1Survey the GI organs.
2Examine the peritoneum, peritoneal cavity, mesenteries, omenta, and peritoneal ligaments.
3Locate the subparts of the greater sac.
4Study the lesser omentum and demonstrate the lesser sac.
5Dissect the celiac trunk and demonstrate its branches.
6Clean and study the organs in the supracolic region: liver; gallbladder and biliary tracts; stomach; duodenum; pancreas; and spleen.
7Demonstrate the structures that make up the portal triad.
8Remove the liver and examine its features.
Anterior Abdominal Wall
The anterior abdominal wall has been opened for you (thank you, first-year students!)
Inspect the internal aspect of the inferior abdominal wall.
Complete anatomy
Posterior Surface of Anterior Abdominal Wall
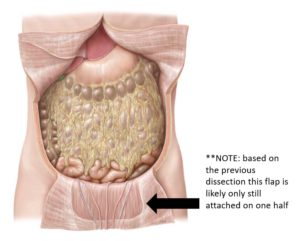
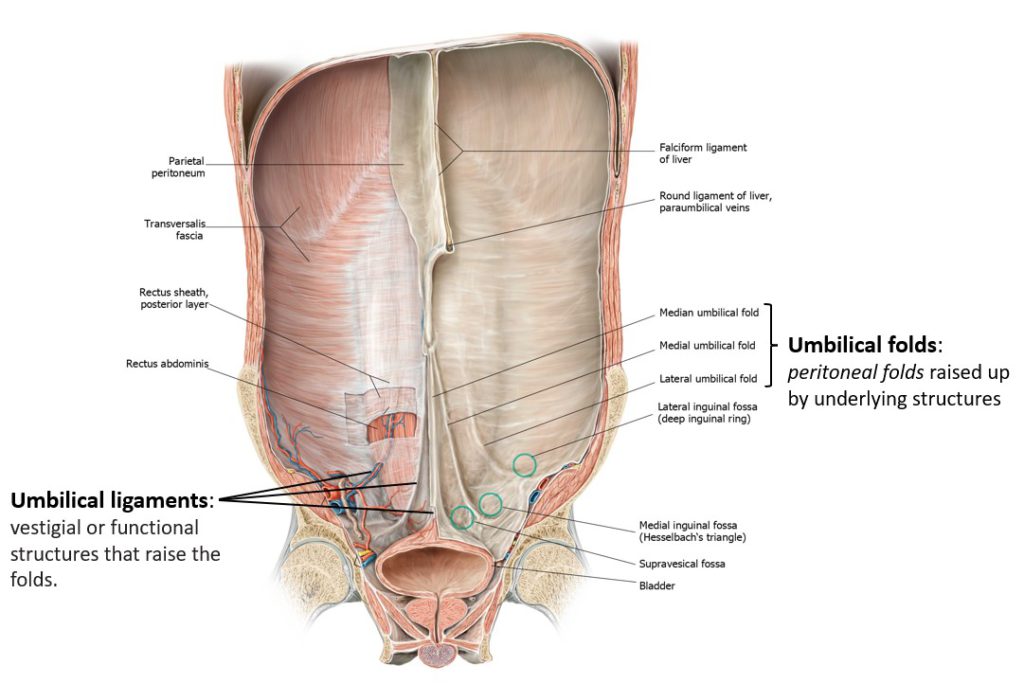
If there is a portion of the inferior abdominal wall intact, inspect the portion beneath the umbilicus to identify the umbilical folds and umbilical ligaments.
Identify:
Median umbilical folds contain the median umbilical ligament (urachus). This is a fibrous vestige of bladder development. Look for this descending down from the umbilicus along the midline.
Medial umbilical folds (left and right) contain the medial umbilical ligaments. These are the obliterated fetal umbilical arteries.
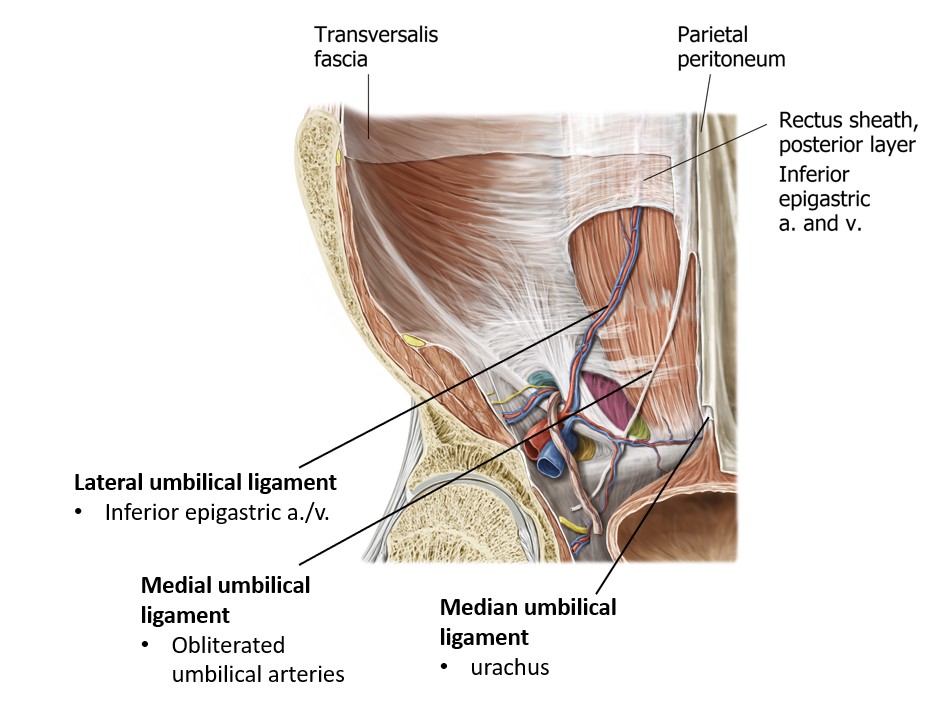
Lateral umbilical folds are more subtle, inconspicuous folds of peritoneum. They contain the inferior epigastric vessels.
Clinical correlation
Can you recall the role of the inferior epigastric vessels in determing direct vs. indirect inguinal hernias? Identify the borders of the inguinal (Hesselbach’s) triangle from this internal surface.
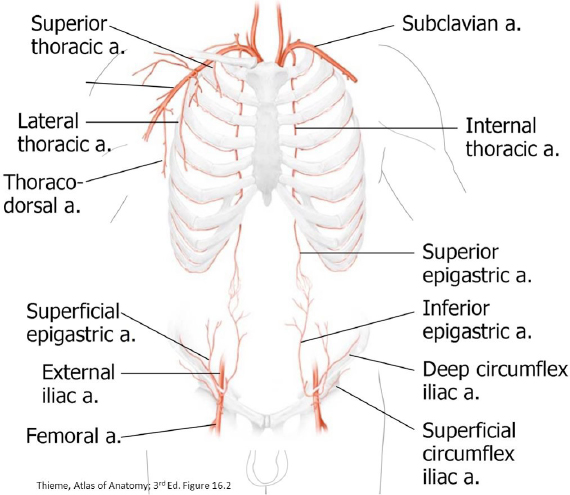
On each side, the inferior epigastric vessels pass under the arcuate line to enter the rectus sheath, posterior to the rectus abdominis muscles. Within the rectus sheath, the inferior epigastric artery supplies the rectus muscle and anastomoses with the superior epigastric artery, a terminal branch of the internal thoracic artery.
