In this material
- Self-study learning goals
- Define and Identify the following:
- Normal QRS interval.
- Normal QRS direction.
- Define the two EKG criteria for LBBB.
- Define the pathophysiology of left bundle branch block.
- Describe how LBBB causes desynchronization.
- Describe how desynchronization hurts LV function.
- Describe resynchronization.
- Describe the differential diagnosis of etiologies LBBB.
Normal physiology of QRS formation
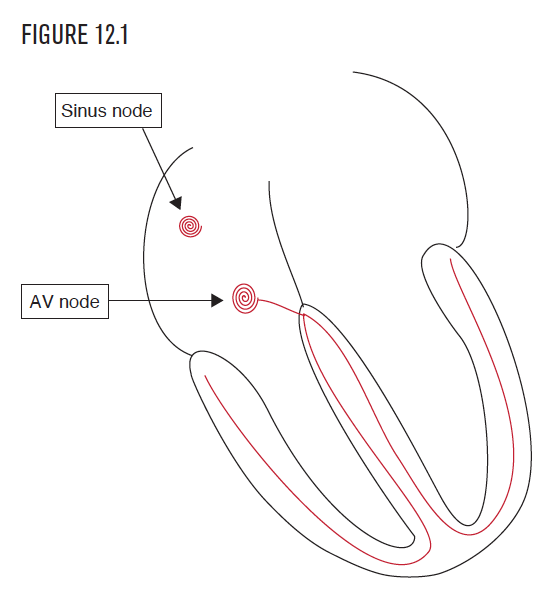
The heart has specialized cells that enable the five critical electrical and mechanical functions. The sinus node established the first of the five critical functions—the ability to create an automatic and regular heart rhythm. The AV node established the second critical function—the ability to delay and then conduct the electrical impulse between the atrium and the ventricle. The right and left bundles provide the third function—communication of the impulse to billions of cells in the right and left ventricles to provide for nearly simultaneous activation of both ventricles.
Normal QRS formation
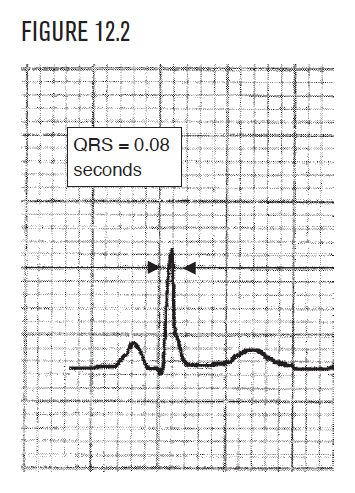
The right and left bundles (Figure 12.1) form an exquisitely capable communication system. They carefully navigate the impulse and depolarize every single one of the hundreds of millions of ventricular cells. This depolarization of the right and left ventricles forms the normal QRS with a normal interval of 0.08 (Figure 12.2).
Normal QRS physiology visualized: Frontal plane
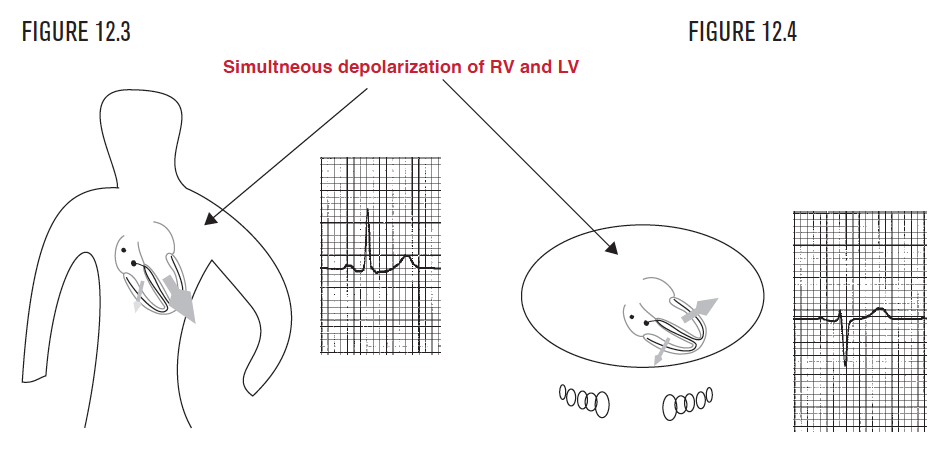
The normal QRS complex represents combined depolarization of all the right and left ventricular cells (Figure 12.2). This normally happens, from first cell to last, in 0.08 seconds. The message to depolarize is conducted to both the right ventricle and left ventricle. The normal direction of the QRS (as was discussed in Chapter 6 and Chapter 11) is toward the left ventricle apex, inferiorly and to the left. This is because the left ventricle has more mass than the right ventricle. This bigger mass creates a bigger electrical force on the EKG than the smaller right ventricle.
