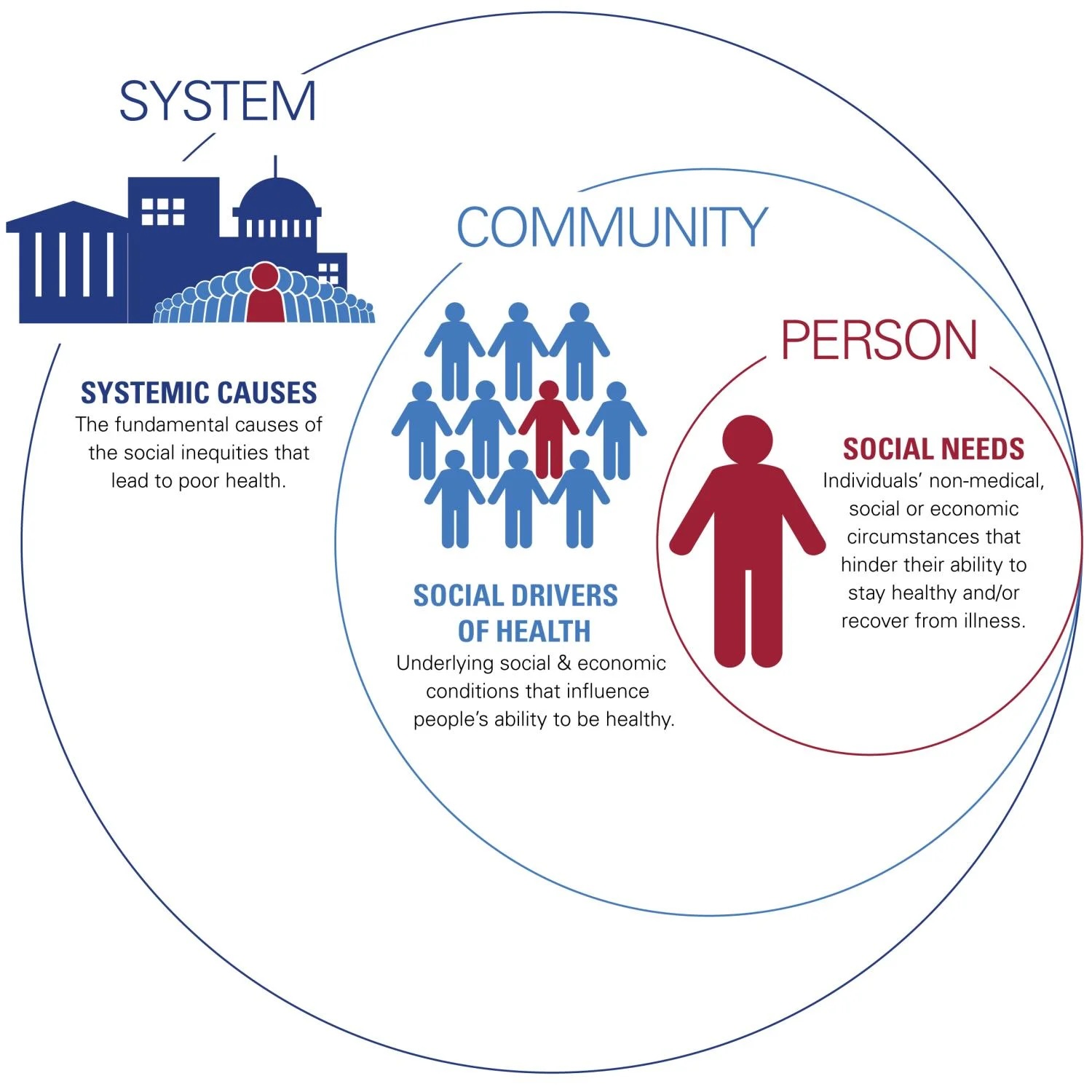
Social determinants of health
Addressing the social determinants of health (SDOH) requires an upstream approach to identify the underlying causes of health inequities.
Solutions require
- Collaboration among public health entities, both public and private.
- Healthcare organizations and providers.
- Community partners.
- K-12 and academia.
- Faith-based organizations
- Policy makers.
Such collaboration can lead to evidence-base initiatives to address the social and societal factors that affect health outcomes.
Strategies include
(but are not limited to)
- Increase knowledge and understanding about the impact of SDOH on health outcomes.
- Tailor the information to different audiences, (e.g., the public, community-based organizations, and healthcare partners) will enable each to identify their niche(s) and their role in improving health outcomes.