This anastomosis could provide an alternate route for blood to reach the lower limb should the descending aorta be compromised.
Clinical correlation
Discuss this alternate route with your group. Draw a flowchart.
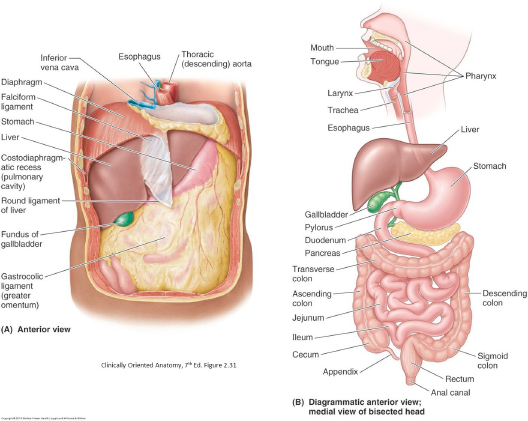
Overview of Abdominal Viscera
Explore and name the organs of the abdominal cavity.
Complete anatomy
Abdominal Viscera
Liver
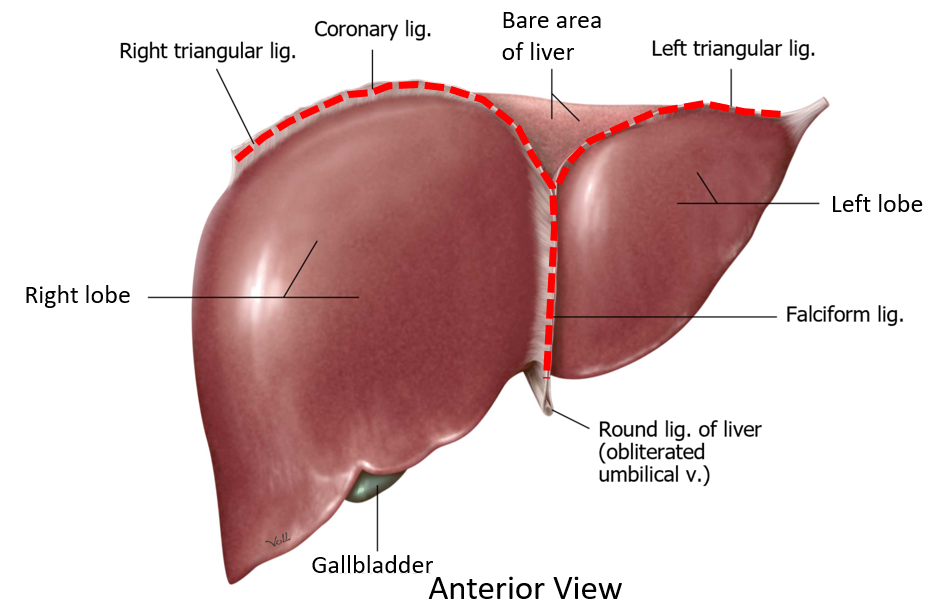
The sharp inferior border peeks out under the costal margin; reach under the diaphragm to feel the liver’s diaphragmatic surface. Identify the right and left lobes of the liver – covered in visceral peritoneum
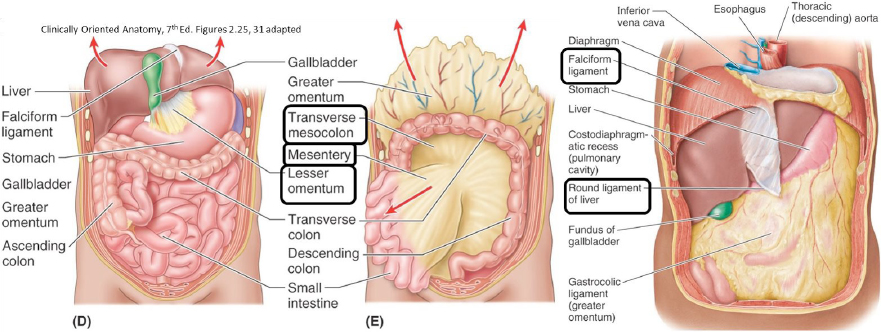
Examine the sickle-shaped falciform ligament running between the lobes. This double layer of peritoneum connects the liver to the anterior abdominal wall (its attachment to the anterior wall has likely been cut). Palpate the arched inferior free margin of the ligament. The cord-like structure within the inferior margin of the ligament is the round ligament of the liver (remnant of the fetal umbilical vein).
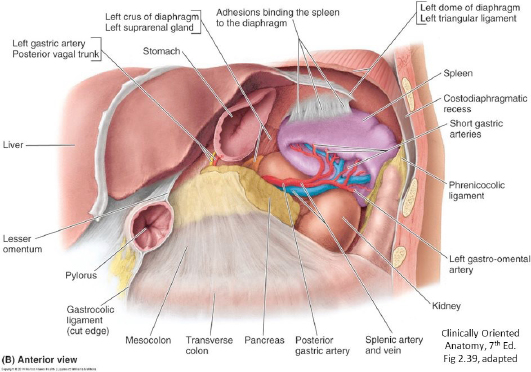
Elevate the liver to find the abdominal esophagus and the stomach. With your right hand, reach across the cadaver to the left side behind to stomach and under the diaphragm to find the spleen.
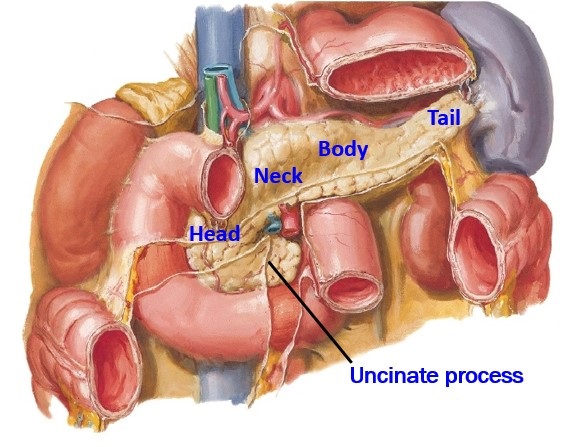
The pancreas is hidden deep to the stomach. It is covered by peritoneum (it is retroperitoneal) so it may be difficult to identify initially.
