Add Your Heading Text Here
Authors
Keely Coxon, MD
Dawn DeWitt, MD
In this module
Overview: Clinical syndrome featuring progressive cognitive decline
- Signs and Symptoms
- Onset is usually gradual and persistent (exceptions: Cruzfeldt-Jacob encephalopathy; Kuru).
- Behavioral changes.
- Cognitive deficits:
- Memory loss.
- Impairment of communication or language.
- Agnosia (inability to recognize familiar objects).
- Apraxia (inability to perform familiar tasks).
- Impaired executive function (reasoning, judgment, and planning).
- Impaired ability to function independently.
A note about this condition
It is often a challenging and expensive condition to manage. It accounts for annual taxpayer burden of more than a billion dollars in both the United States and Canada. It can place a great deal of strain on families, as they try to arrange care for patients.
Living with dementia
Dementia affects millions of people. These videos may bring up distressing feelings if you have family or friends with dementia. Please don’t hesitate to reach out to discuss any issues, thoughts, or feelings that arise for you as you work through this module.
This brief video interviews 4 people with dementia and represents the challenges people face.
This 20-minute video interviews Sarah, a very articulate woman living with dementia.
Screening for dementia in asymptomatic adults
- assessment
- diagnosis
Workup depends on whether the presentation is typical or if there are atypical features such as young age, rapid onset, other neurologic signs (like Parkinsonism).
- If the presentation is relatively typical (older adult [>65 years old], gradual short-term memory loss as the initial symptomatology, then the basic workup is usually:
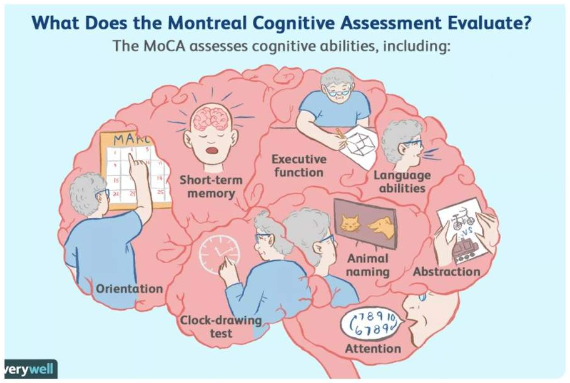
- Screening neurologic exam and MoCA.
- Basic metabolic, B12, TSH, vit D.
- MRI (with contrast if early/rapid onset), CT first test acceptable.
- RPR, Viral PCR.
- Consider sleep studies.
- If younger, atypical or rapid onset, consider other diagnoses:
- Toxin exposure (ETOH, other), Infectious dz w/u (HIV, RPR, Lyme).
- Rheumatology eval.
- Paraneoplastic?
- For early onset or unusual presentations, consider the following with neurologic consultation:
- CSF amyloid β42; Tau/P-tau levels.
- Consider PET if CSF not available.
- Dementia vs. delirium: They can co-occur!
- Dementia = progressive cognitive decline.
- Mainly affects memory.
- Typically caused by changes in neuroanatomy.
- Delirium = reversible decline in cognition.
- Mainly affects attention.
- Typically caused by acute illness, drug adverse effect, or substance use (including ETOH).
- Dementia = progressive cognitive decline.
- Mild cognitive impairment (MCI): relatively mild, objective cognitive deficits that do not meet the criteria for dementia, but are more than those expected with normal aging.
- Patients are still typically able to function independently.
- Stroke.
- Mass.
- Tumor.
- Abscess.
- Co-existing mood disorders (e.g., depression).
- Conditions that can be chronic: E.g., undiagnosed hypothyroidism, vitamin deficiencies, neurosarcoidosis, etc.
Types of dementia
- Alzheimer’s disease.
- Frontotemporal dementia.
- Subtypes: Behavioral variant frontotemporal dementia.
- Primary progressive aphasia.
- Motor disturbance:
- Amyotrophic lateral sclerosis (ALS).
- Corticobasal syndrome.
- Progressive supranuclear palsy.
- Lewy body dementia.
- Huntington’s disease.
- Normal pressure hydrocephalus (NPH).
- Vascular dementia.
- Creutzfeldt-Jakob disease (CJD).
- Korsakoff syndrome.
- Others (not discussed in this module): Mixed dementia, Parkinson’s disease dementia, posterior cortical atrophy, etc.
Alzheimer disease
- diagnosis
- diagnostic testing
- treatment
- Memory impairment (recent memory, forgetfulness) is usually 1st sx.
- Problems with memory, finances, navigating, etc.
- Insight preserved: Anxiety and depression as patient realizes.
- Lack of motor symptoms in early stages (i.e., no tremor, etc.)
- Delusions and hallucinations are uncommon in early stages. If present, consider Lewy body dementia or other diseases.
- Preserved ADLs.
- In younger-onset AD, memory impairment may initially be limited with other sx more common.
