Intro
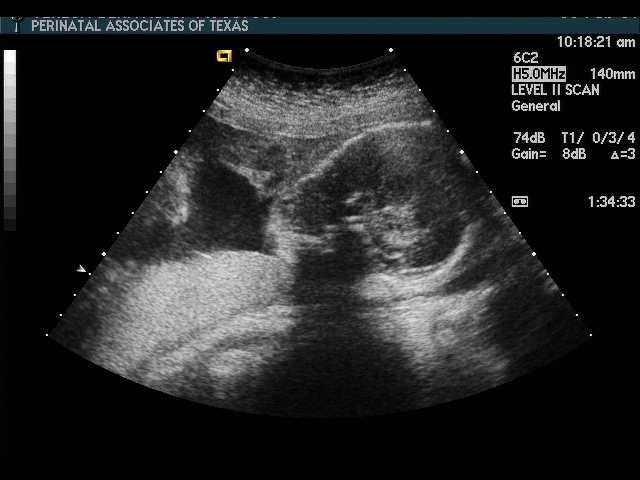
The fetal anatomy scan is the foundation for prenatal diagnosis and management. This scan is sometimes called a “Level II Scan,” although that nomenclature has been dropped by the AIUM.
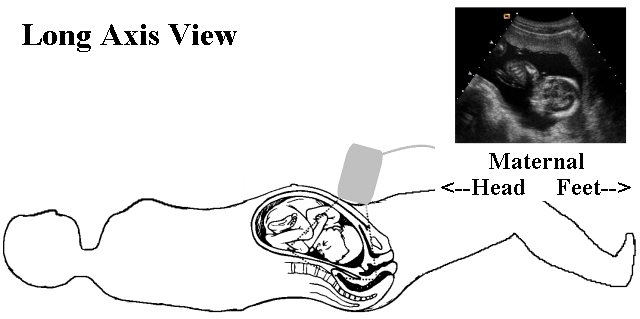
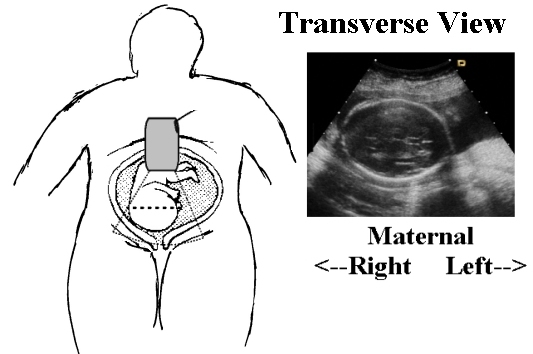
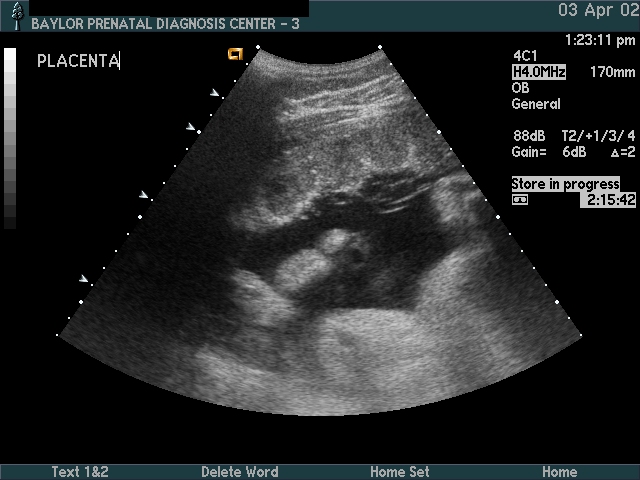
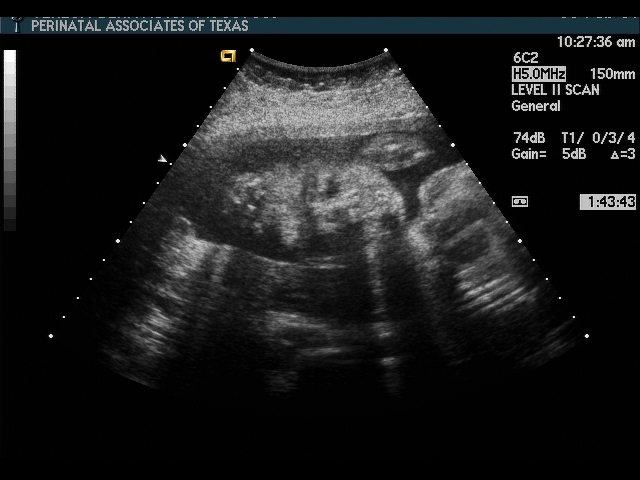
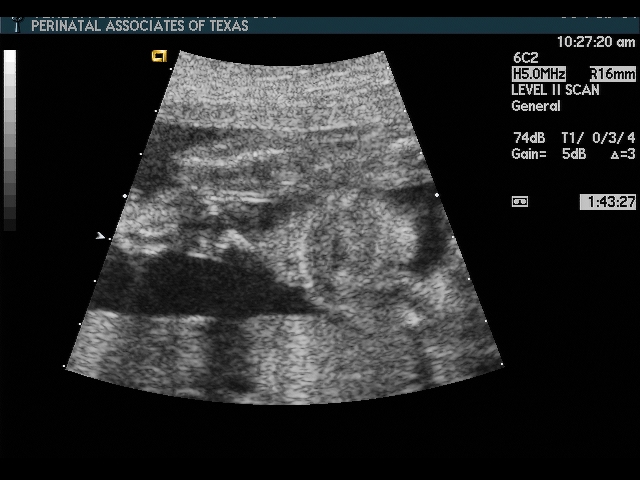
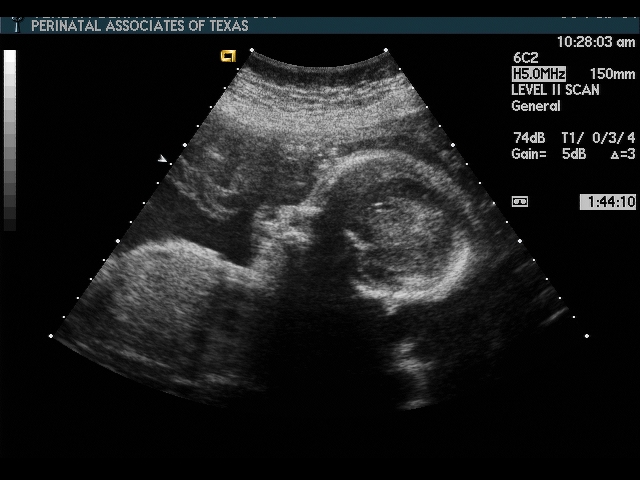
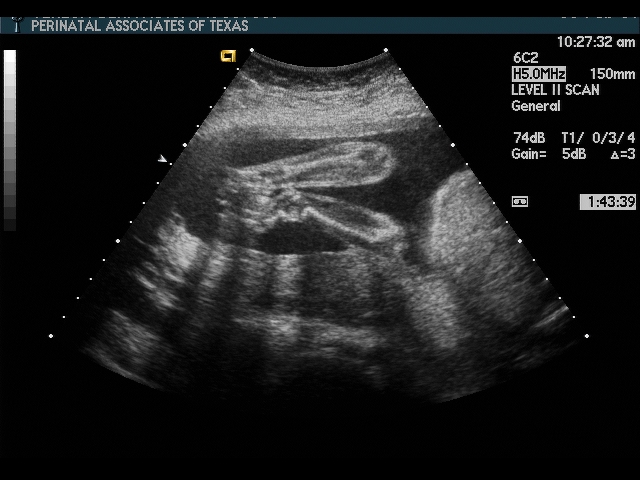
The elements of the basic fetal anatomy include evaluation of the uterus, fetal biometry and fetal anatomy. The sequence of ultrasound pictures shows how I perform a basic anatomy scan. The central principle of the scan is the demonstration of normal anatomy. The presence of a fetal anomaly is often recognized by the absence of normal anatomy. Many different approaches are possible, but it is important that the end result is a thorough review of fetal anatomy. I evaluate the overall fetal presentation, lower segment, placenta, fluid, biometry and fetal anatomy, in that order. In evaluating fetal anatomy I scan from top down (head to rump) to evaluate the neural axis (intracranial structures) and then from bottom up (rump to head) to evalaute fetal organs. Scanning in an organized fashion (much like a CT scan), helps me to remember what structures need to be visualized and avoids missing something. Jumping from structure to structure (i.e., “there’s the face, there’s the stomach, there’s the cord insertion, there’s the heart, …) increases that chance that you will forget something (“oops, I saw everything but the …”).
