- Self-study learning goals
- Describe the normal right and left atrial anatomy.
- Describe the pathophysiology of right atrial abnormality.
- Identify right atrial abnormality on the EKG.
- Describe the pathophysioogy of left atrial abnormality.
- Identify left atrial abnormality on the EKG.
- Describe the association of atrial abnormalities with valvular heart disease.
Atrial abnormalities: Anatomy
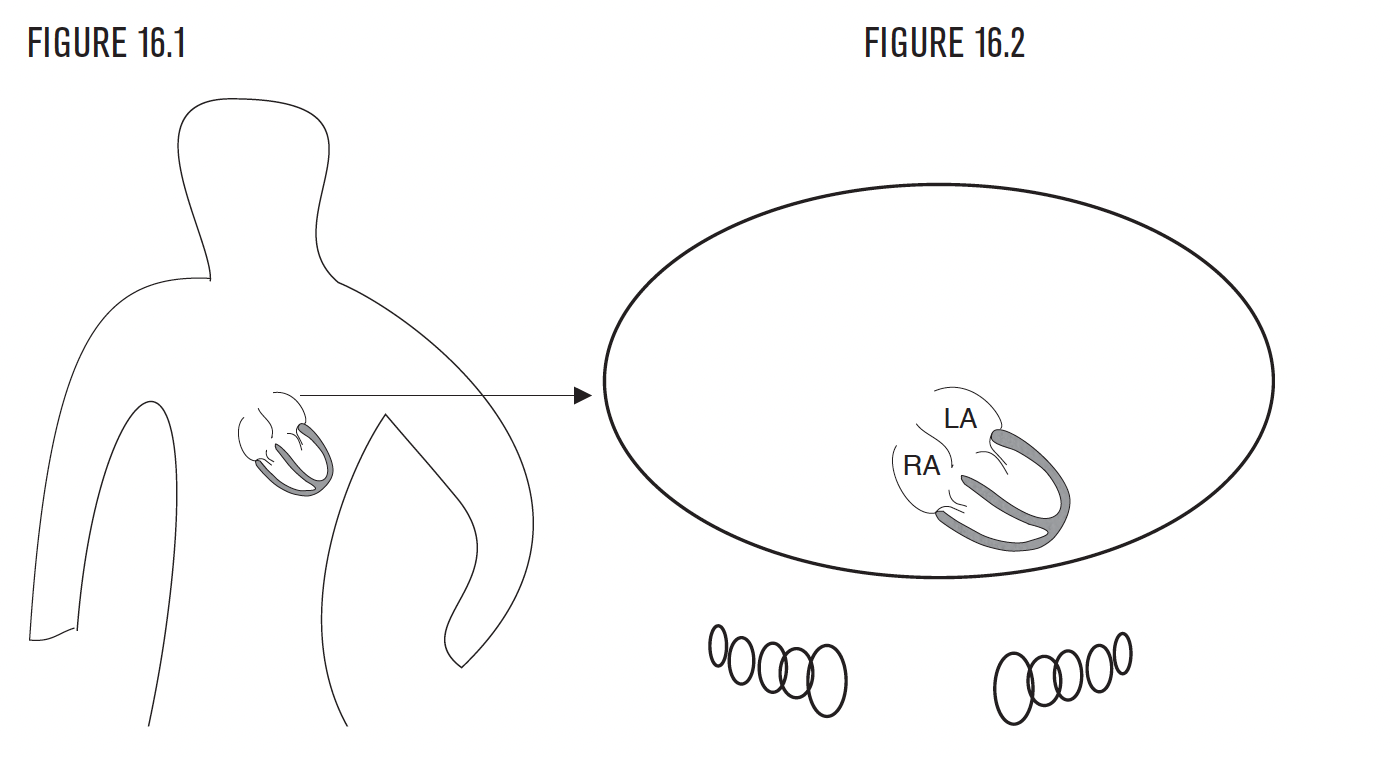
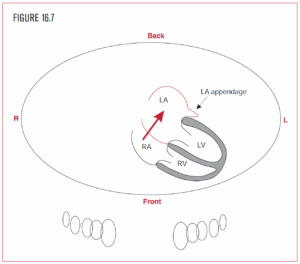
The right atrium (RA) is rightward and anterior. The left atrium (LA) is leftward and posterior. The P wave represents atrial depolarization. Analysis and visualization of the P wave identify atrial abnormalities, or enlargement. Both right atrial abnormality (RAA) and left atrial abnormality (LAA) can be distinguished.
