Emergency department
Based on the patient’s H&P and labs, the ED attending recommends admission and further work-up.
You are a fourth-year medical student on your hospitalist rotation when you receive a call from the ED to admit a “32-year-old Hispanic AMAB, who presented to the ED with a 2-month history of cough, occasional fevers, and weight loss.”
The following diagnostics have been performed:
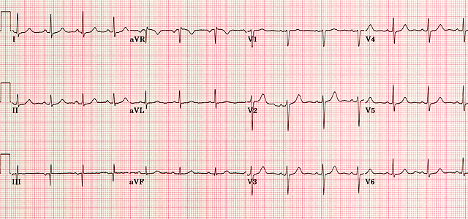
ECG
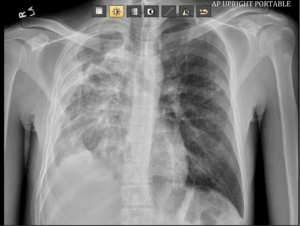
Imaging
Clinical information
Cough.
Comparison
Previous CXR received from Federally Qualified Health Center (FQHC) urgent care.
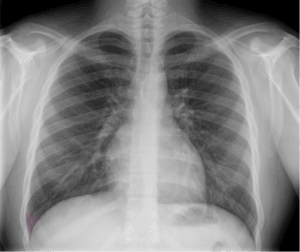
Findings
Right lung consolidation with moderate hydropneumothorax. Normal cardiomediastinal silhouette. No pneumothorax, pleural effusion, or adenopathy. No significant bone abnormality.
Impression
Right lung consolidation with moderate hydropneumothorax could represent pneumonia with parapneumonic effusion versus cavitary pneumonia. Further evaluation with CT is recommended.
Clinical information
Cough and fever for six months. Abnormal chest radiograph.
Comparison
XR chest AP portable (5/23/2025) We try not to have dates. Is this necessary?
Procedure
Axial images through the chest after the administration of 75ml Omnipaque 350 intravenous contrast. Multiplanar reconstructions.
At least one of the following CT dose optimization techniques were used: Automated exposure control; adjustment of mA and/or kV according to patient size; use of iterative reconstruction technique.
Findings
Lungs: Cavitary consolidation of the right-upper lobe as well as of the regions of cavitation within the right-middle and lower lobes. The greatest degree of cavitation is present within the right-upper lobe measuring at least 5.4 × 5.3 × 4.8 cm. Scattered centrilobular airspace opacities involving the right greater than left lung. No cavitation within the left lung.
Multilocular right-sided pleural effusion with complex thin septations. Pleural collection along the anterior inferior right hemithorax measures at least 4.7 × 7.5 cm. Additional loculated posterior pleural component is mild to moderate in severity.
Mediastinum: Normal heart size without pericardial effusion. No pathologically enlarged lymph nodes.
Coronary artery calcification: Minimal or no coronary calcification.
Partial visualization upper abdomen: Negative.
Musculoskeletal: Negative.
Impression
- Multifocal cavitary pneumonia involving the right lung with multilocular right-sided parapneumonic effusion. Findings compatible with necrotizing pneumonia and associated empyema. Significant cavitation involving the right-upper lobe, detailed above. Recommend cardiovascular surgical consult.
- Scattered centrilobular airspace opacities involving the right greater than left lung, likely infectious or inflammatory.
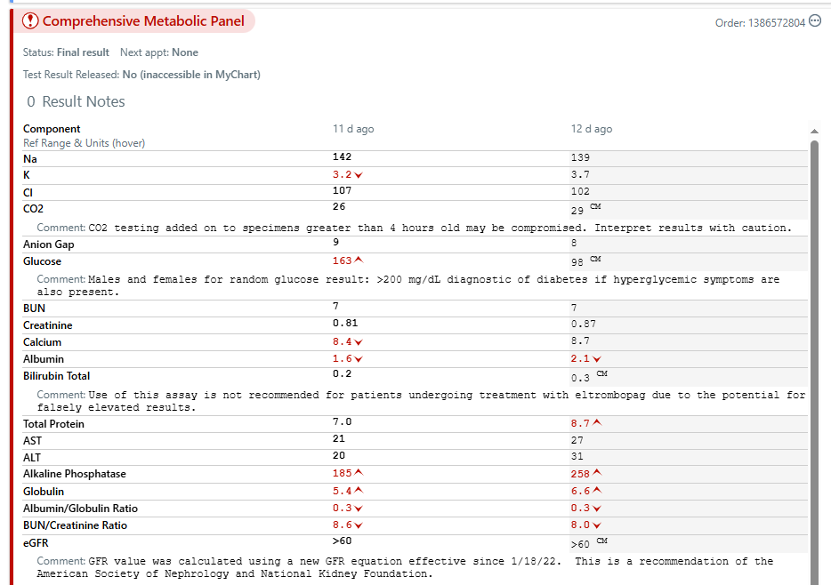
Labs
think about this
If you were a fourth-year medical student on an ED rotation, what other tests would you want to order? Share your thoughts in the Slack channel.
