- Self-study learning goals
Define and identify the following:
- Junctional rhythm.
- 1° AV block.
- 2° AV block.
- Premature atrial contraction.
- Sinus arrest.
- Asystole.
- Complete heart block.
- Ventricular escape beats.
- Ventricular pacing.
- Atrial and ventricular sequential pacing.
- Atrial pacing.
Describe a clinical association or cause of:
- Junctional rhythm.
- 1° AV block.
- 2° AV block.
- Premature atrial contraction.
- Sinus arrest.
- Asystole.
- Complete heart block.
- Ventricular escape beats.
Describe a clinical use for:
- Ventricular pacing.
- Atrial and ventricular sequential pacing.
- Atrial pacing.
Junctional rhythm
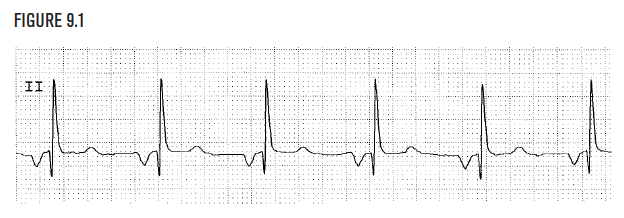
Junctional rhythm is a regular rhythm. A P wave is frequently not seen because the rhythm originates in the AV junctional node. When a P wave is seen, it may precede the QRS, as shown in Figure 9.1 When present, the P wave direction in junctional rhythm is upward. Junctional rhythm may be a manifestation of digitalis toxicity, sick sinus syndrome, and acute inferior wall infarction.
Heart block
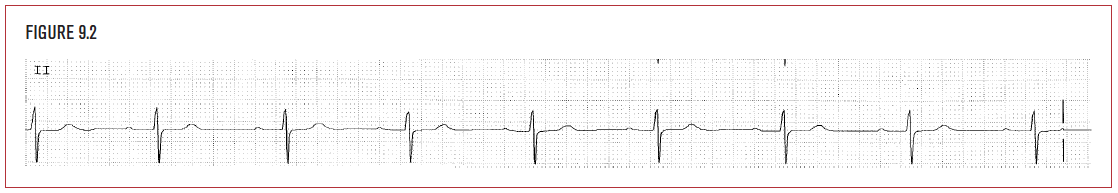
1° AV block is an abnormally long delay in the transmission of the atrial impulse through the AV node. It causes a prolongation of the PR interval to greater than 0.20 seconds. In Figure 9.2, the PR interval is 0.26 seconds long. Associations include sick sinus syndrome, drugs such as digitalis, calcium channel blockers, and antiarrhythmics.
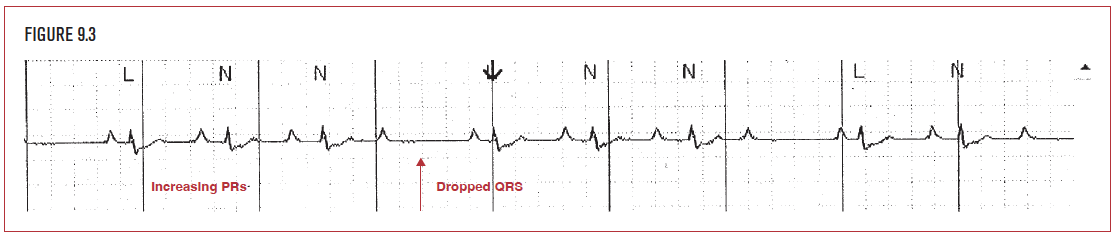
2° AV block is a more severe form of conduction abnormality in the AV node. It is characterized by a P wave that “gets lost” in the AV node and never generates a QRS complex on the EKG. There are two types of 2° AV block: Wenckebach (Type I) and Mobitz (Type II). Wenckebach is characterized by an increasing PR interval leading up to a dropped or nonconducted P wave, as shown in Figure 9.3. Because a grouping of 4 P waves leads to 3 QRS complexes, this is termed 4:3 Wenckebach. Type II (Mobitz) AV block is characterized by sequential P waves (usually more than two) that produce only a single QRS complex.