Although not a standard part of the fetal anatomy scan, testing fetal well-being is an important part of ultrasound scanning. A section is included on the biophysical profile.
Overview
When you first scan the patient, determine the number of fetuses, fetal lie, presentation and presence of a fetal heart beat. It is very embarrassing, not to mention distrubing for the patient, to scan for several minutes, commenting on structures, before you notice that the fetal heart is not beating. This does not mean that you should immediately say, “The fetus is dead!” if you identify an intrautrine fetal demise. Breaking bad news to the patient is a difficult and delicate task. I can only give you my approach.
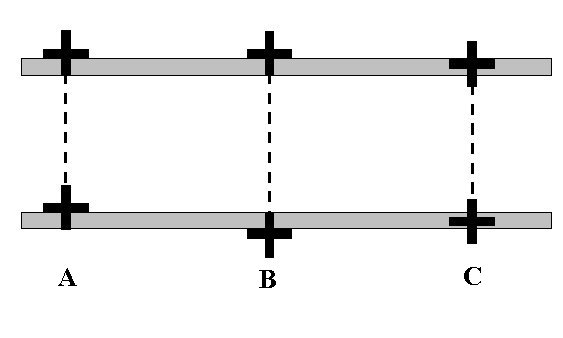
If this is a multiple pregnancy, the fetus closest to the cervix is designated “Fetus A”, next away from cervix is “B”, etc. It is important to determine zygosity if at all possible, as monozygotic twins have a higher risk of complications.
During this initial few minutes, fix the three-dimensional position of the fetus in your head. You should be able to remove the transducer and place it back on the abdomen at the location of any desired body part. (For example, place the probe over the fetal heart). This initial orientation will help you to work through the fetal biometry and anatomy.