Both ventricles normally depolarize at the same time, and so the left ventricular component of the total electrical force overshadows the much smaller right ventricular force. In the frontal view, the QRS points to the patient’s left side, which is upward in lead I. In the horizontal view (from above), the direction of the QRS points posteriorly, which is negative in lead V2.
Left bundle branch block
- Pathophysiology
- EKG in the frontal plane
- EKG in the horizontal plane
- Criteria
- Abnormal ST segments
- Clinical associations
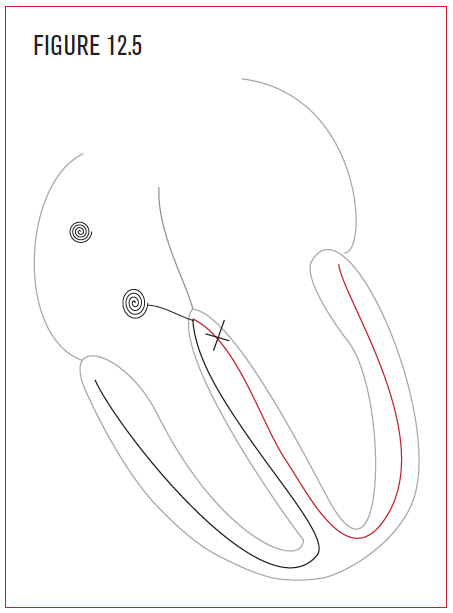
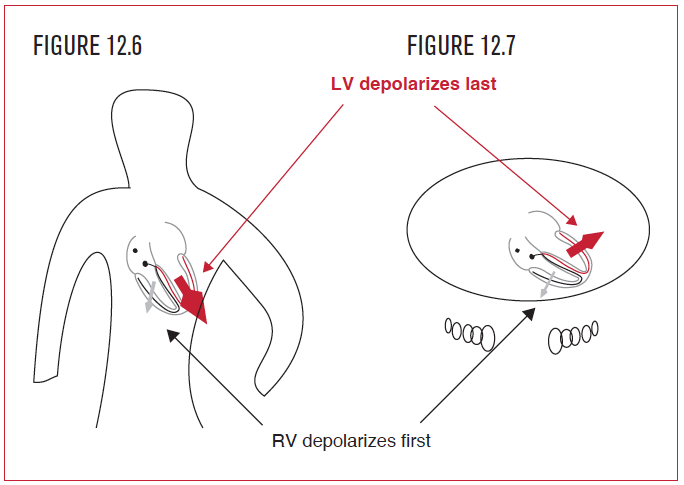
- Cardiac desynchronization
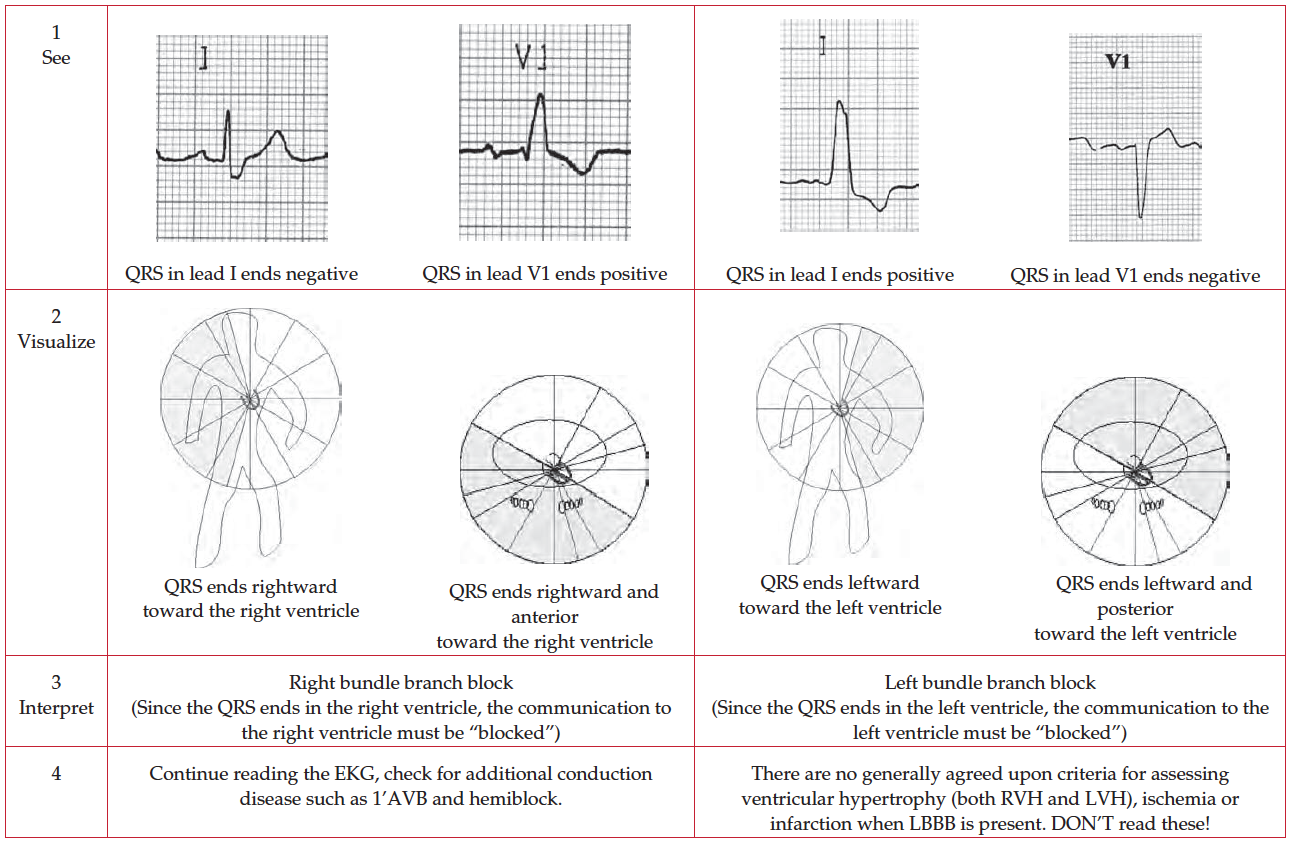
In left bundle branch block (Figure 12.5), this all changes. The ventricles are not depolarized at the same time, but in sequence—first the right ventricle, then the left. The sequence begins with the right bundle, since it is functioning normally. It depolarizes the whole right ventricle in the normal amount of time, which is less than 0.08 seconds.