Small Intestine
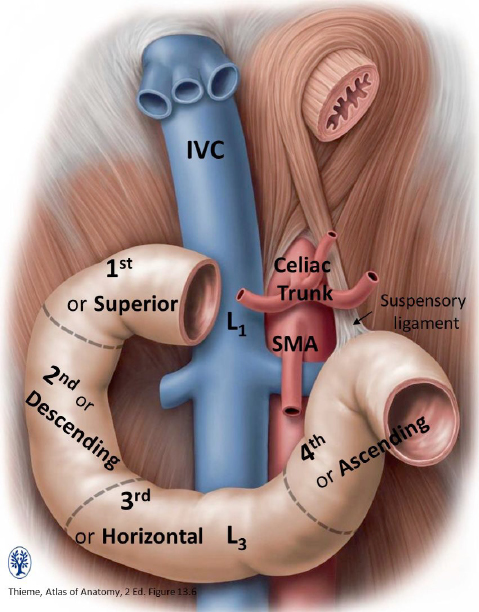
Trace the stomach to the right to find the duodenum. Only the first part of the duodenum is visible (intraperitoneal)—you won’t see parts 2, 3, and 4 yet because they are retroperitoneal. It is curved and shaped like the letter C. The concavity of the curve faces to the left. Distal to the duodenum are the other parts of the small intestine: jejunum and ileum. Push the small intestine to the right to find the duodenojejunal junction. Trace the ileum to the right lower quadrant to find the ileocecal junction.
Large Intestine
Push the small intestine to the left to find the ileocecal junction. Now trace in order from proximal to distal: cecum, appendix (if present), ascending colon, transverse colon (lift greater omentum to see it), descending colon, sigmoid colon, and rectum. Notice how the large intestine forms a box around the small intestine.
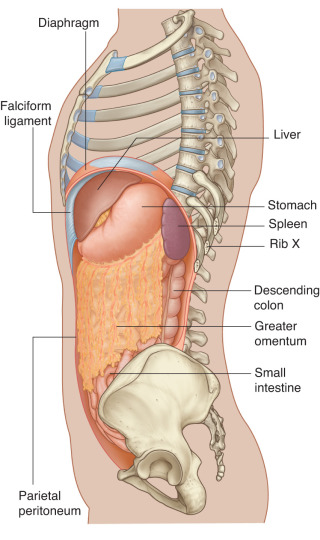
Peritoneum and Peritoneal Cavity
Use your hands to explore the peritoneal cavity, spaces, omenta, mesenteries, and peritoneal ligaments.
Identify:
■Parietal peritoneum (on the body wall)
■Visceral peritoneum (on the organs)
■The peritoneal cavity is the space between the parietal and visceral peritoneum.
REALIZE that the peritoneal cavity is a “potential” space. In a living person, there is very little space between the parietal and visceral layers of the peritoneum. This space is occupied by a thin layer of serous fluid that lubricates the organs and body wall and facilitates their friction-less movements.
The two parts of the peritoneal cavity are the greater sac and the lesser sac. With the anterior abdominal wall laid open, you are looking into the greater sac.
Identify these subparts of the greater sac:
■Sub-phrenic spaces between the diaphragm and liver (this space if further subdivided by the falciform ligament)
■Hepatorenal recess (aka—Morison’s pouch) between liver and the right kidney
■Paracolic gutters (between ascending/descending colon and lateral wall)
■Retrocecal recess (sometimes the appendix hides here!)
■Rectovesical pouch in males—in the pelvis, between rectum and bladder
■Recto-uterine pouch (pouch of Douglas) and vesico-uterine pouch in females (IF there is a uterus present)—in the pelvis, between rectum and uterus, and uterus and bladder, respectively.
Clinical correlation
The peritoneal pouches in the pelvis are clinically important because they are the most inferior parts of the peritoneal cavity, so fluids can collect here.
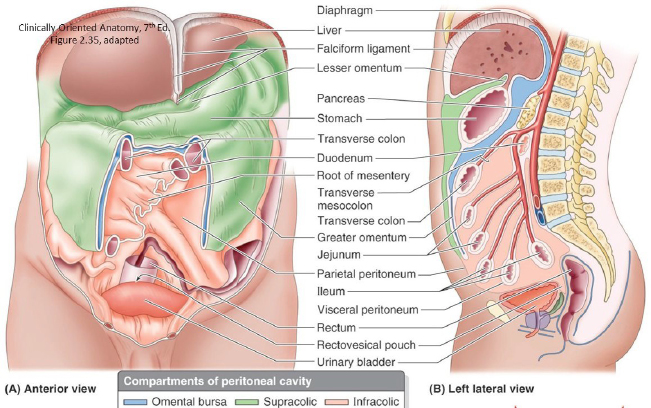
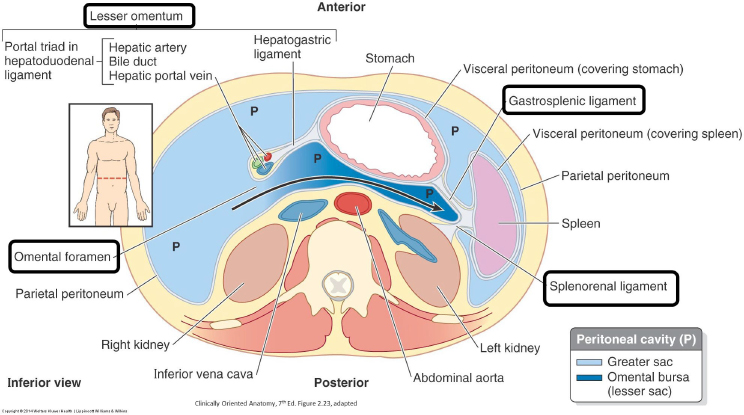
Lesser Sac
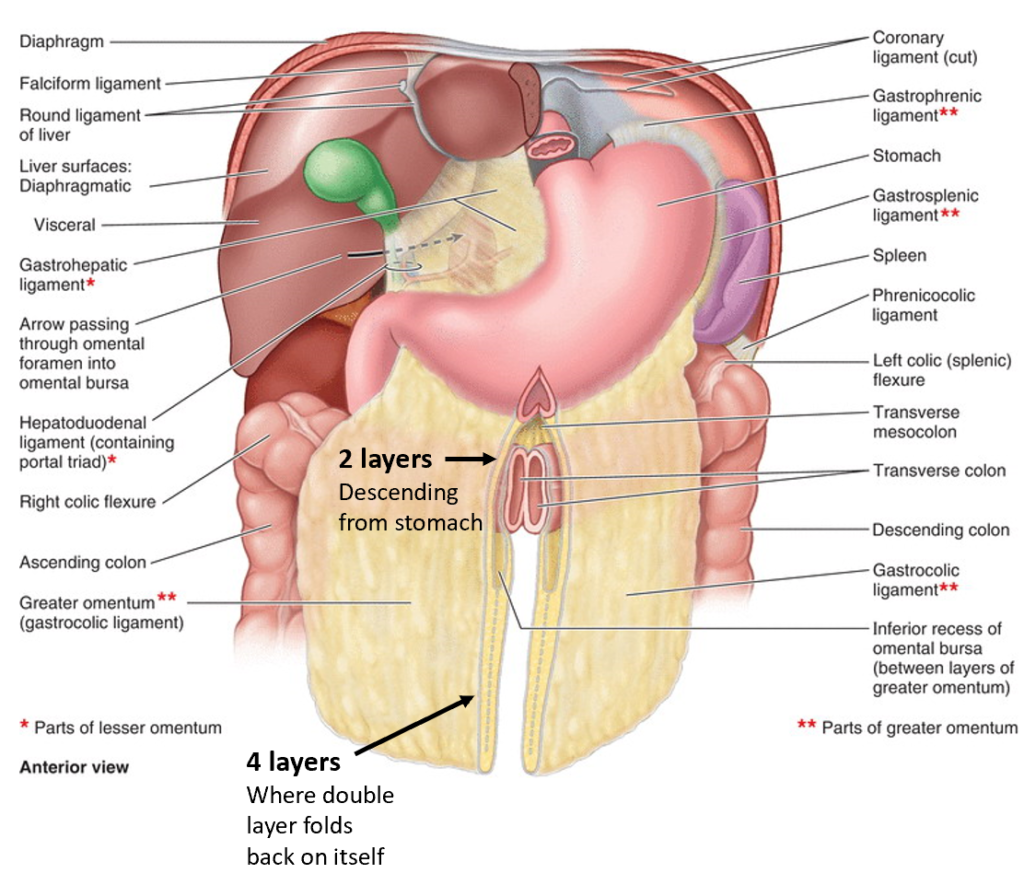
Where is the lesser sac? To find it, first we need to identify the lesser omentum. The lesser omentum is a mesentery that attaches the liver above to the stomach and first part of the duodenum below.
