and uncinate process.
■The duodenum is the first part of the small intestine. It has four parts (Figure 24.1):
■Part one (superior part)
■Part two (descending part)
■Part three (horizontal or inferior part)
■Part four (ascending part)
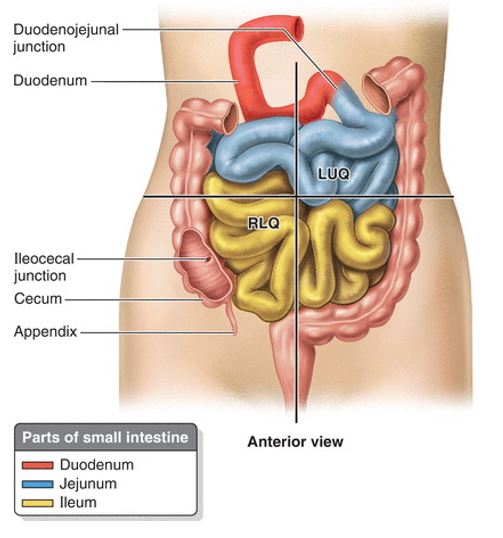
Push the loops of the small intestine to the right and find the duodenojejunal junction. From here, walk down the small and large intestine and name all the parts until you reach the rectum in the pelvic cavity.
■Jejunum and Ileum
■Ileocecal junction
■Cecum
■Appendix – has a base attached to the cecum, and a tip (variable location)
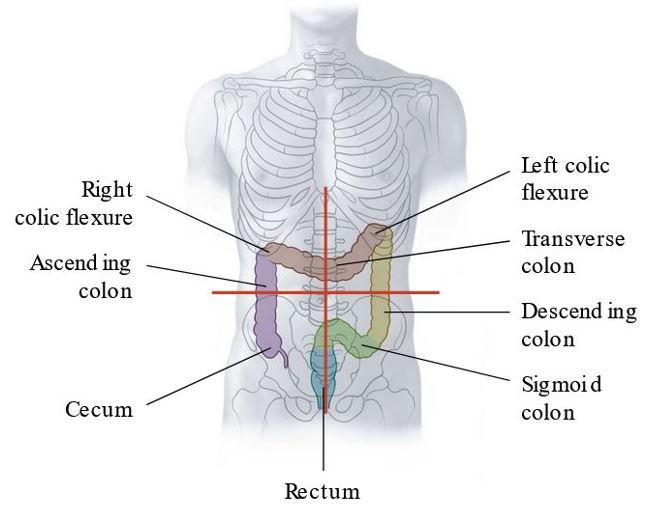
■Ascending colon
■Right colic (hepatic) flexure
■Transverse colon
■Left colic (splenic) flexure
■Descending colon
■Sigmoid colon
■Rectum
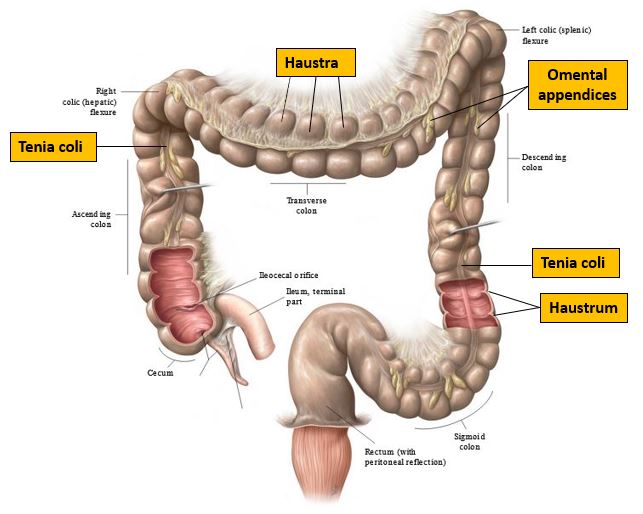
On the colon, identify:
■Omental appendices (fat globs – function unknown, possibly cushioning of the colon, fat storage, defense against infection?)