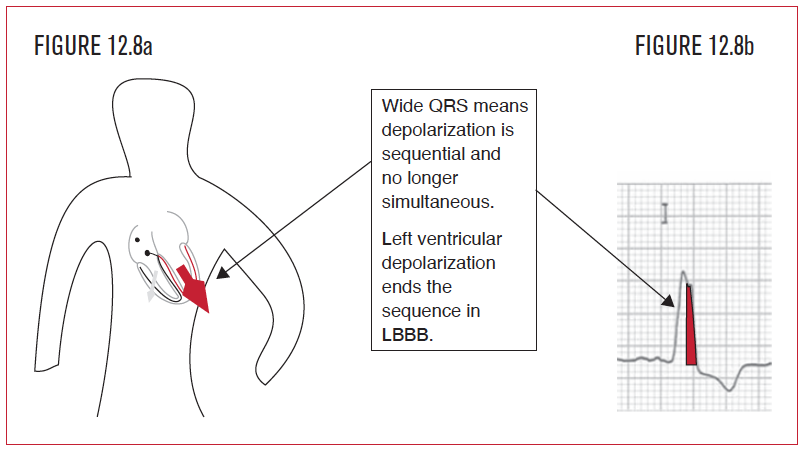
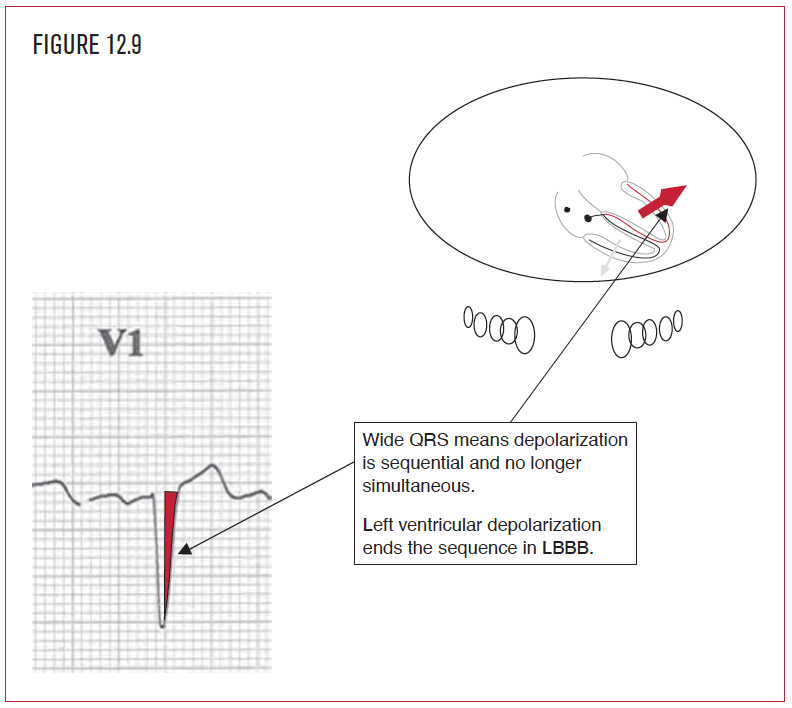
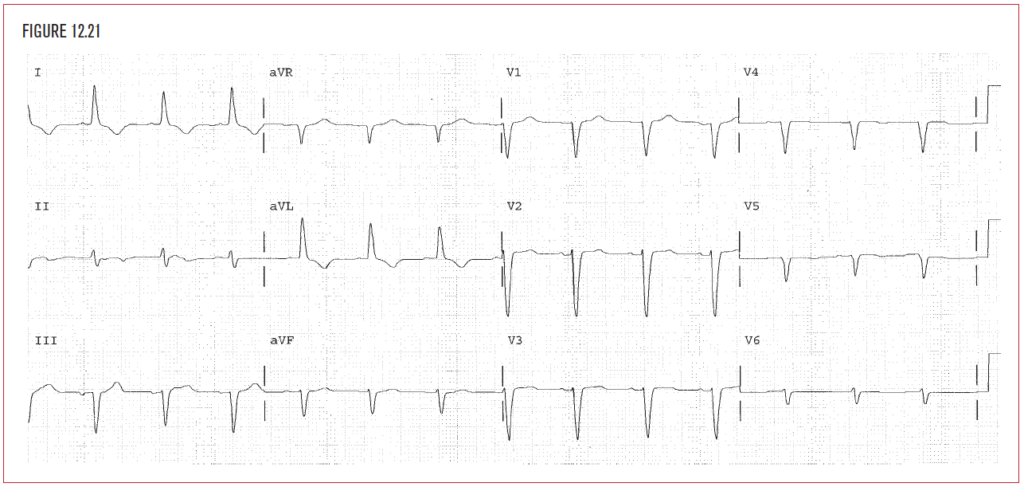
The rest of the QRS after that first 0.08 seconds represents only left ventricular activation. This is the second part of the sequence, depolarization of the left ventricle from the efforts of the right bundle. Since the depolarization of both ventricles is not simultaneous but sequential, it takes 50% longer to finish compared with the normal QRS of 0.08 seconds. Prolongation of the QRS interval to 0.12 seconds or more is the diagnostic signature of bundle branch block. This sequential depolarization allows for the second hallmark of LBBB, namely, that the last part of the depolarization sequence (the QRS) must be left ventricular in direction. In LBBB, ventricular activation ends late and on the left side, so the QRS ends in the left ventricle, a direction that is toward the patient’s left side and posterior.