Complete anatomy
Omenta
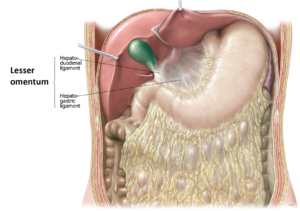
The lesser omentum has two parts:
1Hepatogastric ligament = very thin, almost transparent. Connects liver to lesser curvature of stomach.
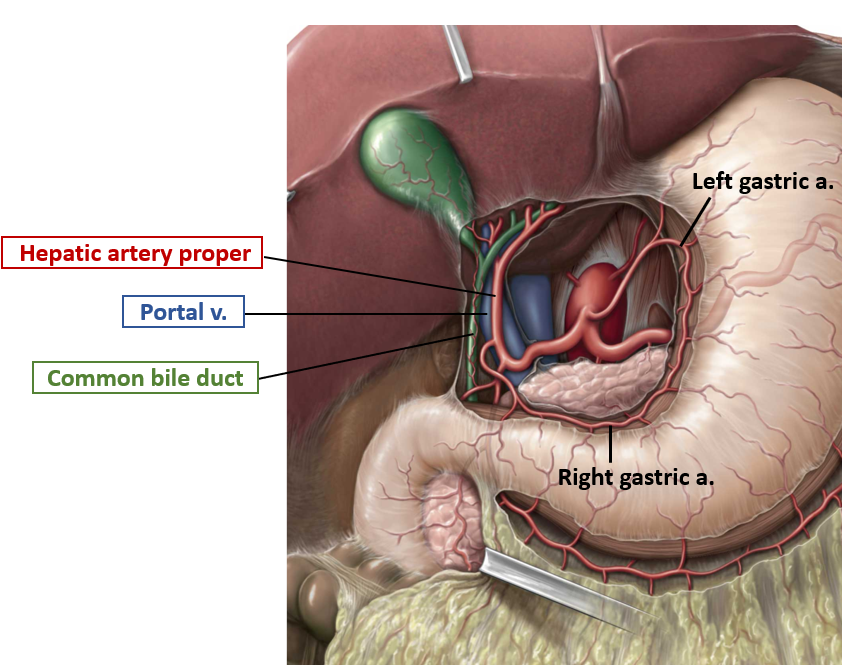
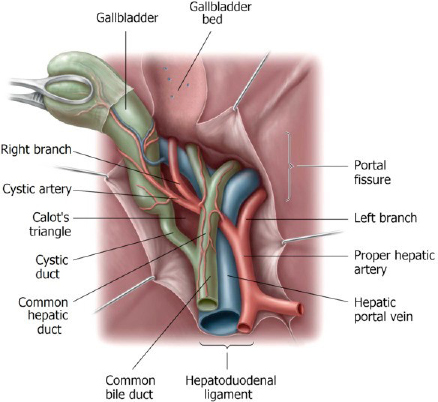
2Hepatoduodenal ligament = connects liver to first part of duodenum (the other parts of the duodenum are retroperitoneal). It is thick, because it contains the portal triad: the hepatic artery proper, the bile duct, and the portal vein. Feel the structures within the hepatoduodenal ligament between your thumb and finger.
Recall from embryology that the lesser omentum and falciform ligament are derived from the ventral mesentery of the stomach.
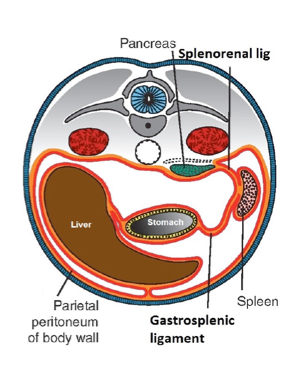
The lesser sac (omental bursa) is a blind pouch posterior to the lesser omentum and stomach. It gives the stomach space to move freely while churning.
Boundaries: anterior is the liver, stomach, and lesser omentum; posterior is peritoneum on the posterior abdominal wall.
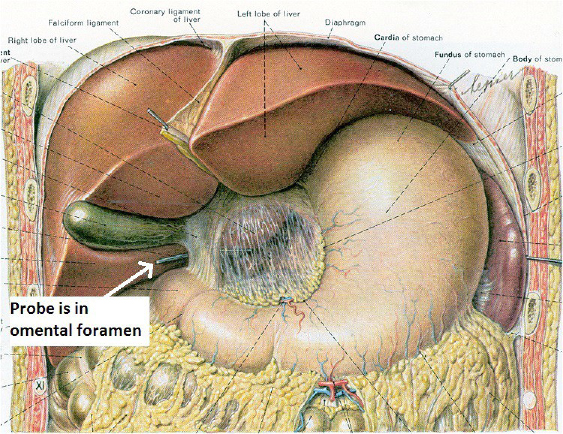
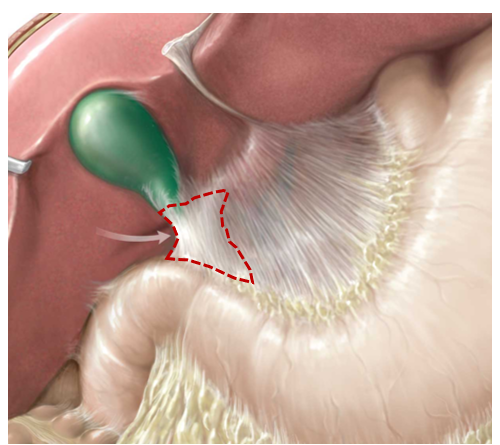
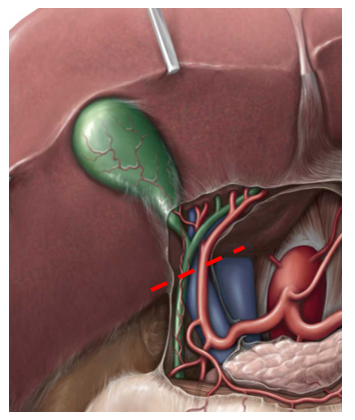
The lesser and greater sacs communicate via the Omental foramen (Foramen of Winslow), located posterior to the hepatoduodenal ligament. Place a finger in the omental foramen.