If indicated may show the following:
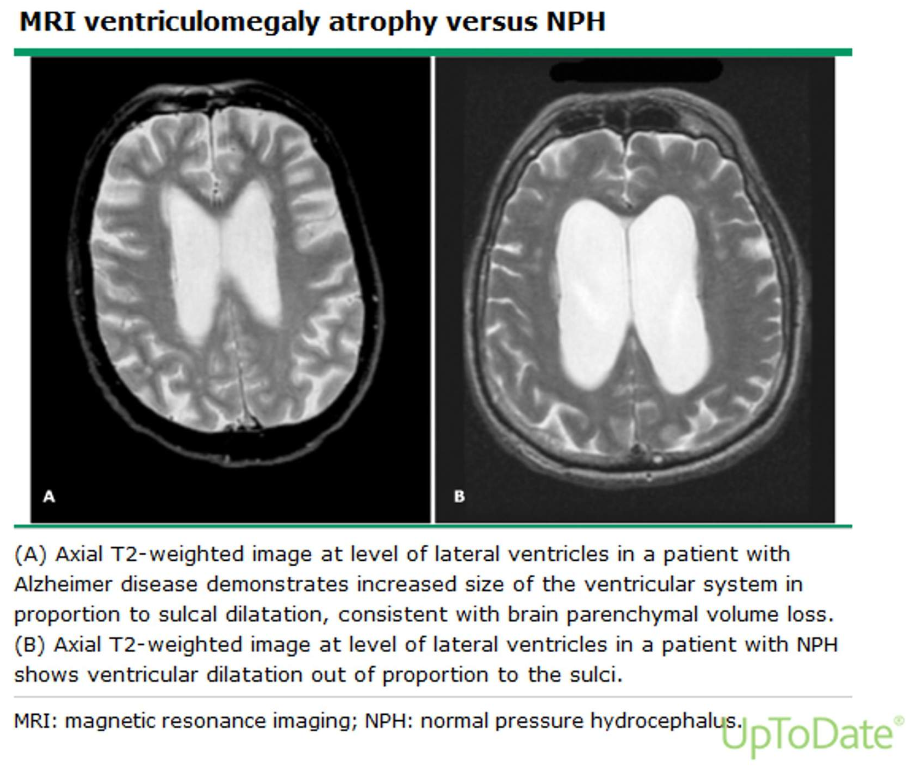
- Hippocampal atrophy (MRI) is non-specific but suggestive FDG-PET or SPECT: Decreased brain activity in parietal and temporal regions.
- CSF Biomarkers (FDA-approved): Decreased (beta-amyloid) AB42 and increased tau and phosphorylated tau.
- Normal AB42 has good negative predictive value.
Mild Alzheimer Disease
- Non-pharmacologic:
- Exercise.
- Heart healthy diet.
- Treat sleep disorders.
- Statins are indicated for CHD, but cases of cognitive decline on initiating statins have been widely reported.
- 1st therapy acetylcholinesterase inhibitors:
- Donepezil.
- Rivastigmine.
- Galantamine.
- Avoid class if cardiac conduction abnormalities.
- Avoid donepezil in patients with seizures.
- GI SE result in discontinuation in 20% of patients; also syncope, agitation, dizziness, vivid dreams, nocturnal cramps.
- Patients may have mild-moderate slowing of progression
- On the horizon: Special note on Aducanumab.
- Aducanumab was approved by the FDA in June, 2021 initially with a broad indication for the diagnosis of Alzheimer’s Disease but soon the indication was narrowed to patients with MCI (mild cognitive impairment) or early Alzheimer’s Disease. The drug is a monoclonal antibody targeting amyloid deposition in the brain. The approval was based on a surrogate biomarker, improvement in amyloid PET scans. Clinical improvement in two phase III trials was minimal on one trial and none in the second. There has been widespread controversy about the use of this drug.). Initial cost was $56K/yr, now reduced to $26K/year. The role of this drug in treating Alzheimer’s Disease remains unclear.
Moderate/Severe Alzheimer Disease
-
NMDA-receptor antagonist (N-methyl-D-aspartate) memantine.
- Must have significant functional impairment.
- Combination with acetylcholinesterase inhibitor is used in some patients.
- Families often need caregiving support.
- Language-variant and Behavioral-variant—2nd most common cause in patients < 65 yo—key feature change in behavior.
- Behavioral/Functional impairment > cognitive impairment—often misdiagnosed as having obsessive compulsive, bipolar, etc. Impulsive/excessive behaviors.
- Family history of autosomal dominant in 10%, general dementia FH in ~40%; ALS (behavior-variant) may co-occur in ~25%.
- CT or MRI needed to distinguish from frontal lobe lesions.
- CSF usually distinguishes from AD: Normal AB42.
- No currently approved therapies; symptomatic tx. Monitor for ALS.
- Chronic Traumatic Encephalopathy (CTE): Repeated head trauma.
- Dementia with Lewy bodies: Associated with Parkinson Disease (second most common form of dementia; labeled DLB if dementia occurs within 1–2 years of PD symptom onset). ⍺-synuclein deposits (Lewy bodies). Delusions and hallucinations more common, may progress rapidly.
- Normal pressure hydrocephalus: Gait changes (wide gait, hesitation, and short steps), urinary incontinence and dementia. CT/MRI shows ventriculomegaly. Treatment is shunting.
- Vascular cognitive impairment: Diffuse vascular dz; gait impairment and pseudobulbar affect (emotional incontinence); MRI can show diffuse white matter hyperdensity.
- Rapidly progressive dementia: Consider Creutzfeld-Jacob (CJD), paraneoplastic, lupus, Sjogren, sarcoidosis, and a long list of others.
Note
NPH is a clinical triad of gait disorder, urinary incontinence, and sub-acute dementia. Radiology only confirms the diagnosis.
Image credits
Unless otherwise noted, images are from Adobe Stock.