■Teniae coli: 3 ribbons containing the colon’s longitudinal smooth muscle, arranged 120 degrees apart. Proximally, they converge on the base of the appendix. Distally, they end at the recto-sigmoid junction.
■Haustra: Sacculations of the colon. They are formed by the tug of the teniae coli on the colon, like a draw string around the waist of your baggy sweatpants.
Does your donor have an appendix?
It’s a blind “worm-like” diverticulum of the cecum, usually 6–10 cm in length. What are its functions thought to be?
Where did you locate the TIP of the appendix? Most often it is found in the retrocecal recess of the peritoneal cavity. The BASE of the appendix attaches to the cecum in a predictable location on the posteromedial side just below the ileocecal junction, where the teniae coli converge.
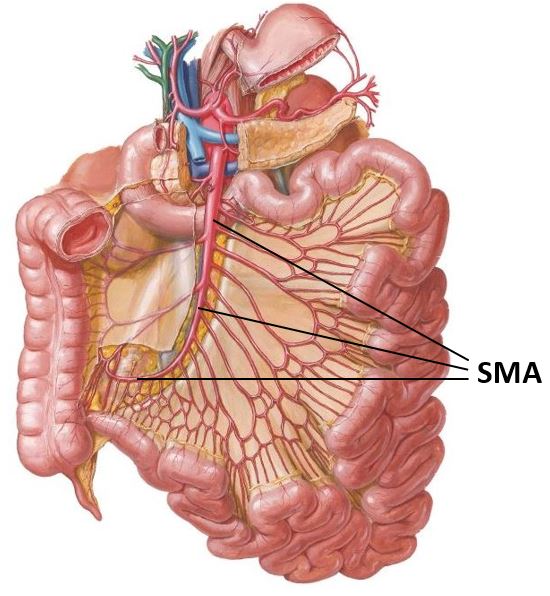
Superior Mesenteric Artery (SMA)
Note
The superior mesenteric artery supplies organs of the midgut.
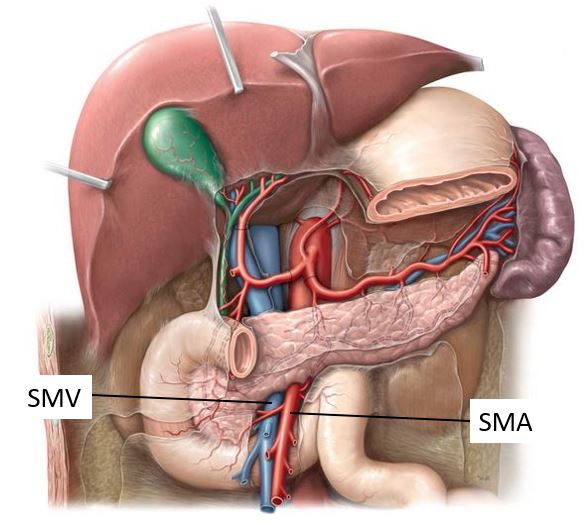
Relationships of the SMA (see Figure 24.6):
■Originates from the abdominal aorta @ L-1
■Passes behind the neck of the pancreas
■Passes anterior to the uncinate process of the pancreas and the horizontal (3rd) part of the duodenum
■Descends to the right side of the abdomen – toward the cecum.
■The superior mesenteric vein is directly to the right of the artery.
Dissect the SMA and its branches.
1Turn the transverse colon and transverse mesocolon upward, as shown in Figure 24.7.
2Strip away the peritoneum to the right of the duodenojejunal junction and inferior to the pancreas.
3Locate the SMA, and to its right, the superior mesenteric vein (SMV), as they cross the uncinate process of the pancreas and third part of the duodenum. You will have to cut away a thick network of autonomic nerves.
4Elevate the pancreas. Clean and follow the SMA proximally to the point where it arises from the abdominal aorta.