Anterior to your finger are the structures of the portal triad. Posterior to your finger is the IVC.
Greater Omentum
Examine the greater omentum, a double-layer of peritoneum hanging down like a fatty apron from the greater curvature of the stomach.
Note
The greater omentum may adhere to areas that were previously inflamed, resulting in a constricted appearance.
Identify its subdivisions:
■Gastrocolic ligament (stomach to transverse colon). This is the part that hangs from the greater curvature of the stomach like an apron.
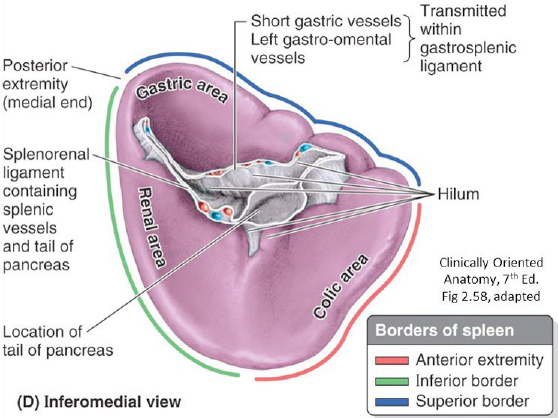
■Gastrosplenic ligament (stomach to spleen)
■Splenorenal ligament (reach way behind the spleen to feel it with your fingertips). It is the part of the greater omentum that connects to the posterior body wall.
The Other Mesenteries
Lift the greater omentum and identify the transverse colon. The double fold of peritoneum suspending it from the posterior abdominal wall is the transverse mesocolon.
Lift the ileum and jejunum and trace their mesentery proper to the posterior abdominal wall.
Trace the ileum to the cecum and find the appendix, often folded back behind the cecum. It has a small mesentery called the mesoappendix.
Trace the large intestine until you get to the sigmoid colon. It is suspended by a sigmoid mesocolon on the left side.
Mesenteries, peritoneal ligaments, and omenta are all structures composed of two layers of peritoneum. Mesenteries attach to the posterior abdominal wall, while omenta attach to the stomach.
List the structures that have mesenteries, and are thus mobile, and called “intraperitoneal” organs.
Which organs had a mesentery, but then lost it during development? These organs are “secondarily” retroperitoneal.
Supracolic Region
The transverse colon is used to divide the contents of the abdominal cavity into two areas: supracolic region (stomach, liver, gallbladder, pancreas, and spleen) and infracolic region (small intestine and large intestine). The pancreas straddles the two regions, but since it is derived from the foregut we will consider it with the other supracolic organs.
Dissect and clean structures of the portal triad.
Revisit the omental foramen by placing a finger in it. Anterior to it are the structures of the portal triad.
Complete anatomy
Portal Triad
Careful!
The structures are often stained green with bile, and the vein has thin walls!
Elevate the liver and use scissors to open a window in the lesser omentum in the middle of the hepatogastric ligament. The left and right gastric arteries run along the lesser curvature of stomach within the attachment of the lesser omentum.
Now you can explore the lesser sac = put your fingers in the superior recess of the lesser sac (behind the liver) and then into the splenic recess to the left between spleen and stomach.
Dissect the celiac trunk and its major branches.
This is a toughie, but we know you are up to the task. Please study atlas figures/Complete Anatomy screens and understand the architecture of the celiac trunk and its branches before you cut!
Complete anatomy
Celiac trunk
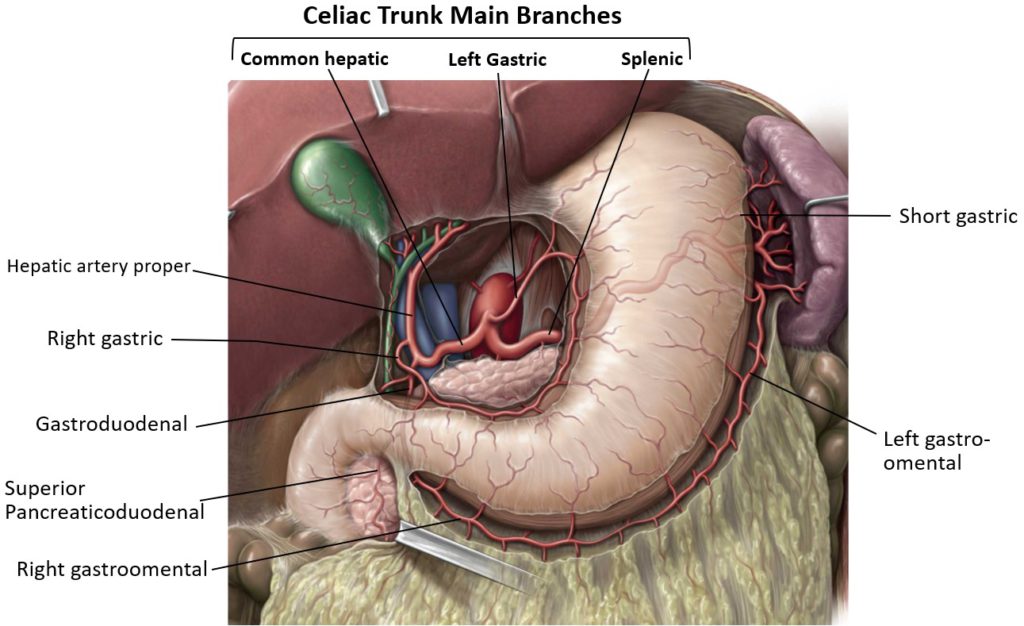
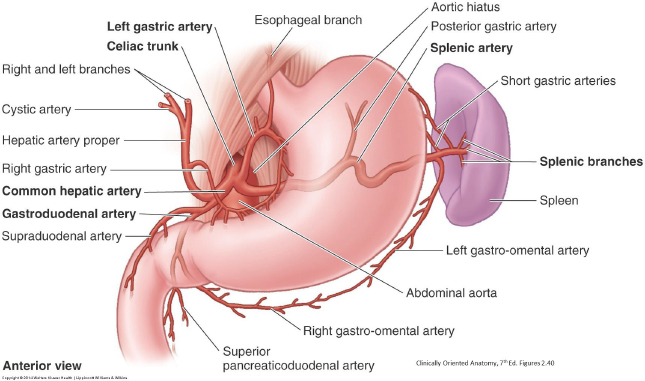
The celiac trunk is the first unpaired branch of the aorta—at T-12 just below the aortic hiatus of the diaphragm. Its branches supply foregut derivatives.