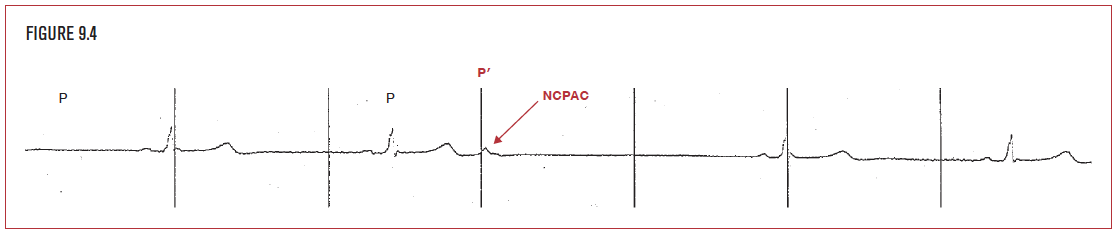
Pauses are most commonly caused by premature atrial contractions (PACs) that do not conduct down to the ventricle and generate a QRS complex. These are called nonconducted PACs (NCPACs). Frequently they occur during the T wave, and deform the T wave compared to normal. In Figure 9.4, the premature wave (P’) does not conduct to the ventricles and causes a pause of 2.6 seconds. Nonconducted PACs may be a sign of underlying conduction disease, such as sick sinus syndrome, particularly if they occur late in the cycle and are followed by a long pause.
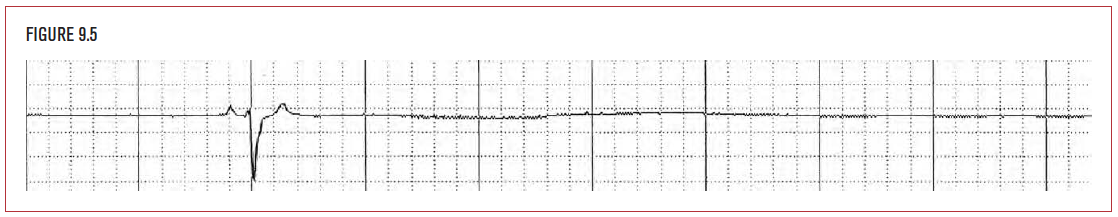
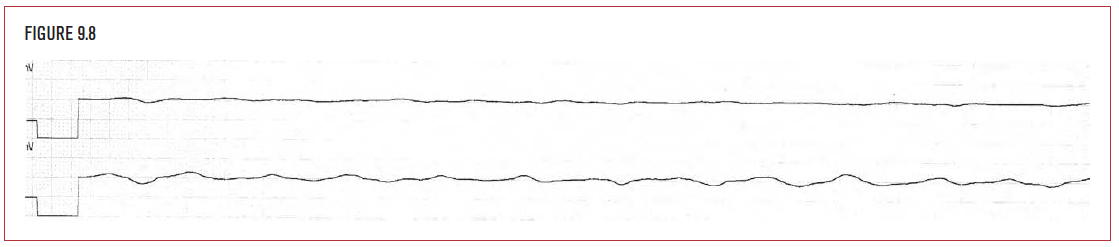
Asystole is a prolonged period of no electrical activity. In Figure 9.5, for example, a sinus beat is followed by a period of 8 seconds of electrical asystole that continues until the end of the strip. Cessastion of function of the sinus node is called sinus arrest. Normally, when sinus arrest occurs, another pacemaker must take over, such as the junction (usually at an escape rate of 40–60 bpm) or the ventricles (usually at an escape rate of 30 bpm). In Figure 9.5, however, there is sinus arrest with no further pacemaker activity anywhere. This leads to asystole and cardiac arrest.
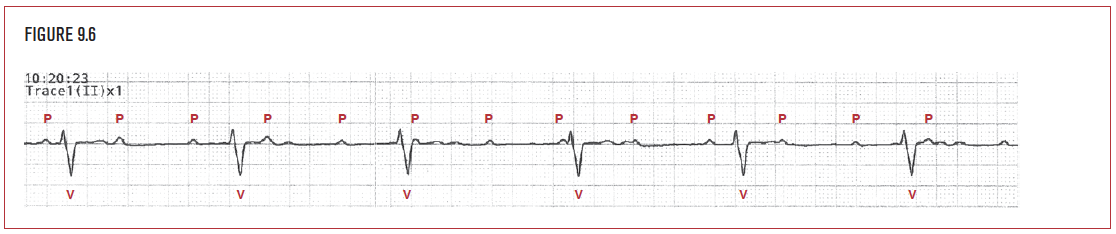
Complete heart block (CHB), also known as 3° AV block (3° AVB), describes the presence of atrial activity that does not conduct down to the ventricles on a continuing basis. Figure 9.6 demonstrates a patient with P waves (P) at a rate of 83 bpm. The P waves do not generate QRS complexes. A regular ventricular rhythm (V) at a rate of 36 bpm has come in as an escape to provide a heart beat.