Prolongation of the QRS interval to 0.12 seconds or more is the diagnostic signature of bundle branch block. This sequential depolarization allows for the second hallmark of LBBB, namely, that the last part of the depolarization sequence (the QRS) must be left ventricular in direction. In LBBB, ventricular activation ends late and on the left side, so the QRS ends in the left ventricle, a direction that is toward the patient’s left side and posterior.
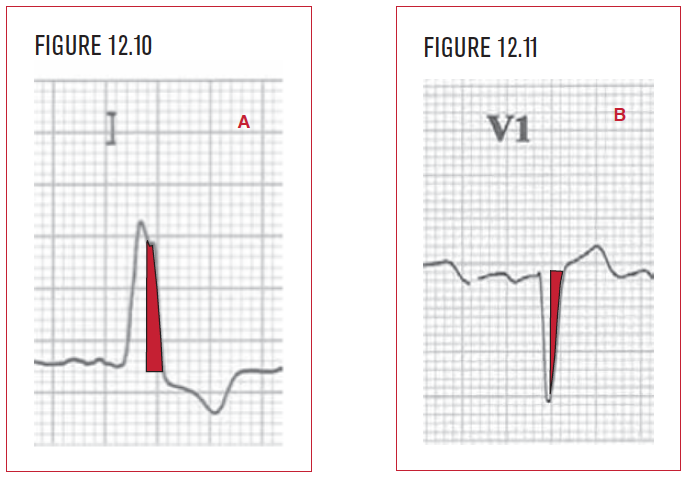
When the QRS interval is 0.12 seconds or more, bundle branch block is present. Visualize the direction of the end of the QRS. If it points to the left ventricle, then LBBB is present. In the frontal plane view (Figure 12.8a), the last part of the sequence emanates from the left ventricle and points to the patient’s left. Visualize the direction of the end of the QRS in lead I. Since it is positive, it points toward the left.
Prolongation of the QRS interval to 0.12 seconds or more is the diagnostic signature of bundle branch block. This sequential depolarization allows for the second hallmark of LBBB, namely that the last part of the depolarization sequence (the QRS) must be left ventricular in direction. In LBBB, the right bundle finishes off ventricular activation on the left side, so the QRS ends in the left ventricle, a direction that is toward the patient’s left side and posterior.
When the QRS interval is 0.12 seconds or more, bundle branch block is present. Visualize the direction of the end of the QRS in the horizontal plane. If it points to the left ventricle, then LBBB is present.
- The QRS interval is 0.12 seconds or longer.
- The last part of the QRS is moving toward the left ventricle, which is left and posterior.
-
- Limb Leads: The QRS ends in a positive wave (R or R’) in lead I, and in V6. This is a leftward direction.
- Horizontal Leads: The QRS ends in a negative (Q or QS) wave in lead V1. This is a posterior and leftward direction.
