- Self-study learning goals
- Define and identify the associated EKG changes for:
- Pneumothorax.
- Pleural effusion.
- Dextrocardia.
- Pericardial effusion.
- Infiltrative cardiomyopathy.
- Pericarditis.
- Dilated cardiomyopathy.
- Hypertrophic cardiomyopathy.
- Chronic obstructive lung disease (COPD).
- Athlete’s heart.
- Describe possible EKG changes associated with:
- Postoperative patients.
- Cancer patients.
Overview
The electrocardiogram (EKG) not only provides valuable information on the electrical events of the heart, but it can also be useful in the diagnosis of medical and surgical conditions that affect the heart.
Clinical conditions
Low voltage
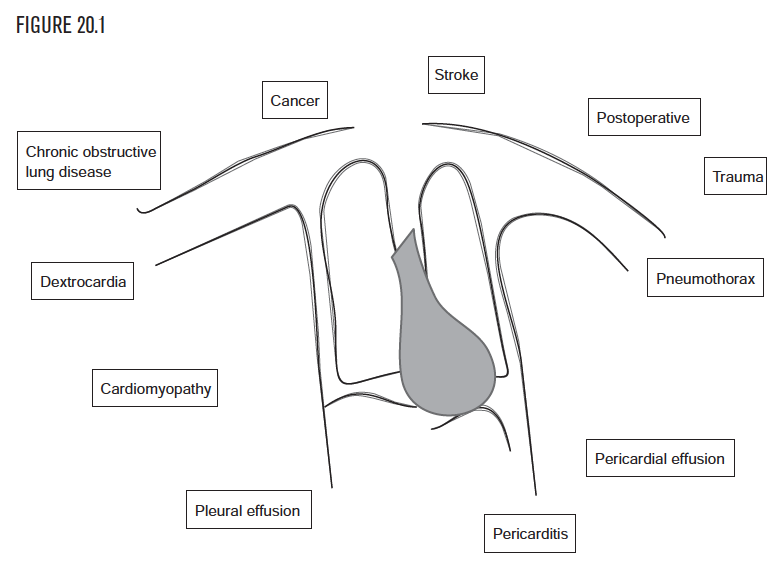
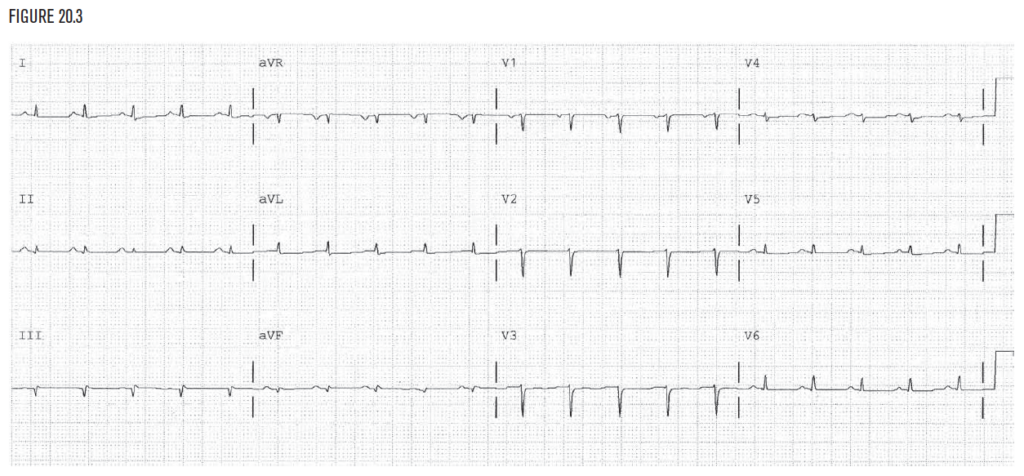
The heart lies in the chest in the mediastinum, slightly to the left of the midline. There are certain diseases and conditions that alter the normal anatomy of the chest cavity and can cause changes in the EKG.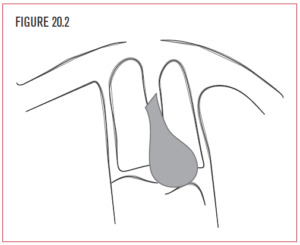 When the changes in anatomy interfere with the ability of the EKG leads to take normal measurements, a condition called low voltage can occur (Figure 20.3).