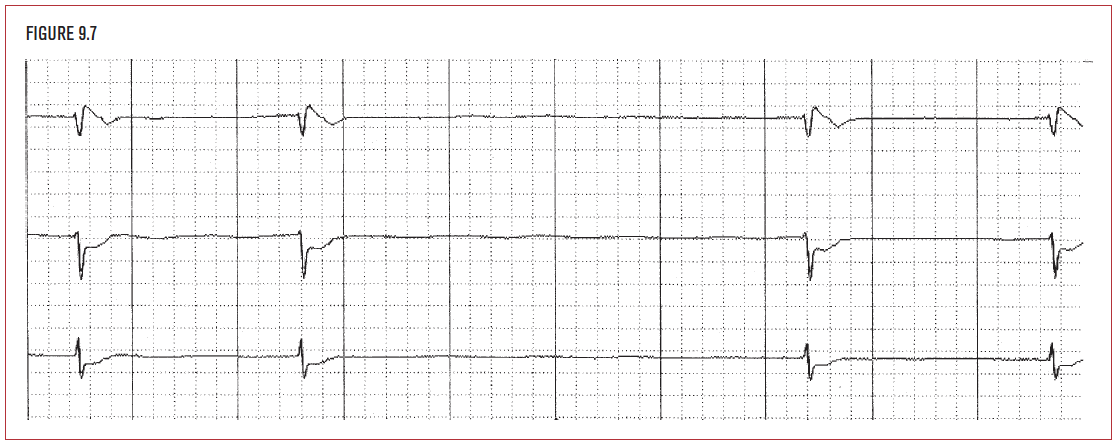
Ventricular escape beats (VE) are wide QRS complexes that come late and function as a rescue rhythm of last resort for the heart. They function at a slow rate, usually in the range of 30 to 40 bpm. The ventricular escape mechanism is not as reliable a pacemaker as the sinus node or junction. It is typically associated with significantly compromised myocardium, as would be seen in cardiac arrest.
Pacemakers
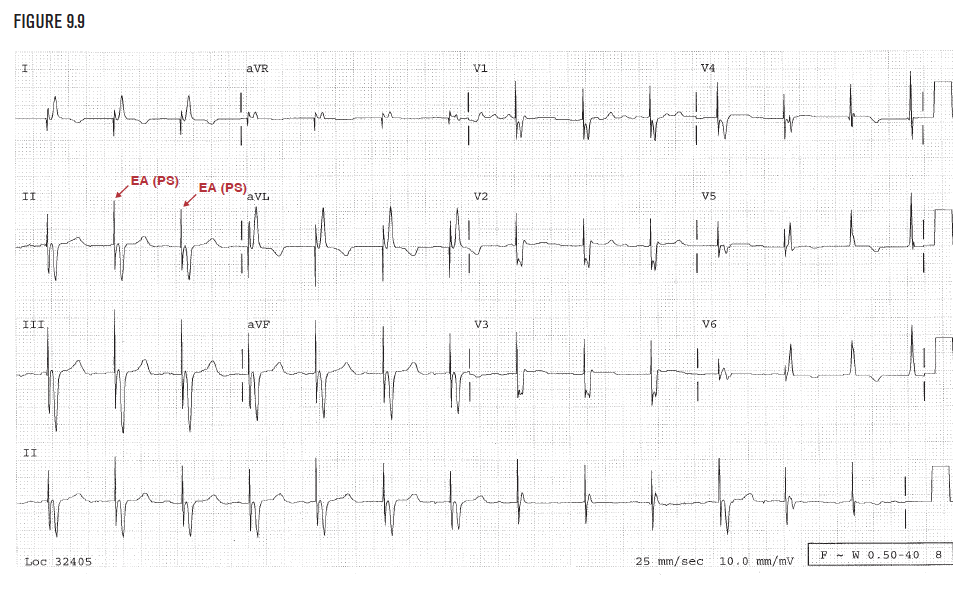
Ventricular pacing
Ventricular pacemaker rhythm demonstrates a vertical electrical artifact (EA) at the beginning of the QRS. Because each QRS in Figure 9.9 begins with a pacing artifact, this is pacemaker rhythm. The presence of the pacing spike (PS) demonstrates pacemaker output. The presence of an ST segment after the QRS proves that the pacemaker captured (depolarized) the ventricles. Ventricular pacemakers are used in the setting of complete heart block or episodes of asytole longer than 3 seconds (off any suspected medications), particularly in the setting of atrial fibrillation.