Right atrial abnormality
- Pathophysiology
- EKG diagnosis
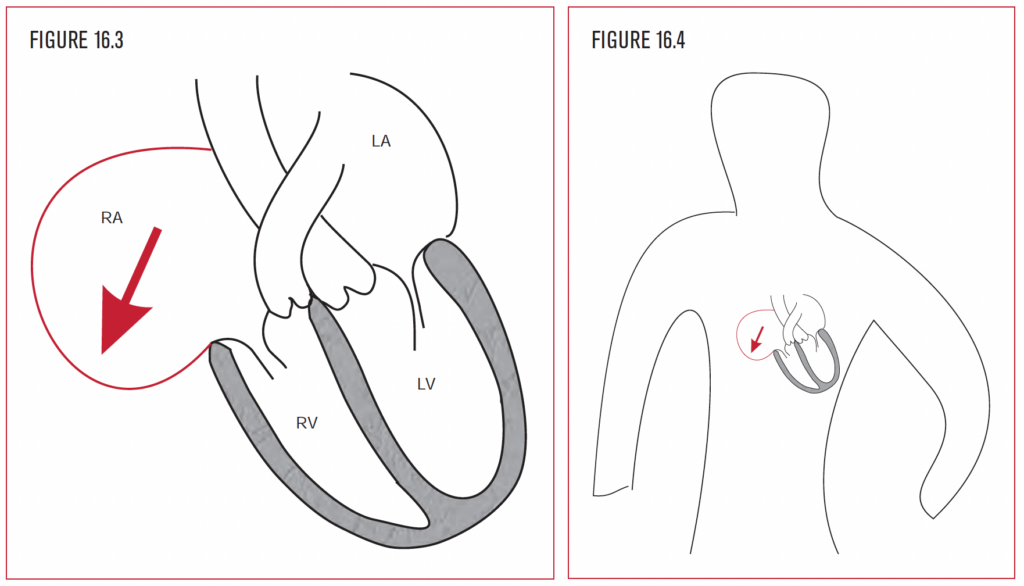
The right atrium is to the right and in front of the left atrium. In fact, the right atrium is the most rightward chamber of the heart. As the right atrium is subjected to the stress of either an increased pressure load or increased volume load, it enlarges as a compensatory mechanism to handle the increased work. Increased pressure in the right ventricle can be present from pulmonary hypertension secondary to chronic obstructive lung disease or pulmonary embolism. To handle the stiff muscular right ventricle, the right atrium has to “bulk up” in response. Increased volume in the right atrium can result from tricuspid regurgitation, commonly seen after pacemaker implantation, or because of long-standing pulmonary hypertension. To handle the volume overload, the right atrium has to “make space,” and so it dilates.
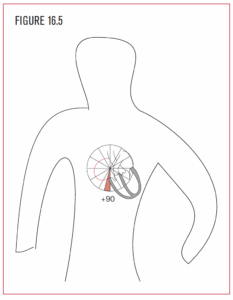
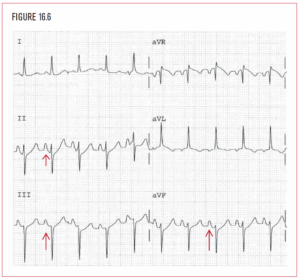
RAA can be diagnosed by an increase in the P wave amplitude to 2.5 little boxes in leads II, III, and AVF. RAA can also be diagnosed by a change in the P wave axis to a rightward direction. Right atrial abnormality on the EKG identifies enlargement in cavity size or muscle mass of the right atrium. Enlargement (bigger chamber) or hypertrophy (thicker walls) of the right atrium can change the P axis to a rightward direction. It can also increase the amplitude of the P wave.