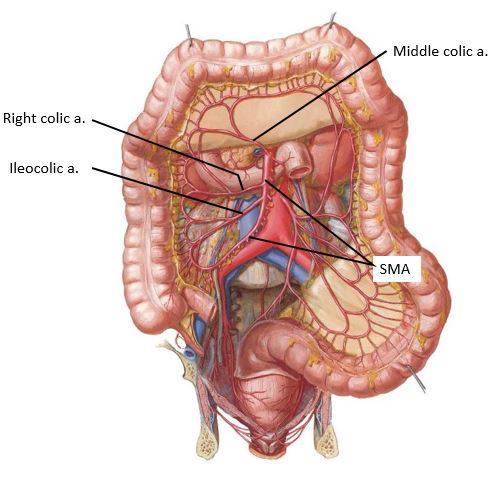
5Identify branches of the SMA:
■Push the loops of the small intestine to the left side of the abdomen.
■Strip away the posterior layer of the transverse mesocolon and identify the middle colic artery. Trace it down to where it joins the SMA. See Figure 24.7.
■Follow the SMA distally – identify the right colic artery: it passes behind the peritoneum to the right, toward the ascending colon.
■Just above the ileocecal junction, remove the peritoneum from the posterior abdominal wall and clean the medial surface of the cecum and proximal part of the ascending colon. Identify the ileocolic artery and trace it to the SMA.
Note
Variations in the branching patterns of colic arteries are common.
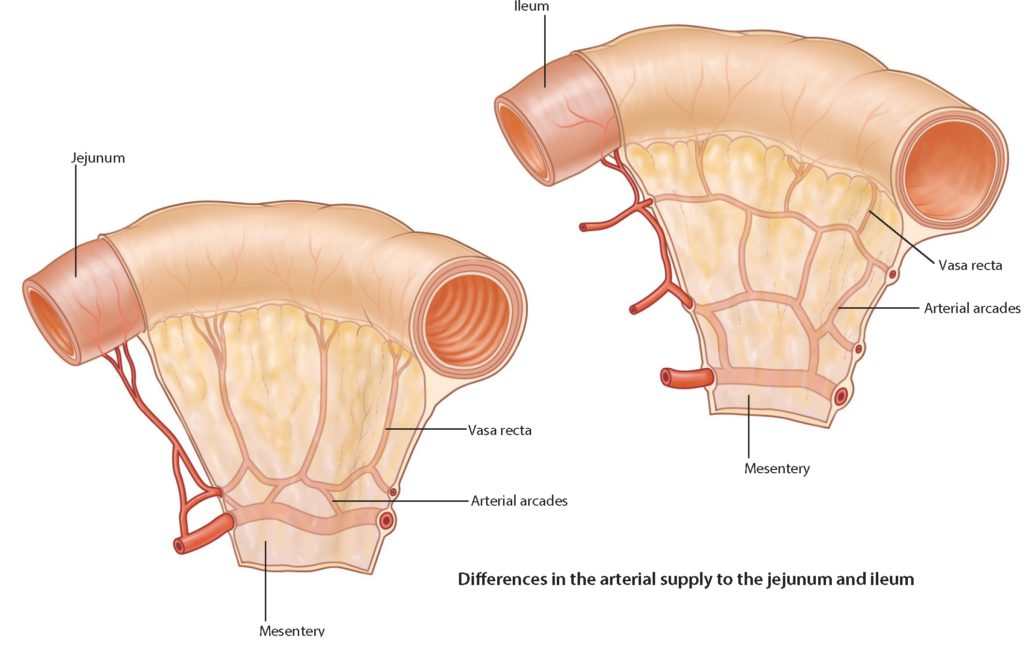
■Strip away the peritoneum from the right side of the mesentery of the small intestine, just distal to the duodenojejunal junction, and clean off some jejunal arteries.
■Follow the jejunal arteries distally and note how they form arcades (arches or loops) that anastomose with neighboring arteries.
■Clean off a few straight arteries (vasa recta) as they branch from the arcades and pass toward the wall of the jejunum.
■Locate a portion of the ileum proximal to the ileocecal junction. Strip away peritoneum and do the same drill: locate a couple ileal arteries and follow them toward the ileum until they form arcades and give off straight arteries.