Finding the celiac trunk itself is tough since it is short and covered by peritoneum, and surrounded by a dense network of autonomic nerves (aortic plexus). The trick is to identify one of the three major branches (left gastric, common hepatic, or splenic artery), clean it, and follow it backwards to its origin from the celiac trunk.
Left Gastric Artery
Probe along the lesser curvature of the stomach near the esophagus to find the left gastric artery. Follow the left gastric artery back to the celiac trunk. Trace the right gastric artery along the right side of the lesser curvature.
■Gastric arteries anastomose within the lesser curvature of the stomach.
■Gastro-omental arteries anastomose along the greater curvature.
Summary
Where do the gastric and gastro-omental arteries arise?
Common Hepatic Artery
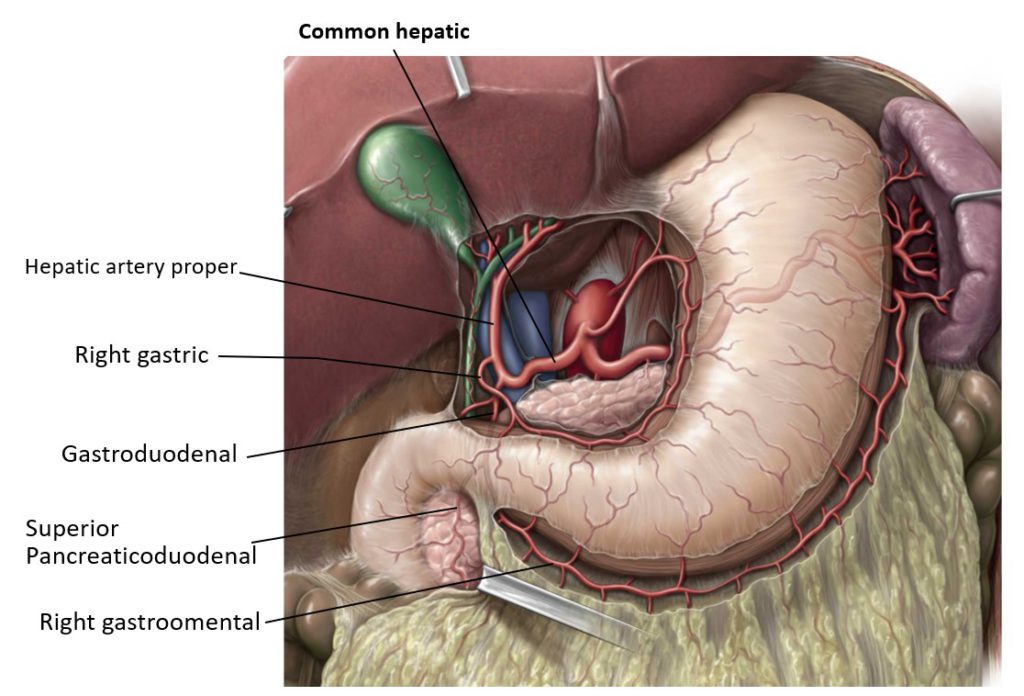
Go back to the structures you just dissected in the hepatoduodenal ligament and find the hepatic artery proper. Trace it back to the upper border of the duodenum where it unites with the gastroduodenal artery. From here, clean off and follow the common hepatic artery to the left where it joins the celiac trunk.
Find the remaining branches of the arteries you just identified. First, find the right gastric artery branching from the hepatic artery proper and running towards the lesser curvature of the stomach. Next, follow the gastroduodenal artery behind the duodenum and find where it branches into the superior pancreaticoduodenal and right gastroomental branches.
Splenic Artery
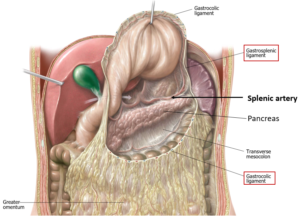
Follow the splenic artery: with scissors, open a hole in the gastrosplenic ligament to the left of the greater curvature of the stomach. Widen the opening with your hands by tearing into the gastrocolic ligament, from left to right, below the greater curvature of the stomach (be careful not to damage the gastro-omental arteries running along the greater curvature!) Elevate the stomach to reach the hilum of the spleen. You should see the pancreas just deep to the peritoneum on the floor of the lesser sac. Clean the hilum of the spleen to find the splenic artery. Trace the tortuous (twisty) splenic artery to the right until you reach the celiac trunk. It runs along the upper border of the pancreas and may be embedded in pancreatic tissue. See Figure 23.17.
Find the left gastro-omental artery passing from the splenic artery onto the greater curvature of the stomach (within the gastrocolic ligament). Keep following it, and it will merge with the right gastro-omental artery, which comes from the gastroduodenal artery.
Examine Figure 23.18.
Your beautiful dissection should look similar to this!! Make sure you have cleaned and identified the branches of the celiac trunk before you move on.
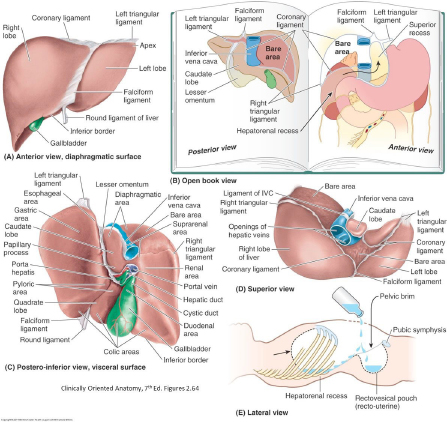
Liver and Gallbladder
Remove the liver in order to examine its surfaces.
Check with instructors first
We may want to keep a couple awesome portal triad dissections intact for the future.