When the changes in anatomy interfere with the ability of the EKG leads to take normal measurements, a condition called low voltage can occur (Figure 20.3).
Low voltage is present in the frontal plane if the sum of the QRS amplitudes in leads I, II, and III (ie, I + II + III) is less than 15 little boxes. Similarly, low voltage is present in the horizontal plane if the QRS amplitude does not reach 15 little boxes in at least one of leads V1, V2, or V3. Some examples of this are pneumothorax, large pleural effusion, obstructive lung disease, infiltrative cardiomyopathies, and dextrocardia.
Pericarditis
Disorders of the pericardium can also produce specific changes in the EKG without causing a large collection of fluid and without causing low voltage. Pericarditis occurs when the pericardium becomes inflamed. Although the cause of pericarditis is not fully understood, it is associated with other disease processes, such as connective tissue disorders and infection. The inflammation of the pericardium can directly injure the underlying myocardium and mimic ischemia on the EKG. Sinus tachycardia may be present.
Cardiomyopathy
- Dilated
- Hypertrophic
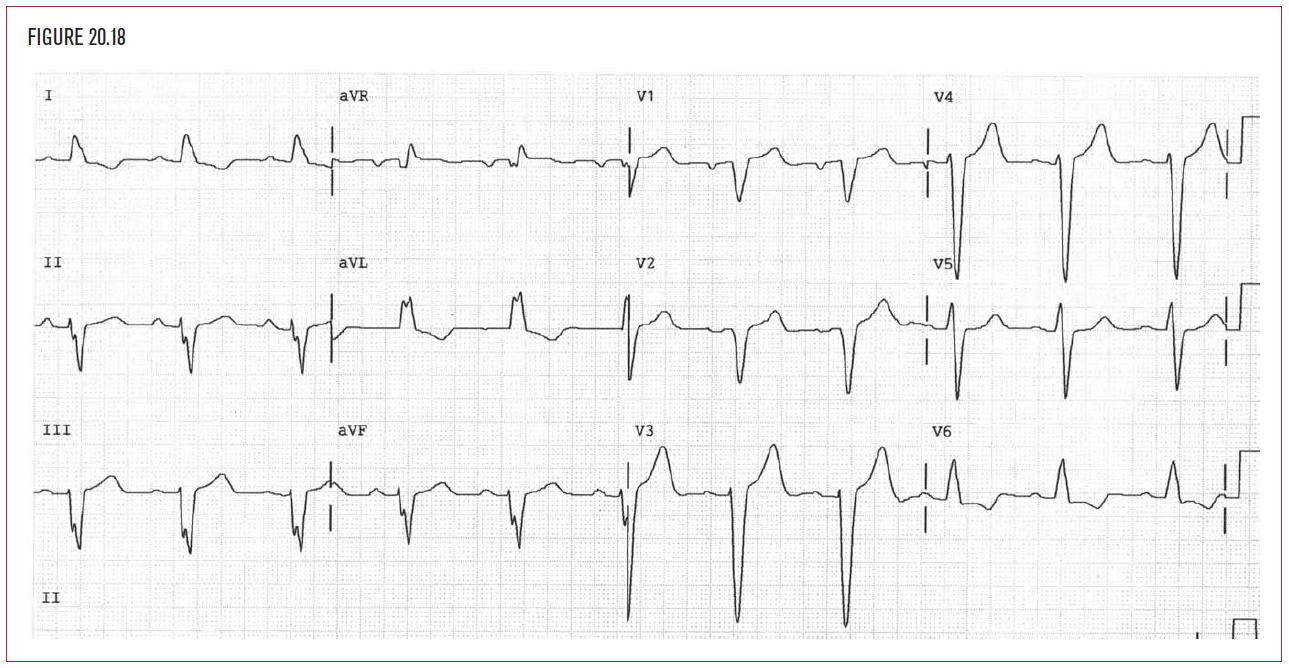
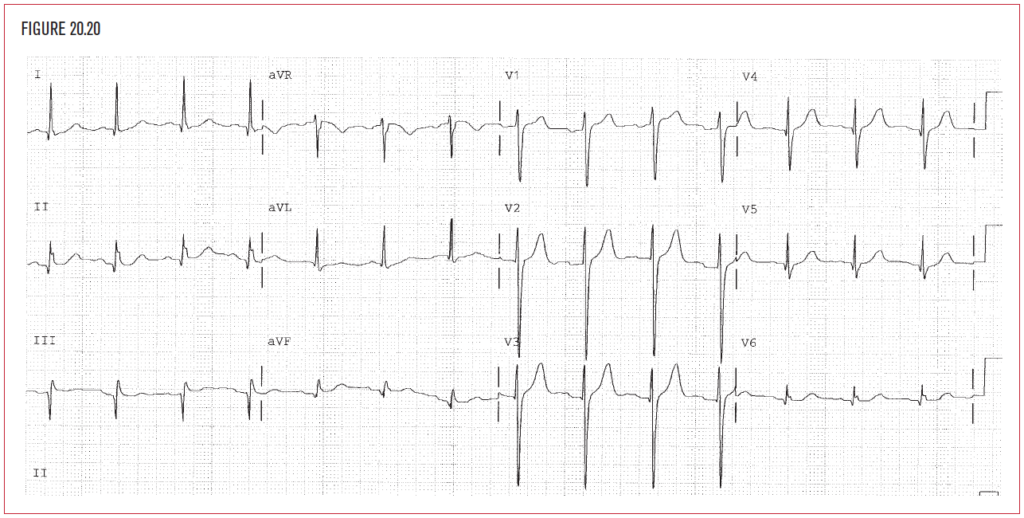
The EKG demonstrates abnormalities in many of the cardiomyopathies. Dilated cardiomyopathy is the diagnostic term used to describe a dilated and diffusely weakened heart muscle.  Although in most cases the cause of cardiomyopathy is unknown, there are certain diseases, such as hypertension, viral infections, and alcoholism that may contribute to it. The EKG may demonstrate left bundle branch block (Figure 20.18). Left atrial abnormality is another helpful clue.
Although in most cases the cause of cardiomyopathy is unknown, there are certain diseases, such as hypertension, viral infections, and alcoholism that may contribute to it. The EKG may demonstrate left bundle branch block (Figure 20.18). Left atrial abnormality is another helpful clue.