■Compare the architectures of the intestinal arcades and straight arteries in the two regions. Notice any differences? See Figure 24.8.
Note
After examining Figure 24.8, you will note that the intestinal arcades are simpler (single-tiered) in the jejunum, whereas the arcades are more complex, having more tiers in the ileum. As a result, the straight arteries are longer in the jejunum than they are in the ileum. Anatomy is a beautiful thing!
6The intestinal arteries (jejunal + ileal arteries) branch from the left side of the main trunk of the SMA as it passes along the base of the mesentery.
Note
Note that the main trunk of the SMA (the part that gives off the intestinal branches) connects distally with the ileocolic artery near the cecum (see Figure 24.9) = a rare case where a main artery and one of its branches anastomose. Wild!
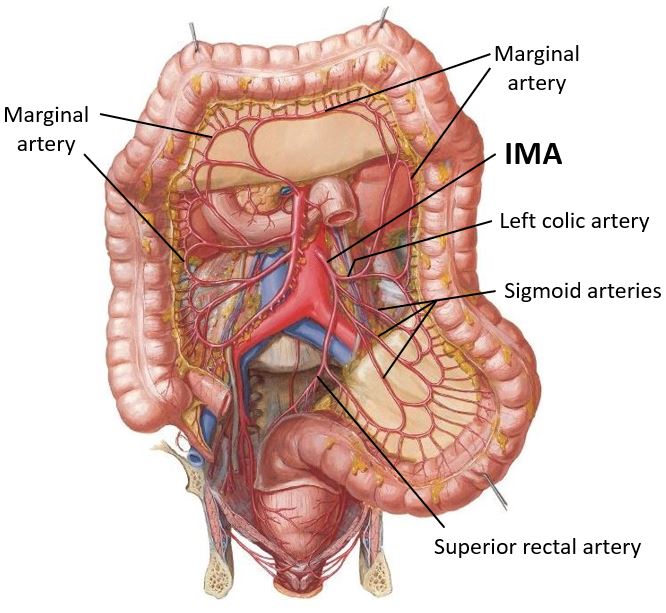
Inferior Mesenteric Artery (IMA)
Push the loops of the small intestine to the right side of the abdomen. The IMA supplies organs of the hindgut.
1Below the 3rd (horizontal) part of the duodenum, palpate the abdominal aorta through the peritoneum of the posterior abdominal wall.
Note
The aorta may be rock hard due to plaques in its wall and blood clots clogging its lumen.
Dissect the IMA and its branches.
2Remove the peritoneum over the aorta with forceps and scissors down to the bifurcation of the aorta (level of L-4) into common iliac arteries. Clean away the autonomic nerves on the aorta’s surface.
3Locate the inferior mesenteric artery (IMA). It’s not nearly as large as the SMA and it is often flattened against the anterior wall of the aorta – so, look carefully! The IMA arises from the aorta @ L-3. It passes to the left side of the body.
4Clean the IMA distally and identify the following branches (Figure 24.10):
■Left colic artery (to descending colon)
■Sigmoid arteries (to sigmoid colon)
■Superior rectal artery (The main trunk of the IMA continues inferiorly into the pelvic cavity. After crossing the pelvic brim, the IMA becomes the superior rectal artery.)
Marginal Artery (of Drummond)
■Clean along the inner border of the large intestine “box”, from cecum to sigmoid colon.
■Note the interconnected series of arteries forming a continuous source of blood to the colon. As each colic artery reaches the inner border of the colon it splits into two branches: one proceeding proximally and the other distally, to join with branches of the adjacent colic arteries.
■This arterial anastomosis, from cecum to sigmoid, is the Marginal artery (artery of Drummond). See Figure 24.10.
Can you name all the arteries that contribute to the marginal artery? What is the significance of the marginal artery?