Medications: Ibuprofen; per patient, he’s been on two courses of antibiotics and an albuterol inhaler, which he has with him.
Allergies: None.
You learn Raul prefers to be called Ray and has been sick for almost three months with symptoms of cough, fatigue, and weight loss. He’s been on antibiotics twice (he doesn’t remember the names of the antibiotics but remembers the first one was five days and the second one made him feel (“Enfermo en el estómago.” You know enough Spanish to understand it made him sick in his stomach.)
You ask about his fever. Ray says he felt warm when he first got sick and a little sweaty, but it’s been hot outside. The bunk house where he sleeps does not have air conditioning, and the old fan stopped working weeks ago.
You ask him to describe the cough. Ray says that this is what’s been bothering him the most because it makes it hard to work. It occurs “all the time,” sometimes worse at night, definitely worse when he is working in the orchard, especially after it has been sprayed.
Occasionally, Ray coughs up some green stuff (mucus). You ask about hemoptysis—Ray and the translator look at you because they do not know what you mean. You rephrase: “Have you coughed up any blood?” Ray says, “Sí.” The translator continues: “Once after I coughed really hard, my chest hurt, and I had a bit of blood in my hand.”
You ask more about the chest pain. Ray says (through the translator) that when he had been either coughing hard or working hard, his chest hurt, kind of like if he got punched. Sometimes he gets a sharp pain when he takes a deep breath in or out.
You complete your HPI by asking him about his weight loss and fatigue. He notes he loses weight every year when he is working the farms— long hours and not so great food—but he has never lost this much weight. He had to put a few more notches in his belt to keep his pants up. As for fatigue, Ray tells you that he feels run down (exhausted) all the time, lacks energy. Although he has had some light duty work in the warehouse, he has not recovered like he thought he should. This worries him. He does not want to risk not staying on as a hire for the rest of this season or being able to come back. He prefers orchard work in the region, and he needs to send money home to his family.
Adult Medical Illnesses: None.
Childhood Illnesses: Chickenpox, strep throat, fractured right radius as teenager.
Surgical History: None.
Trauma: None.
Habits/Risk Factors: Occasional beers.
Preventive Health History: Knows he received vaccinations as a child, otherwise doesn’t see a physician.
Social History: Migrant farm worker; wife, 3 children, and other family live in Navojoa; he returns there after the season in Washington.
Family History: Unremarkable for medical problems; mother has arthritis in her hands and back, as does his father.
Bolded indicate positive results.
General: Fever, chills, night sweats, exhaustion, and weight loss.
Dermatologic: No rashes, changes in skin color, masses or lesions, itching, hair loss, or changes in hair or nails.
HEENT
- Head: No headaches, head injury, dizziness, or lightheadedness.
- Eyes: No changes in vision including double vision, eye pain, or photophobia.
- Ears: No hearing loss, tinnitus, vertigo, or otitis.
- Nose: No epistaxis, nasal stuffiness, sinus trouble, or hay fever.
- Neck: No lumps, pain, or neck stiffness.
- Throat (oropharynx): No bleeding gums, frequent sore throats or oral ulcers, or hoarseness.
Respiratory: As per HPI, denies wheezing.
Cardiovascular: Chest pain, dyspnea on exertion; no pedal edema, palpitations, or claudication.
GI: Nausea; no vomiting, abdominal pain, dysphagia, heartburn, diarrhea, constipation, hepatitis, jaundice, hematemesis, or melena.