Hypertrophic cardiomyopathy is associated with sudden death. This may include asymmetric hypertrophy of the ventricular septum, which produces increased voltage and criteria for LVH on the EKG. There may be dynamic outflow obstruction below the aortic valve as well. This is due to coaptation of the anterior mitral valve leaflet against the ventricular septum. This coaptation restricts the exit of blood from the left ventricle.
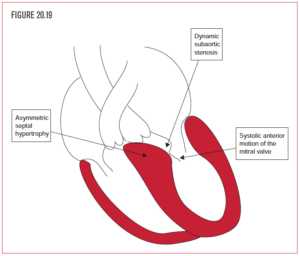 This drop in cardiac output can cause syncope, shock, or sudden death. The EKG typically shows increased voltage but no obvious universal pattern of changes has been described. The presence of EKG evidence of LVH without a history of hypertension should prompt a workup for other causes of LVH.
This drop in cardiac output can cause syncope, shock, or sudden death. The EKG typically shows increased voltage but no obvious universal pattern of changes has been described. The presence of EKG evidence of LVH without a history of hypertension should prompt a workup for other causes of LVH.
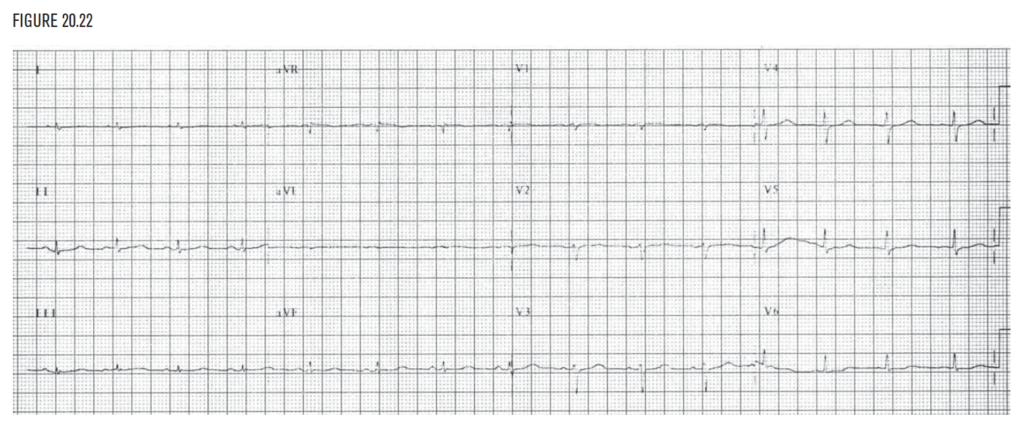
Chronic lung disease: Low voltage
COPD is a common disease and the most common cause of low voltage (Figure 20.22). Diseased airways trap excessive air in the lungs. Air is a poor conductor of electrical forces, and so the voltage of some or all leads on the EKG is lowered. Hypoxia or low oxygen level in the blood is another frequent cause of sinus tachycardia, when moderate or when the patient is treated with sympathetic agonists, or sinus bradycardia, when profound. All patients on ventilator support or those with chronic lung disease who develop sudden bradycardia should be evaluated immediately for hypoxia.