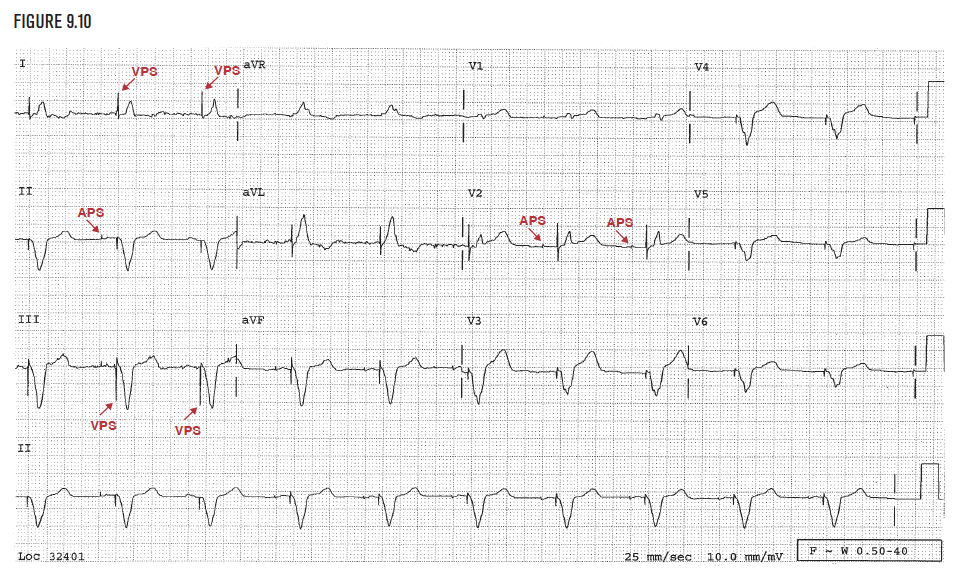
Figure 9.10 demonstrates vertical pacing spikes or artifacts before each QRS complex (VPS). In addition, a second pacing spike is present 0.16 seconds before the QRS. This represents an atrial pacing spike (APS). This is called AV sequential pacing. The pacemaker checks that a native beat has not occurred in time. Next it sends a charge into the atrial wall causing atrial depolarization. The pacemaker waits 0.16 seconds acting as an artificial AV node. Finally it sends a second charge into the ventricle depolarizing it. This pacemaker would be used in patients who have heart block or asystole but do not have atrial fibrillation. The use of two-chamber pacing is particularly important in the setting of heart failure.
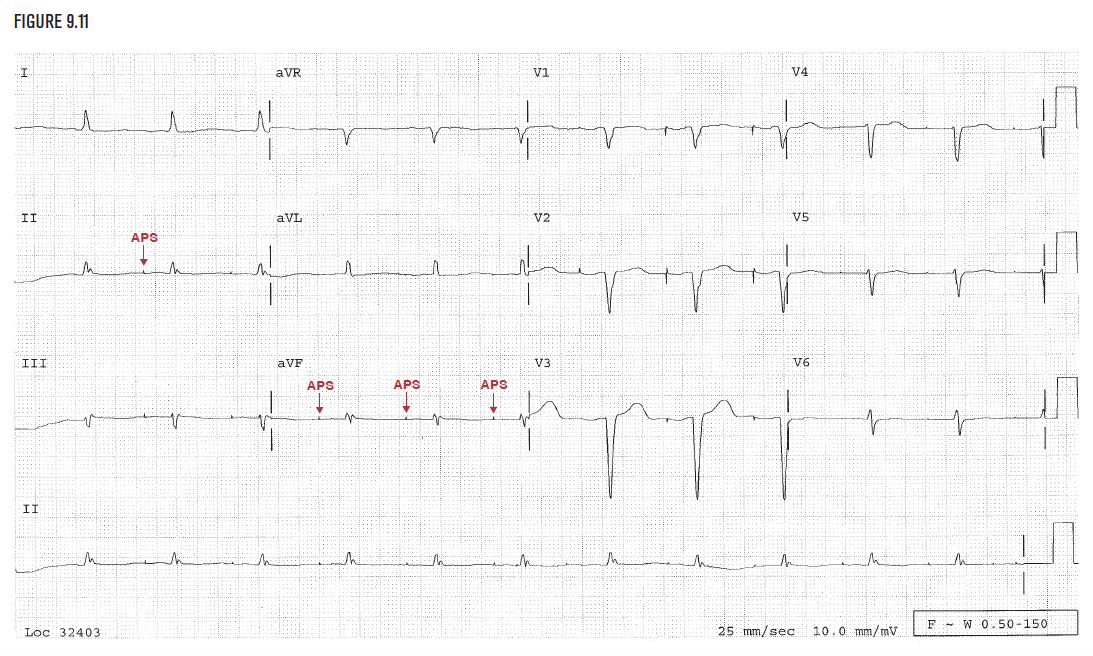
Atrial pacing
Figure 9.11 demonstrates atrial pacing alone. The pacemaker waits for the sinus node for a predetermined period of time. After this time passes, the pacemaker sends an electrical charge into the atrium. The rest of conduction is carried out normally through the patient’s AV node. Ventricular conduction is through the patient’s native conduction system. This system can only be used if the AV node functions normally. It cannot be used in atrial fibrillation.