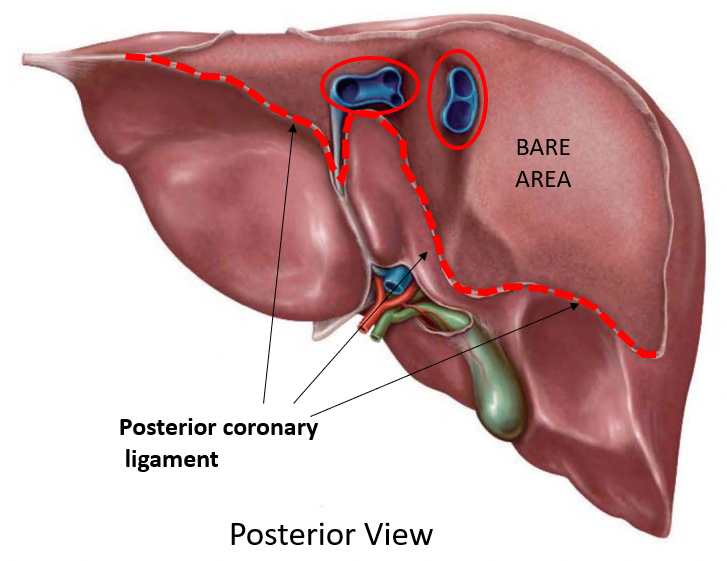
2Push the liver down and use scissors to cut the anterior layer of the coronary ligament and the two triangular ligaments away from their attachments to the diaphragm. As you apply downward pressure on the liver, use blunt dissection with fingers to free up the diaphragmatic surface until you can see the IVC passing up into the diaphragm behind it.
Note
If you are having trouble, you may need to remove a few costal cartilages and some of the diaphragm for better access.
3Continue to apply downward pressure as you cut the posterior layer of the coronary ligament behind the liver. Cut through hepatic veins as they enter the IVC posterior to the liver.
4Try to remove the liver—if it is held up, it may be that the IVC is passing through the liver itself, in which case you will have to remove part of the IVC with the liver. Cut through the IVC in two places: Above the liver as it passes into the diaphragm and below the liver where the IVC is behind the omental foramen. Lift the liver out of the cadaver! Voilà!
Examine the Surfaces of the Liver
■The liver has two surfaces: Diaphragmatic and Visceral.
■The surfaces of the liver are separated by the sharp inferior border. The inferior border is palpated when you examine a patient’s liver.
LOCATE these peritoneal structures on the diaphragmatic surface (they may not be prominent):
■Falciform ligament
■Coronary ligament: Anterior and Posterior layers. The coronary ligament perches atop the liver like a “crown,” connecting the liver to the diaphragm
■The bare area of the liver is between the layers of the coronary ligaments. Why is it called “bare”?
Anatomic Lobes of the Liver
■Right and Left Lobes: Best seen on the diaphragmatic surface where they are separated by the falciform ligament
■Caudate and Quadrate Lobes: Seen on the visceral surface
Complete anatomy
Visceral Surface of the Liver
FIND these landmarks/structures on the visceral surface (brought to you by the letter H):
■Right sagittal fissure
■Contains the IVC and the fossa that contains the gallbladder
■Left sagittal fissure
■Contains the ligamentum venosum and the round ligament of the liver
■These ligaments are remnants of embryonic blood vessels = which ones?
■Porta hepatis (cross bar of the H)
■The caudate and quadrate lobes are sandwiched between the sagittal fissures
Chalk Talk
This is a good time for a Chalk Talk on the visceral surface of the liver.
Review the concept of “functional” parts of the liver.
■The part of the liver to the right of the right sagittal fissure is the functional right liver.
■The part of the liver to the left of the right sagittal fissure is the functional left liver. It includes the caudate and quadrate lobes.
Turn the liver over to the visceral surface and clean structures in the porta hepatis.
Often, everything is green here, so be sure you’re following your vessels.
CLEAN and FIND:
■Hepatic artery proper
■Right and left hepatic arteries (be aware of variations)
■The cystic artery is usually a branch of the right hepatic artery. Surgeons locate it within the triangle of Calot. See Figure 22.23.
■(Common) Bile duct
■Common hepatic duct
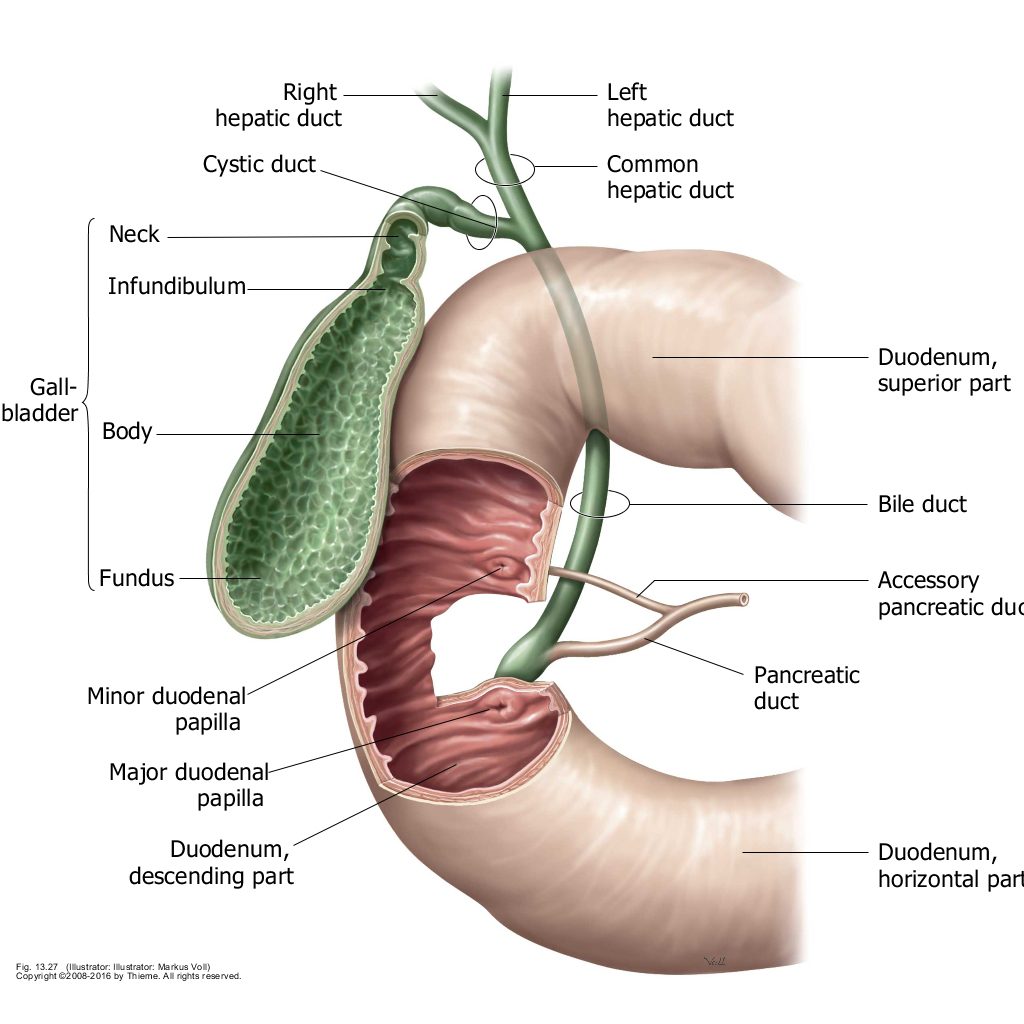
■Cystic duct
■Portal vein—the portal vein divides in the porta hepatis into left and right branches—this is one of the rare cases where a vein branches!