Critical Point: The first half of the QRS is irrelevant in making the diagnosis of LBBB!
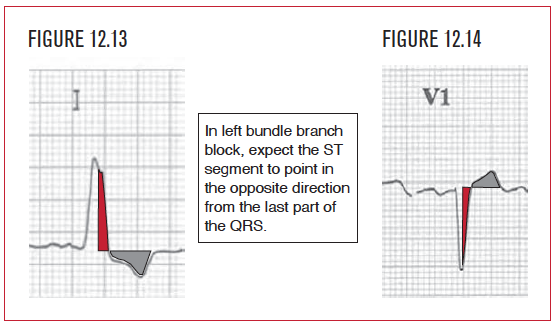
In LBBB, the ST segment is predictably abnormal and points away from the left ventricle. In Figure 12.13, the last part of the QRS is positive in lead I, so the ST segment should point away from this, or manifest ST segment depression in that lead. In lead V1 (Figure 12.14), the last part of the QRS is negative, so the ST segment should point away from that, or manifest ST segment elevation. In LBBB, the formation of the QRS is so abnormal that none of the criteria for analyzing the QRS, ST segment, or T wave are particularly useful. Therefore, in LBBB, do not describe any further abnormalities! When LBBB is present, stop further EKG analysis. Do not diagnose hemiblock, infarction, ischemia, or hypertrophy.
There are five common classes of clinical associations in LBBB.
- Coronary artery disease.
- Pressure overload.
-
- Hypertension.
- Aortic stenosis.
- Hypertrophic cardiomyopathy.
- Volume overload.
-
- Mitral regurgitation.
- Aortic regurgitation.
- Dilated cardiomyopathy.
- Primary disease of the conduction system.
When the ventricles lose coordination in either direction or timing of contraction between parts of the left ventricle or between the left and right ventricles, desynchronization is present. Desynchronization hurts overall cardiac function and can worsen symptoms of systolic and diastolic heart failure.  Figure 12.18 demonstrates a dilated cardiomyopathy. There are three ways that LBBB can hurt overall cardiac function in a patient with severe left ventricle dysfunction, as shown in Figure 12.19.
Figure 12.18 demonstrates a dilated cardiomyopathy. There are three ways that LBBB can hurt overall cardiac function in a patient with severe left ventricle dysfunction, as shown in Figure 12.19.
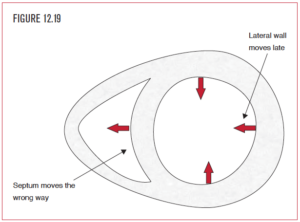
First, the septum is depolarized by the right bundle, and so contracts the wrong way, namely toward the RV. This means one of the four weak walls (the septum) is not only not helping, but is going the wrong way and subtracting from the other walls’ efforts. This is called a dyskinetic septum and can be diagnosed easily on echocardiography.
Second, the delay between the activation of the septum and the far away left ventricular lateral wall is prolonged by at least 50%. Thus, the lateral wall and septum do not contract simultaneously, but sequentially. This significantly reduces whatever mechanical effectiveness the weak left ventricle has remaining.
Third, the right ventricle depolarized normally and earlier, so blood is on the way from the right to the left ventricle before the left side is ready. The only place to put that blood is into the lungs, which leads to increased pulmonary congestion.
How resynchronization therapy works
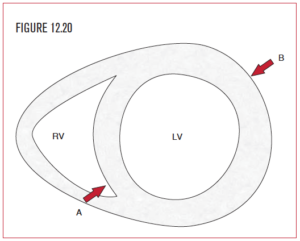 Resynchronization therapy is used in situations where both severe left ventricular systolic function and bundle branch block are present. Two pacing leads are used for the left ventricle. One is placed inside the right ventricle at the apex (A). The second is placed either in the coronary sinus or on the outside surface of the lateral wall of the left ventricle (B). This dual pacing (biventricular pacing) effect provides simultaneous depolarization of the left ventricle from two different sides and helps to provide a more synchronized effort for the weakened walls.