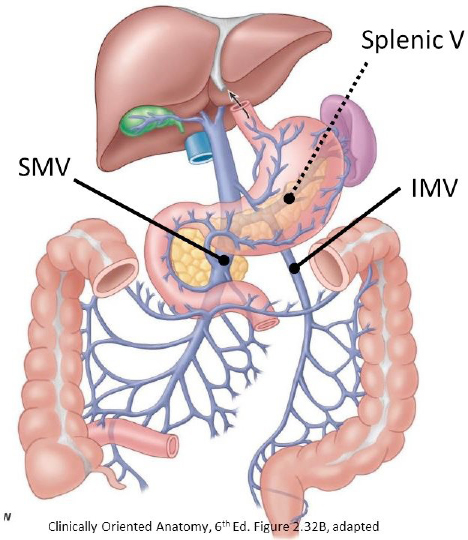
Portal System of Veins
1Pry the pancreas loose from the body wall. Find the splenic vein posterior to the pancreas and follow it as it passes to the right.
2Clean the superior mesenteric vein (SMV) adjacent to the SMA.
3Find and clean the inferior mesenteric vein (IMV). It ascends behind the peritoneum on the posterior abdominal wall, parallel to and on the medial side of the descending colon. Trace it superiorly—it typically joins the splenic vein.
4Trace the splenic and superior mesenteric veins until they join to form the hepatic portal vein behind the pancreas. [You may have only a stump of the portal vein if you removed the liver from your donor.]
5The SMV and IMV drain organs of the midgut and hindgut, respectively. Venous drainage from parts of the foregut is through veins that drain directly into the portal vein.
Where is the celiac vein? (This may be a trick question!)
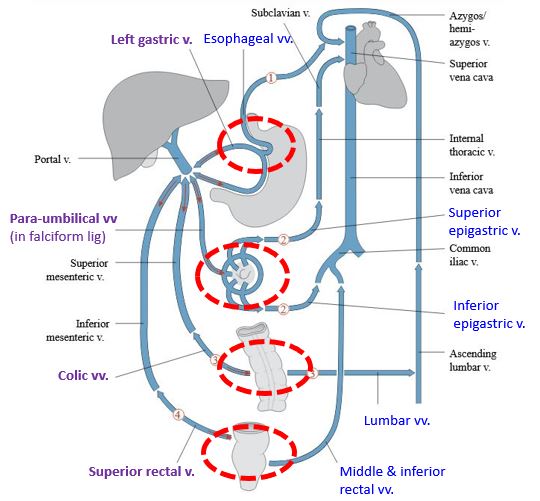
Note
Here is a good opportunity to discuss the concept of porto-systemic anastomoses. These occur in organs where there are venous plexuses that connect to veins of both the portal system and systemic (caval) circulation (Figure 24.12). In the case of portal hypertension, these venous plexuses can swell, producing varices. Where are these anastomoses located and what is their clinical importance?
Open parts of the intestines and inspect their internal anatomy.
Let’s have a look inside a few of these organs.
■Using a scalpel or scissors, make 3- to 4-inch-long incisions in both the proximal jejunum and distal ileum. Clean out any contents of the organs.
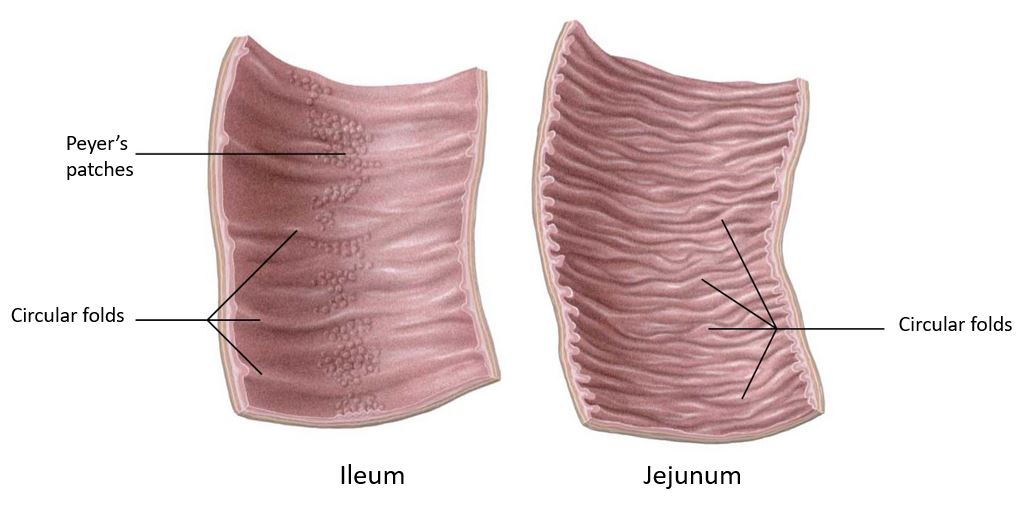
■Identify the internal folds of mucosa in these regions, the circular folds (plicae circulares). These are permanent structures (unlike rugae in the stomach) that increase the absorptive surface area of the small intestine. Note that as you move from jejunum to ileum the plicae circulares decrease in size and number.