- Community based organizations have a ground-level understanding of the needs, challenges, and resources within their communities.
- They have established trusting relationships with the individuals within their communities.
- They are best served to tailor interventions to address the unique social and societal factors impacting health outcomes of their members.
- Employing and supporting community health workers can build rapport with individuals who may not trust those outside of their community, which facilitates navigating resources and services.
- Transportation: Provide transportation assistance to help patients attend appointments.
- Affordable housing: Address housing insecurity by connecting individuals with affordable housing options.
- Food security: Improve access to healthy, affordable food through initiatives like food banks and community gardens.
- Financial assistance: Connect individuals with financial resources and support programs.
- Childcare: Offer childcare services to make it easier for parents to attend appointments or participate in programs.
- Education: Provide opportunities for individuals to improve educational attainment that improve their lives and their family members.
- The first step in a public health approach is to define and monitor the issue through the use of relevant data.
- Surveillance involves the collection, analysis, and interpretation of information to track the occurrences and trends of health issues.
- Evaluation of the significance of the issue and its impact on the community uses data from sources such as hospital records, surveys, and vital statistics.
- Data sharing between healthcare organizations, social service agencies, community-based organizations, public-health entities, and policy makers becomes a necessity.
Public health advocacy is a process of influencing public policy to improve population health. It involves educating the public and policymakers about the importance of health issues and the need for specific policies. Advocacy can lead to:
- Change in systems and policies that affect populations, such as increasing minimum wage, promoting affordable housing, improving educational quality, and expanding access to social protection programs.
- Address root causes, (i.e., the underlying or root causes for the social, economic, and environmental factors) that contribute to health disparities:
- Poverty.
- Discrimination.
- Lack of access to education and employment.
- Create healthy environments that make healthy choices the easy choices and more socially normative, (i.e., passive behavior change).
- Invest in human capital by supporting, investing in, and promoting:
- Education.
- Early childhood development.
- Job training.
Public health policy and advocacy examples
Tobacco control
- Clean air laws.
- Tobacco regulations and taxes.
Nutrition and food policies
- Healthier food options in schools.
- Restrict marketing of unhealthy foods to children.
- Improve food access in underserved communities.
Environmental health
- Pollution reduction policies.
- Protection of natural resources.
- Address climate change.
Health equity
- Address systemic barriers to health, (e.g., lack of access to healthcare, affordable housing, and healthy food options, particularly for marginalized communities).
Societal factors that influence health: A framework for hospitals
American Hospital Association (AHA) framework
Who: Individuals who present for health care services.
Setting: Patient encounter at a point of care.
Examples:
- Lack of stable housing.
- Homelessness.
- Limited access to healthy food.
- Insufficient transportation options.
- Loneliness.
- Human trafficking.
- An unsafe home environment.
Strategies: Patient-level interventions can mitigate non-medical social and economic challenges.
- Hospitals can:
- Screen and document social needs.
- Gather race, ethnicity, and language data.
- Utilize relevant ICD-10-CM Z codes.
- Create interdisciplinary care teams that include social workers, case managers, and community health workers.
- Establish hospital-based food pharmacies.
- Connect to temporary supportive housing.
- Partner with ride shares to provide transportation to medical appointments.
- Provide referrals to social service organizations.
- Provide assistance in signing up for medical and social benefits.
Who: The community served by the hospital.
Setting: In the community—where people live, learn, work, play, and pray.
Examples:
- Food deserts.
- Lack of affordable housing.
- Community violence.
- Inadequate public transportation.
Strategies: Hospitals can lead, convene, collaborate, invest in or support activities that improve the community environment with multi-sector stakeholders.
- Hospitals can:
- Support local food banks and meal delivery services.
- Partner with economic development organizations and contribute to the local investment environment.
- Build grocery stores in food deserts.
- Invest in affordable housing.
- Foster employment and career advancement opportunities.
- Advocate for the public transportation ecosystem.
Who: Anchor organizations, such as hospitals and health systems, community leaders, legislators or policymakers.
Setting: Community, state or national.
Examples: Systemic inequities such as:
- Racism.
- Sexism.
- Generational poverty.
- Redlining by financial institutions.
- Environmental injustice.
- Educational systems.
Strategies: In partnership with other stakeholders, hospitals can support and affect policy, system, environmental and cultural changes to achieve widespread impact on societal issues.
- Hospitals can:
- Incentivize investments in poor communities.
- Develop health career partnerships with local school districts.
- Advocate for the removal of barriers to cross-sector and inter-agency coordination.
- Invest in early childhood education.
Source: AHA.