- Self-study learning goals
- Identify the components of the conduction system.
- Identify the two parts of the left bundle.
- Describe the criteria for left anterior hemiblock.
- Describe the criteria for left posterior hemiblock.
- Identify left anterior hemiblock on the EKG.
- Identify left posterior hemiblock on the EKG.
Overview
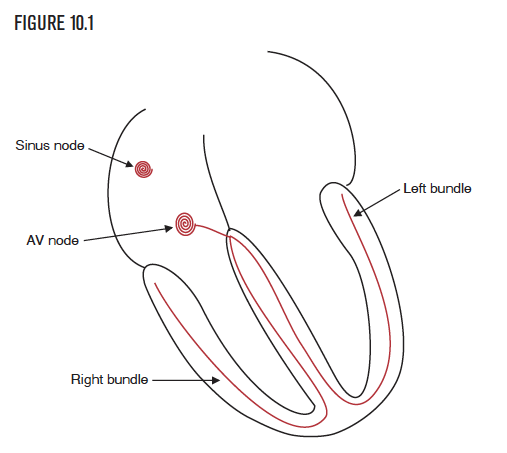
The heart has specialized cells that enable the five critical electrical and mechanical functions. The sinus node established the first of the five critical functions—the ability to create an automatic and regular heart rhythm. The second critical function allows for communication between hundreds of millions of cells in less than one or two tenths of a second. This conduction system is an exquisitely capable communication system. It carefully navigates the impulse from the atria through the normal AV node and the bundle of His, then through the right and left bundles and the Purkinje fibers, before finally depolarizing every single one of the millions of ventricular cells. The right and left bundles are directly responsible for conducting, or communicating, the electrical signal to all cells in both ventricles (Figure 10.1).
The left bundle branch
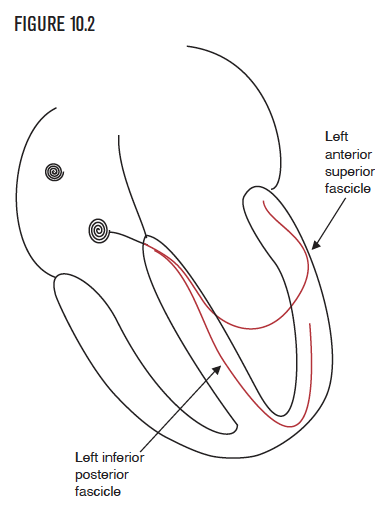