A normal range for the P wave direction in the frontal plane is usually to the patient’s left and inferior, although anywhere from −30° to +75° may be normal. Visualization of the normal P wave should point in this range. A P wave direction of +90° to +105° or more indicates right atrial abnormality (RAA).
Left atrial abnormality
- Pathophysiology
- EKG diagnosis
The left atrium is located behind the right atrium. In fact, the left atrium is the most posterior chamber of the heart. As the left atrium is subjected to the stress of pressure or volume, it enlarges as a compensatory mechanism to handle the increased work. Increased pressure in the left ventricle can be present from hypertension, aortic stenosis, or hypertrophic obstructive cardiomyopathy. To handle the stiff muscular left ventricle, the left atrium has to “bulk up” in response. Increased pressure in the left atrium can directly result from mitral stenosis.
Increased volume in the left atrium can result from mitral regurgitation. To handle the volume overload, the left atrium has to “make space,” and so it dilates. The small pouch-like sack attached to the left atrium is called the left atrial appendage. It is a critical structure clinically because it can harbor thrombus formation in low flow states, such as atrial fibrillation. Part of the thrombus can fragment and embolize to the systemic circulation, where it can cause stroke, bowel infarction, or limb embolus. Left atrial abnormality is a tiny part of the EKG that provides important clinical clues about disease on the left side of the heart.
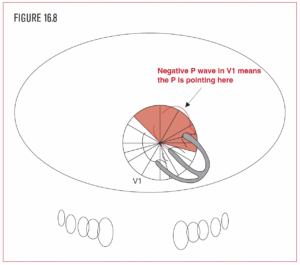
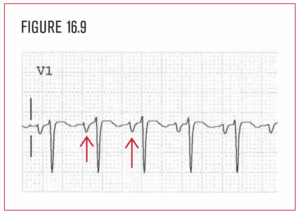
The direction of normal left atrial depolarization is posterior. The atrial depolarization force is represented on the EKG by the P wave. An increase in left atrial mass will increase the left atrium component of the P wave. Lead V1 is usually the best lead for determining whether the left atrium is enlarged. A left atrial abnormality creates a visible negative part to the P wave in V1. Since the left atrium is farther away from the sinus node than the right atrium, the second half of the P wave usually represents the left atrial component. In LAA, the P wave in V1 is negative by at least 1 little box. The negative part of the P wave in V1 must also be 1 little box wide (0.04 seconds) (Figure 16.9).
Valvular heart disease
Diseased or malfunctioning heart valves cause increased burdens on the atria and ventricles (either volume or pressure) that can produce suggestive EKG changes. When valves leak (regurgitate) or become narrowed (stenose), they put a strain on at least one of the four chambers of the heart. This strain leads to increased mass of the involved chamber, as it tries to adapt to the added workload. The increased mass of any cardiac chamber creates a larger electrical force on the EKG, and this is how we detect hypertrophy of any of the heart chambers.
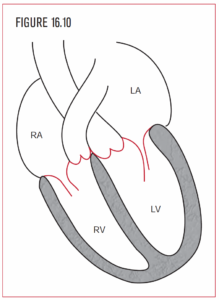 Regurgitation typically causes an added burden in the form of extra volume, which requires more space. The involved chambers of the heart respond by dilatation. This adaptation works well to offset the volume overload of regurgitation, as long as it develops slowly.
Regurgitation typically causes an added burden in the form of extra volume, which requires more space. The involved chambers of the heart respond by dilatation. This adaptation works well to offset the volume overload of regurgitation, as long as it develops slowly.
Stenosis is quite a different matter. It creates an added burden in the form of increased resistance to flow, which requires pressure-generating ability. The involved chambers behind the stenosis typically develop thicker walls.
In the adult, the four most common valvular heart diseases that cause abnormalities on the EKG are mitral stenosis, mitral regurgitation, aortic regurgitation, and aortic stenosis.