Gallbladder
Stomach
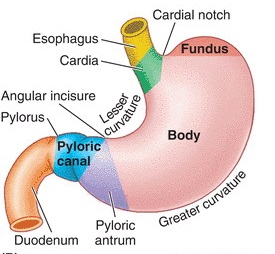
EXAMINE the stomach and identify its parts and relationships:
NAME these parts of the stomach:
■Cardia, fundus, body, and pyloric part.
SURFACE FEATURES of the stomach include:
■Cardiac notch and Greater and Lesser Curvatures.
Examine the stomach’s relations with other organs and omental bursa:
■Anterior: diaphragm, left lobe of liver
■Posterior: lesser sac, pancreas, spleen, left kidney, and left suprarenal gland
Spleen
The spleen has two surfaces: Diaphragmatic and Visceral. The diaphragmatic surface is curved to conform to the underside of the diaphragm. The visceral surface contains the hilum of the spleen where the vessels enter.
Duodenum and Pancreas
With the liver removed, clean the duodenum and pancreas.
Behind the stomach, strip the peritoneum and clean the head of the pancreas and first and second parts of the duodenum.
1Clean and follow the gastroduodenal artery behind the duodenum where it gives off two arteries:
■You already found the right gastro-omental artery onto the greater curvature of the stomach.
■If you didn’t find it already, look for the superior pancreaticoduodenal arteries on the head of the pancreas. They’re small, so no worries if you can’t find them.
CONCEPT
The pancreaticoduodenal arteries (superior from the celiac, inferior from the superior mesenteric artery) meet/ anastomose in the duodenum and head of the pancreas.
Complete anatomy
Gastroduodenal Branches
Open the stomach and duodenum.
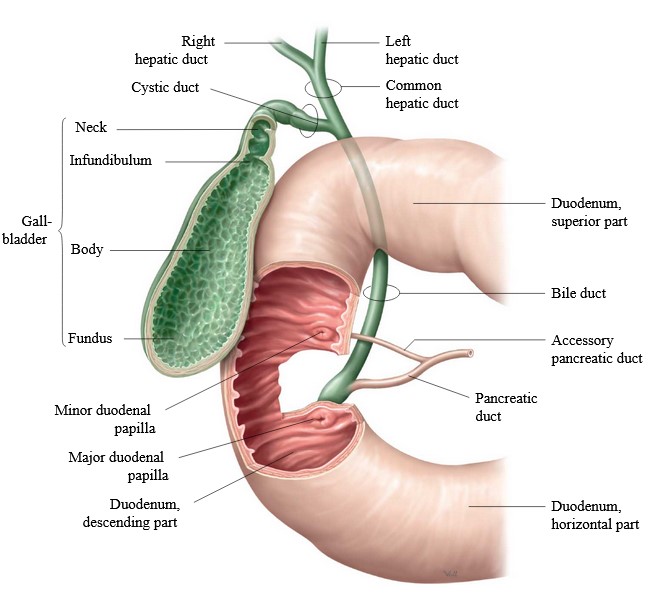
To study the internal anatomy of the duodenum, first examine Figure 23.31, then follow these steps:
1Open the anterior wall of the body of the stomach with scissors. Clean out gastric contents to find gastric folds (rugae). These are temporary folds that flatten out as the stomach fills.
2Make a horizontal incision through the junction of the stomach and duodenum to see the pyloric sphincter.
3With a vertical incision, open the entire length of the descending duodenum. Observe the circular folds. These are permanent folds that help to increase the absorptive surface area.
Dissect out the pancreatic and bile ducts.
Complete anatomy
Bile and pancreatic ducts
Follow the bile duct inferiorly behind the superior duodenum and head of the pancreas. Use scissors and forceps to carve away pancreatic tissue to locate the union of the bile duct and main pancreatic duct in the head of the pancreas, medial to the descending part of the duodenum.The (common) bile duct and main pancreatic duct unite in a muscular chamber: the hepatopancreatic ampulla.
Note
Sphincters are present in the distal part of the bile duct (the Choledochal sphincter), and in the hepatopancreatic ampulla (Sphincter of Oddi). You won’t see these but know where they are located.
The ampulla causes an internal bulge in the mucosa within the lumen of the descending duodenum (2nd part). This bulge is the major duodenal papilla; look in the duodenum to see if you can locate this. Both bile from the liver and digestive enzymes from the pancreas enter the duodenum through the orifice atop the major duodenal papilla.
Checklist, Lab #23
Review and make sure you have identified each of the structures below.
Internal aspect of anterior abdominal wall
Median umbilical fold w/ligament (urachus)
Medial umbilical folds w/ligament (obliterated umbilical arteries)
Inferior epigastric vessels
Peritoneum and peritoneal cavity
Parietal and visceral peritoneum
Peritoneal cavity
Greater sac
Subphrenic spaces
Hepatorenal recess
Paracolic gutters
Retrocecal recess
Rectovesical pouch (in pelvis—male)
Recto-uterine and uterovesical pouches (in pelvis—female, when uterus is present)
Lesser sac
Omental foramen
Lesser omentum
Hepatoduodenal ligament
Hepatogastric ligament
Greater omentum
Gastrocolic ligament
Gastrosplenic ligament
Splenorenal ligament
Mesentery of the small intestine
Transverse mesocolon
Sigmoid mesocolon
Details of supracolic structures
Abdominal esophagus
Liver
Diaphragmatic & visceral surfaces
Anatomic Lobes: right, left, caudate, quadrate
Right and left sagittal fissures
Porta hepatis
Coronary ligament of liver (anterior & posterior layers)
Bare area of liver
Falciform ligament
Ligamentum venosum (vestige of ductus venosus)
Round ligament of liver (vestige of umbilical vein)
Gallbladder
Fundus, Body, and Neck
Cystic duct
Common hepatic duct
Common bile duct
Portal vein
Portal triad = hepatic artery proper, bile duct, and portal vein
Stomach
Cardia & cardiac notch
Fundus and Body
Greater and Lesser curvatures
Pyloric part with pyloric sphincter
Gastric folds (rugae)
Duodenum = 4 parts
Superior (1st part), descending (2nd part), inferior/horizontal (3rd part), and ascending (4th part)
Pancreas
Head w/uncinate process
Neck, Body, and Tail
Bonus points for locating the Main pancreatic duct
Hepatopancreatic ampulla (= union of Bile duct + Main pancreatic duct)
Major duodenal papilla
Spleen: visceral and diaphragmatic surfaces
Celiac trunk
Left gastric artery
Splenic artery
Left gastro-omental artery
Common hepatic artery
Right gastric artery (can be quite small . . . so bonus points if you find it)
Gastroduodenal artery
Right gastro-omental artery
Hepatic artery proper
Right & left hepatic arteries
Bonus points for cystic artery (supplies gallbladder—usually a branch of the right hepatic artery)