■You may be able to see small ovoid lumps in the mucosa of the ileum. These are lymphoid nodules (Peyer’s patches), large accumulations of lymphoid tissue, present only in the terminal region of the ileum (Figure 24.13).
■If it’s not too full of fecal material, open the cecum near the ileocecal junction and clean it out with paper towels. Find the ileal orifice and, if possible, the orifice of the appendix. The appendix is a hollow lymphoid organ. Its lumen is a blind diverticulum that communicates proximally with the cavity of the cecum.
■If you haven’t already done so, open the stomach and identify the gastric folds (rugae) and open the 2nd (descending) part of the duodenum and identify the major duodenal papilla, where the hepatopancreatic ampulla (ampulla of Vater) opens. The ampulla is the common chamber where the distal parts of the common bile duct and main pancreatic duct meet.
Checklist, Lab #24
Review and make sure you have identified each of the structures below.
Mesentery of small intestine
Transverse mesocolon
Sigmoid mesocolon
Duodeno-jejunal flexure
Jejunum and Ileum
Ileocecal junction
Cecum
Appendix
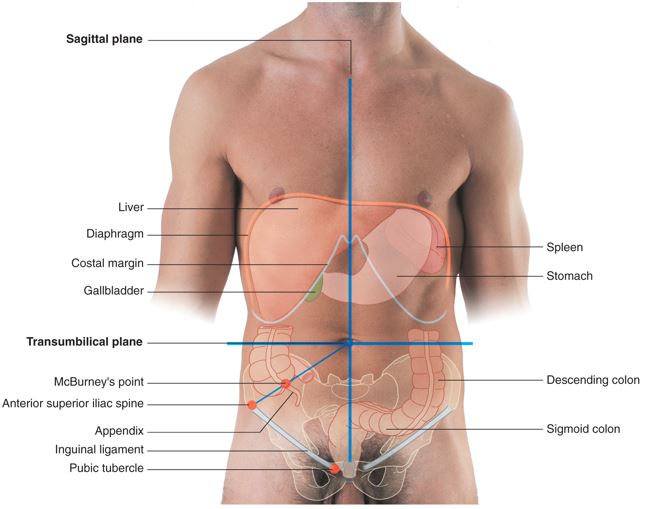
The location of McBurney’s point (on the surface of the abdominal wall)
Ascending, transverse, and descending colon
Right and left colic flexures (aka = hepatic and splenic flexures)
Rectum
Circular folds (plicae circulares) = in duodenum and jejunum
Gastric folds (rugae)—inside the stomach
Major duodenal papilla (in duodenum)
(Common) Bile duct
Main pancreatic duct—you are a superstar if you can find it!
Haustra of colon, omental appendices, and teniae coli
Superior mesenteric artery
Jejunal and ileal arteries
Arterial arcades (associated with jejunal and ileal arteries)
Ileocolic artery
Right colic artery
Middle colic artery
Inferior mesenteric artery
Left colic artery
Sigmoidal arteries
Superior rectal artery
Marginal artery (of Drummond)
Superior mesenteric vein
Splenic vein
Inferior mesenteric vein
Hepatic portal vein