The left bundle has two parts (sometimes called fascicles) that help it communicate with the far greater number of cells in the left ventricle. The parts are called the anterior and posterior divisions, which are responsible for depolarization of the left ventricle, including the septum. Hemiblock is the loss of function in one of the two parts of the left bundle (Figure 10.2).
Left anterior hemiblock
- Pathophysiology
- Criteria
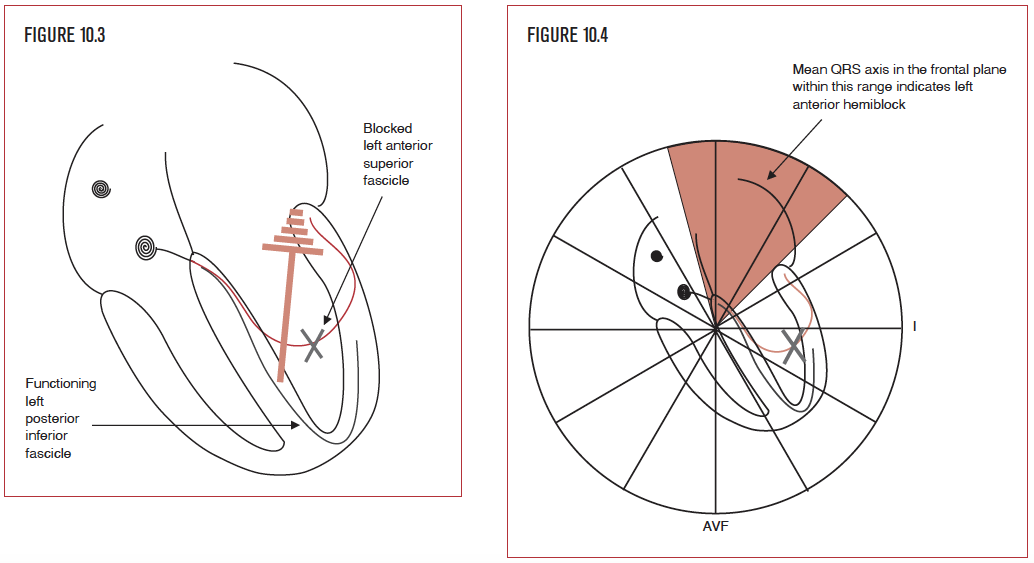
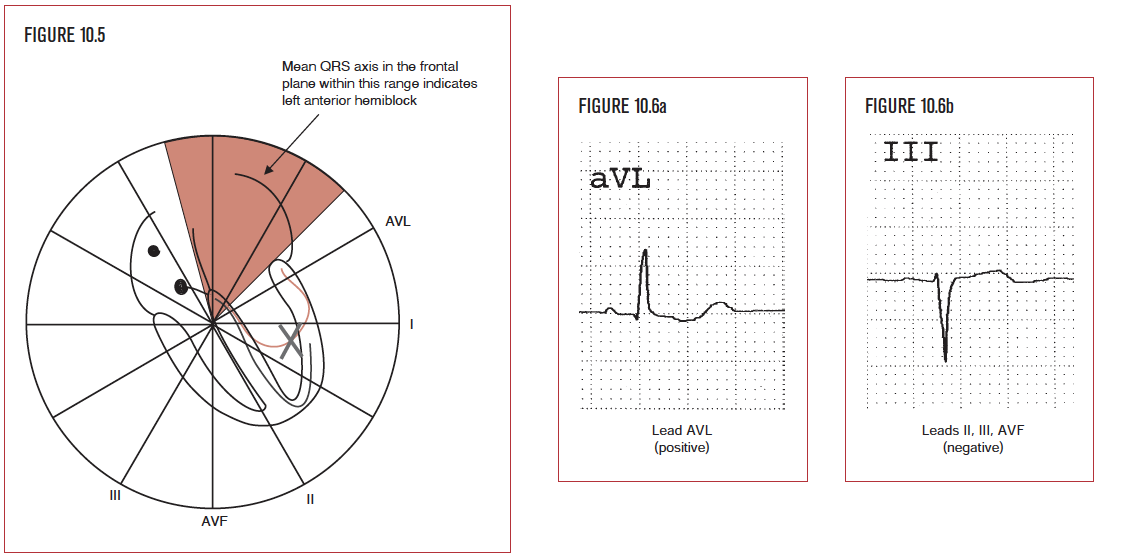
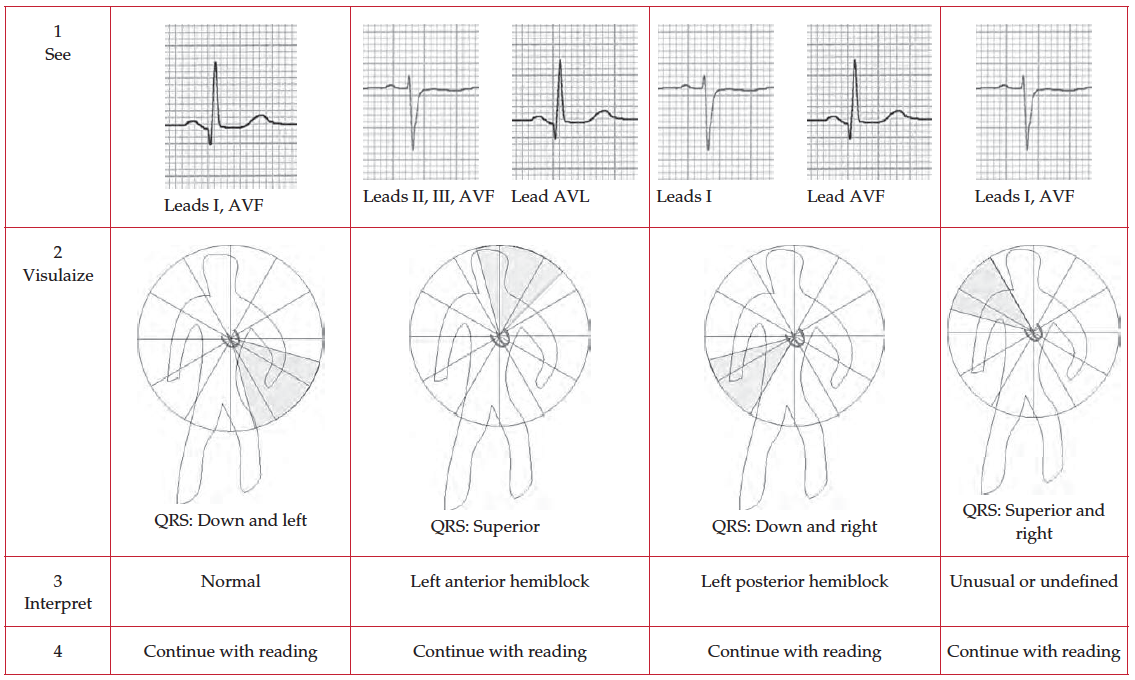
Left anterior hemiblock (LAHB) occurs when there is a loss of function in the anterior branch or fascicle of the left bundle branch (Figure 10.3). It is diagnosed by evaluating the mean QRS axis, or direction, in the frontal plane. The normal QRS direction is from the AV node toward the apex of the heart, that is inferiorly and to the patient’s left side. Left anterior hemiblock shifts the mean QRS axis upward and leftward (Figure 10.4). This occurs because the electrical impulse from the left inferior fascicle spreads superiorly and to the left to depolarize the entire left ventricle since the left anterior branch is unable to do so. Left anterior hemiblock is sometimes called left anterior superior hemiblock (LASH), which calls attention to the diagnostic trademark of LAHB, namely a superior QRS direction in the frontal plane. The two terms are synonymous. Of note, hemiblock does not significantly increase the duration of the QRS interval because each side of the heart has one functioning fascicle.