GU: No dysuria, frequency, urgency, hesitancy or hematuria, or penile discharge.
MSK: No pain, swelling, stiffness, or locking of joints.
Psych: Mild anxiety (situational, wondering what’s going on); no depression, sleep disturbance, hallucinations, or suicidal ideations.
Neuro: No loss of consciousness, seizures, paralysis, weakness, numbness, or involuntary movements
Hematopoietic: No prolonged bleeding, easy bruising, or known anemia.
Endocrine: No polyuria, polydipsia, or heat or cold intolerance.
General appearance: Ray is a mildly il-appearing Latino male, appears stated age, somewhat pale in appearance and gaunt.
Vital Signs
- BP 114/72, right arm, sitting.
- P 92 regular.
- RR 20.
- T 100.
- PaO2 95%.
Skin: Dry, warm. No jaundice, rashes, or skin irregularities.
HEENT: Normocephalic.
- Eyes: Sclerae w/o icterus, conjunctivae clear. PERRLA, EOMs intact. Fundi normal bilaterally w/o papilledema, hemorrhages, or exudates.
- Ears: External ear canals clear; TMs with visible light reflex and w/o erythema, bulging, or perforations bilaterally. Hearing grossly intact to conversational voice.
- Nose: No nasal polyps. Nasal mucosa/turbinates without lesions or hemorrhages.
- Oropharynx: No pharyngeal erythema or exudates. Oral mucous membranes are pale, moist, without lesions. No tonsillar enlargement. Good dentition.
- Neck: Full range of motion. Thyroid smooth, non-tender, normal in size and consistency and without nodules. Trachea midline.
Lymph nodes: No submandibular, cervical, axillary, epitrochlear, or inguinal adenopathy.
Thorax: AP diameter not increased. No deformities, ribs easily visible.
Lungs: Increased respiratory effort, symmetrical chest expansion, no accessory muscle use. Right lung fields demonstrate decreased breath sounds and egophany, especially at base, some crackles upper field; tactile fremitus, dullness with percussion throughout entire right lung field.
Cardiovascular: Regular rate and rhythm. S1 and S2 normal; no murmurs, gallops, rubs, heaves, or thrills. PMI palpable in the 5th left intercostal space in the midclavicular line. No JVD. Carotids full on palpation without bruits bilaterally.
Peripheral pulses: Radial, brachial, femoral, posterior tibialis, and dorsalis pedis pulses symmetrical and full with normal upstroke. No carotid, aortic, renal, or femoral bruits.
Abdomen: Soft, scaphoid, without scars or distention. Normal bowel sounds, no abdominal bruits. No tenderness to superficial or deep palpation, no palpable masses. No rebound tenderness. No hepatosplenomegaly
Back: No kyphoscoliosis; no vertebral or costovertebral angle tenderness to fist percussion.
Extremities: Full range of motion; no joint deformities. No clubbing, cyanosis, or edema.
Neurologic: CN2–12 grossly normal; no focal sensory or motor findings upper/lower extremities.
Mental Status: Alert and oriented ×4, cooperative, appropriate.
think about this
Based on the lab results so far, what consultations would you order? Share your thoughts in the Slack channel.
think about this
In the Slack channel, write your admission orders using the mnemonic ADCVANDISMAL.
think about this
Discuss in the Slack channel. Based on your admission orders, Ray is admitted to the hospital. Consultations are performed. Based on the available labs and consultations:
• What is your current differential diagnosis?
• What medications would you start and why?
Public Health correlation
Health Policy and Advocacy
- Should migrant farmworkers receive more targeted public health interventions (e.g., TB screening, access to paid sick leave, mobile clinics)?
- What policies could support this?
Occupational and Environmental Health
- Should physicians ask about workplace exposures more routinely in patients like Ray? Why or why not?
- What responsibilities do employers, public health systems, or physicians have in identifying and addressing work-related health hazards?
Public health systems response
- How well are local public health departments equipped to address the needs of migrant agricultural workers?
- What data would public health agencies need to proactively prevent cases like Ray’s from progressing to hospitalization?
- How could a community-based intervention (e.g., health outreach at work camps) have changed this trajectory?
Image credits
Unless otherwise noted, images are from Adobe Stock.