Resynchronization therapy is used in situations where both severe left ventricular systolic function and bundle branch block are present. Two pacing leads are used for the left ventricle. One is placed inside the right ventricle at the apex (A). The second is placed either in the coronary sinus or on the outside surface of the lateral wall of the left ventricle (B). This dual pacing (biventricular pacing) effect provides simultaneous depolarization of the left ventricle from two different sides and helps to provide a more synchronized effort for the weakened walls.
Mechanical contraction with a normal QRS
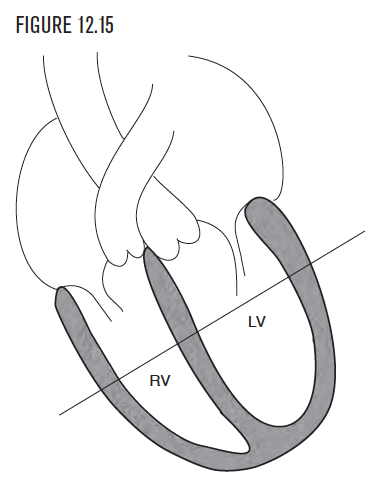
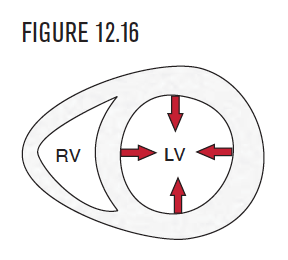
To visualize ventricular contraction with a normal QRS, it is easier to view a cross-section of the heart. Figure 12.15 demonstrates a four-chamber view of the heart. A line through the middle of this view produces Figure 12.16. This cross-sectional view is usually called a short axis view. You can easily recognize it because the LV looks like a donut, or car tire.
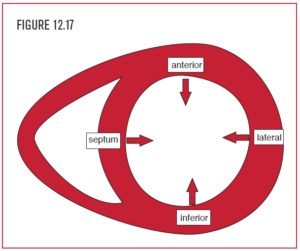 In a functioning ventricle with normal conduction, each of the four walls of the left ventricle (septum, anterior wall, lateral wall, and posterior wall) contracts normally and in synchronization toward the center of the left ventricular cavity. (In mechanical terms, the septum functions as an equal partner for the LV, not the RV.) This provides for normal cardiac systolic and diastolic function. In Figure 12.17, the patient has a severely dilated and hypokinetic left ventricle. Since the ventricle is so weak, it is very important for the four walls to contract in unison, however weak they are. With a normal QRS, the four walls of the left ventricle contract (however weakly) in the same direction, at the same time, and simultaneously with the right ventricle.
In a functioning ventricle with normal conduction, each of the four walls of the left ventricle (septum, anterior wall, lateral wall, and posterior wall) contracts normally and in synchronization toward the center of the left ventricular cavity. (In mechanical terms, the septum functions as an equal partner for the LV, not the RV.) This provides for normal cardiac systolic and diastolic function. In Figure 12.17, the patient has a severely dilated and hypokinetic left ventricle. Since the ventricle is so weak, it is very important for the four walls to contract in unison, however weak they are. With a normal QRS, the four walls of the left ventricle contract (however weakly) in the same direction, at the same time, and simultaneously with the right ventricle.
Incomplete left bundle branch
- Pathophysiology
Less than total loss of function in either the right or left bundle is called intraventricular conduction delay (IVCD) or incomplete LBBB. The primary diagnostic EKG abnormality in IVCD is prolongation of the QRS interval to 0.10 or 0.11 seconds. As in bundle branch block, IVCD may be left, right, or indeterminate. Once the QRS interval is measured at 0.10 or 0.11 seconds, it is the end of the QRS that is the key to diagnosis. If the end of the QRS is leftward (postive in lead I) and toward the left ventricle (negative in lead V1), then LIVCD is present.