Left posterior hemiblock
- Pathophysiology
- Criteria
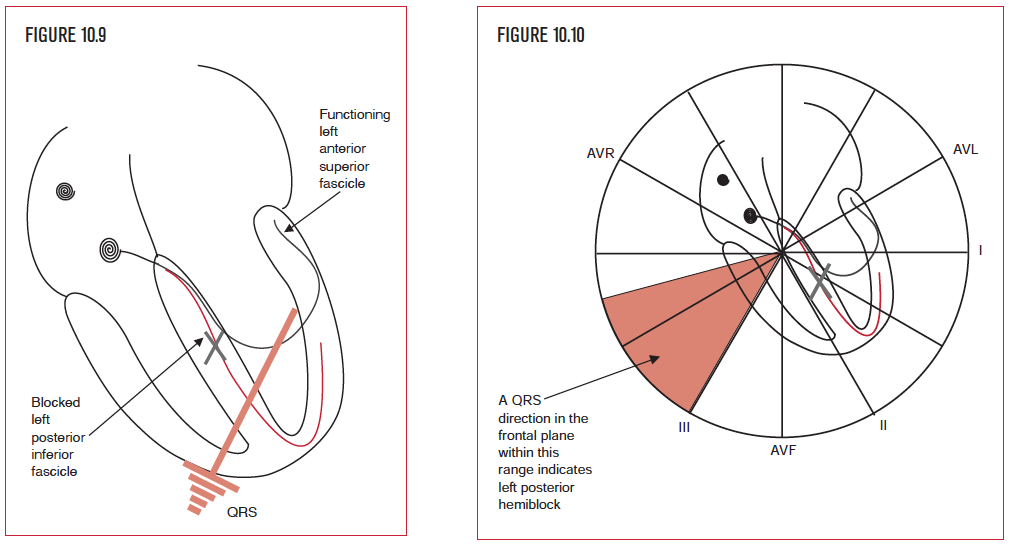
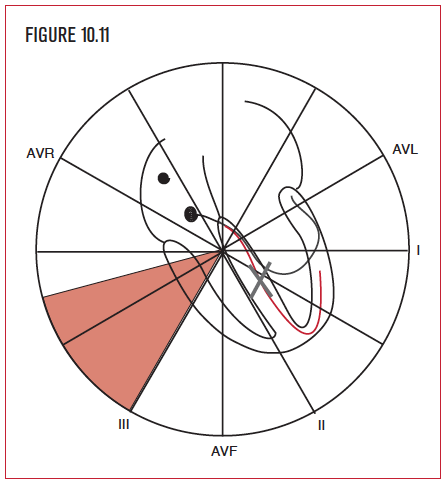
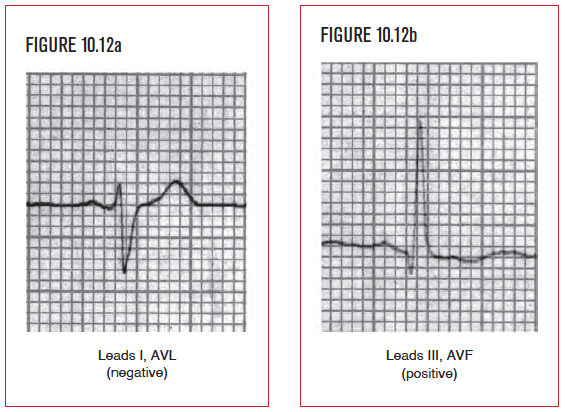
The second type of hemiblock is called left posterior hemiblock (LPHB). It occurs when there is a loss of function in the posterior part or fascicle of the left bundle branch. Like LAHB, it is diagnosed by evaluating the mean QRS axis or direction in the frontal plane. The normal QRS direction is from the AV node toward the apex of the heart, that is inferiorly and to the patient’s left side. Left posterior hemiblock shifts the mean QSR axis to the patient’s right side. This occurs because the electrical impulse from the left anterior fascicle spreads inferiorly and to the right to depolarize the entire left ventricle since the left posterior branch is unable to do so. Left posterior hemiblock is sometimes called left inferior posterior hemiblock (LIPH), which calls attention to the diagnostic trademark of LIPH, namely an inferior and rightward QRS direction in the frontal plane. The two terms are synonymous. Again, hemiblock does not significantly increase the duration of the QRS interval since each side of the heart has one functioning fascicle.