Athlete’s heart
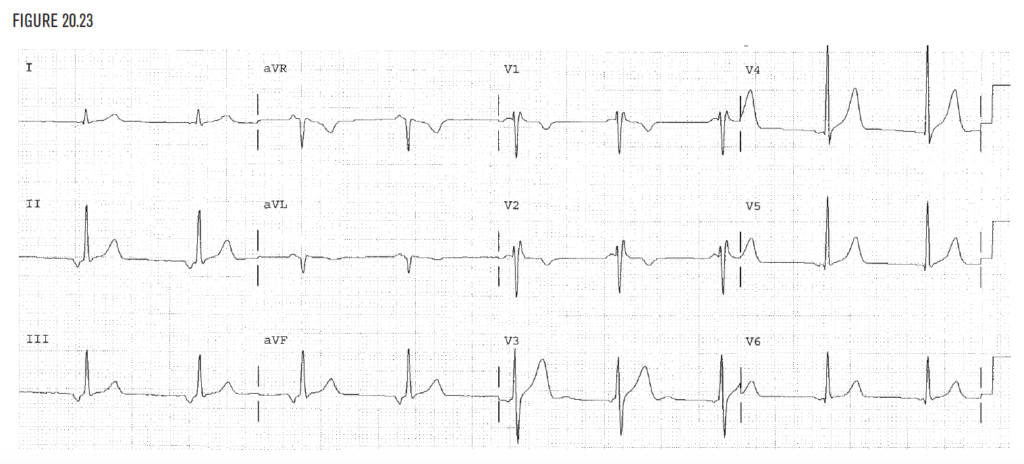
The evaluation of the athlete’s heart is always challenging for the clinician. Many of the EKG changes and dysrhythmias associated with an athlete’s heart could represent a pathologic process in an average individual, but they are often considered normal for the well-conditioned person.
Examples of dysrhythmias often experienced by an athlete:
- Sinus bradycardia.
- Sinus arrhythmia.
- Sinus pause.
- Escape beats.
- Various AV blocks.
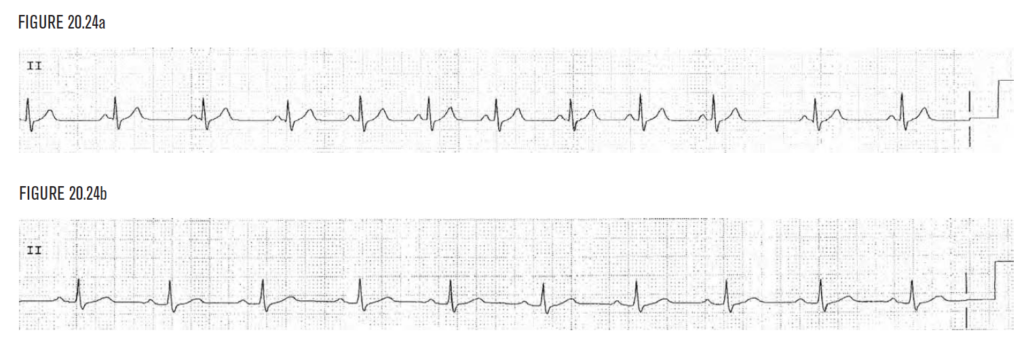
On the EKG, changes in the P wave and QRS complex are also common. Increased P wave voltage representing left or right atrial enlargement and increased QRS voltage representing right ventricular hypertrophy (RVH) or LVH are often seen. Figure 20.23 demonstrates junctional rhythm and right intraventricular conduction delay (RSR in V1). Figure 20.24a demonstrates sinus arrhythmia. Figure 20.24b demonstrates 1° AV block.