Lower Uterine Segment & Placenta
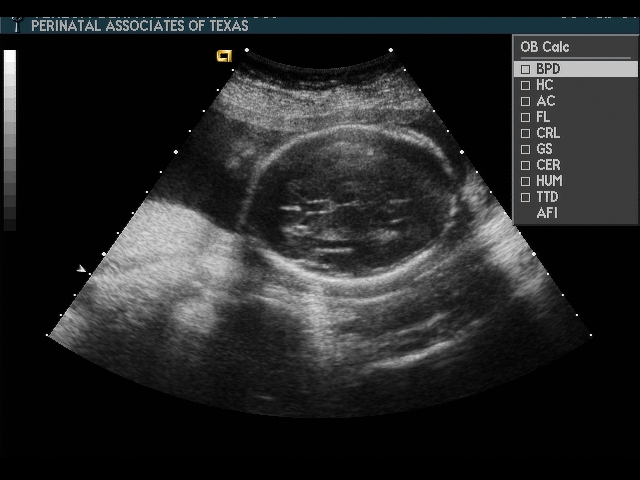
Biometry
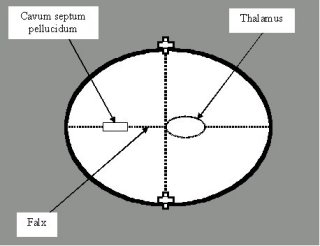
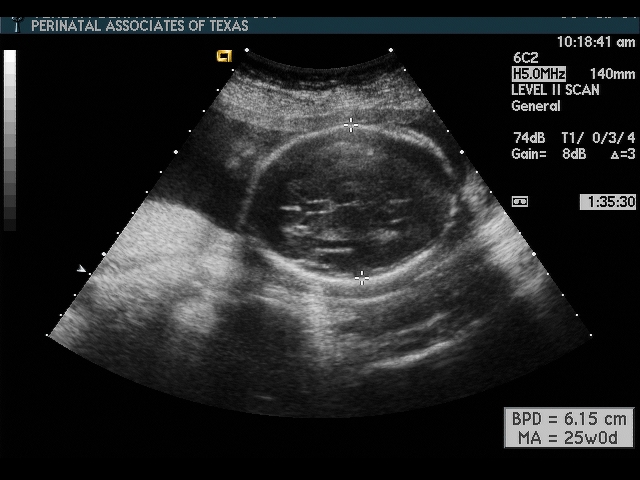
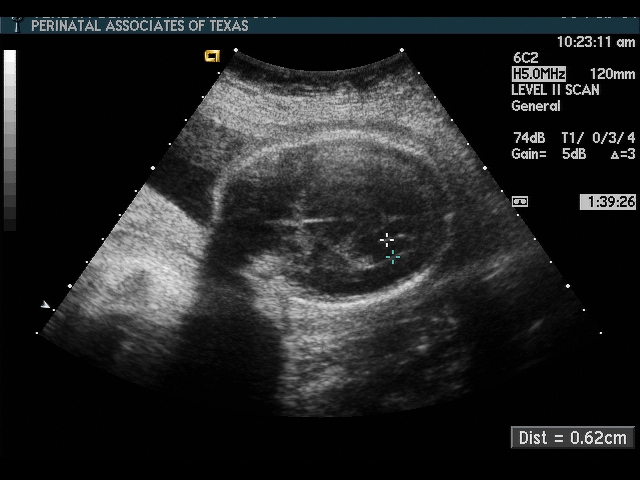
Biparietal Diameter (BPD)
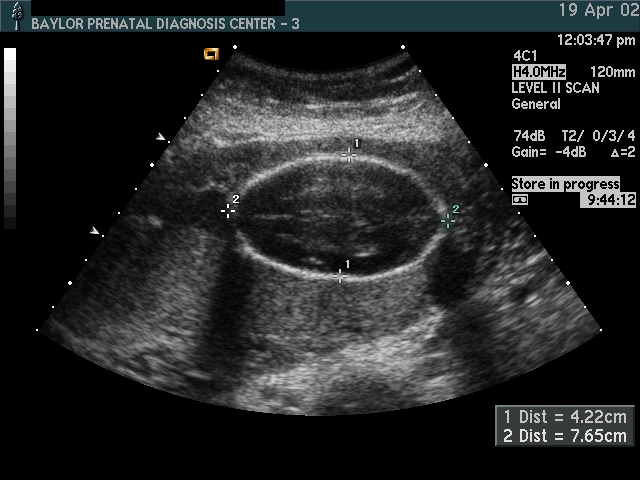
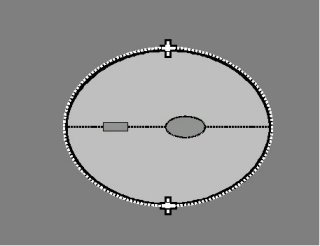
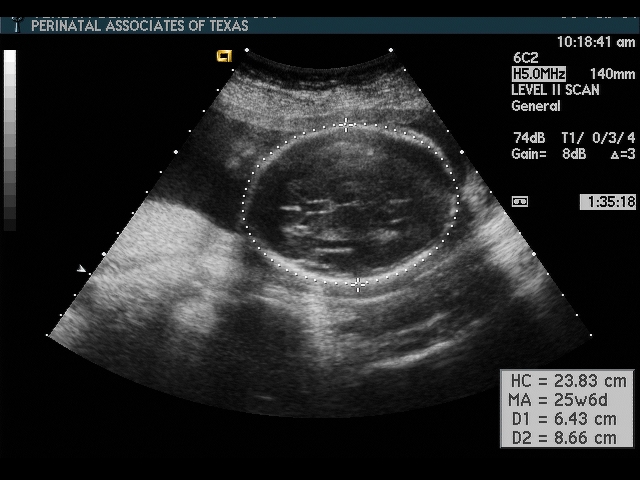
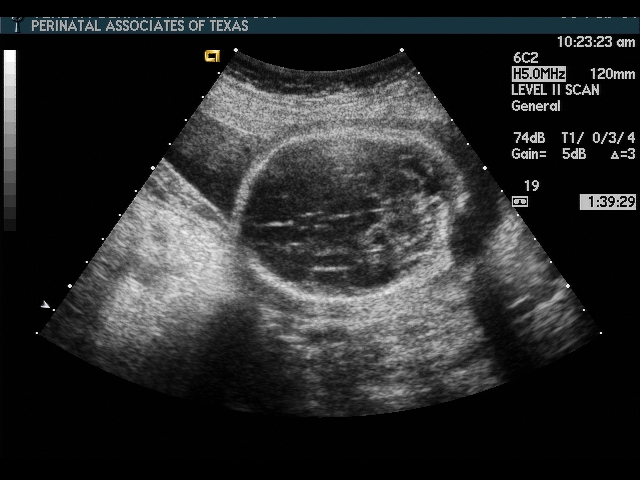
Head Circumference (HC)
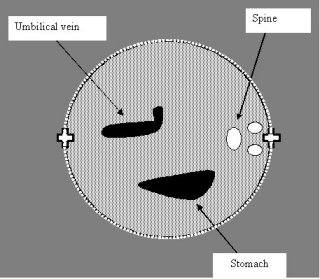
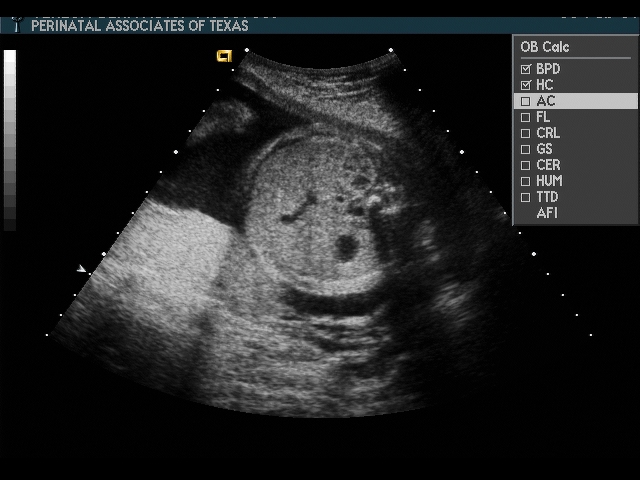
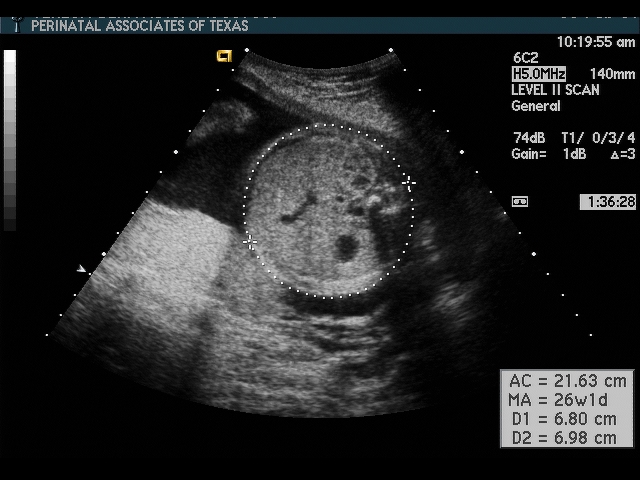
Abdominal Circumference (AC)
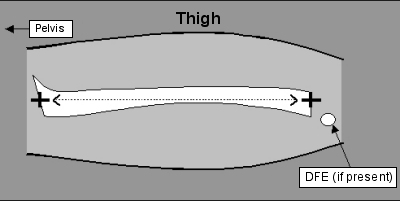
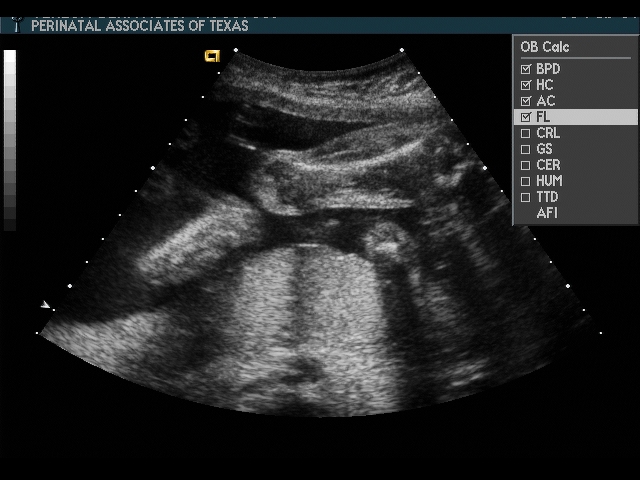
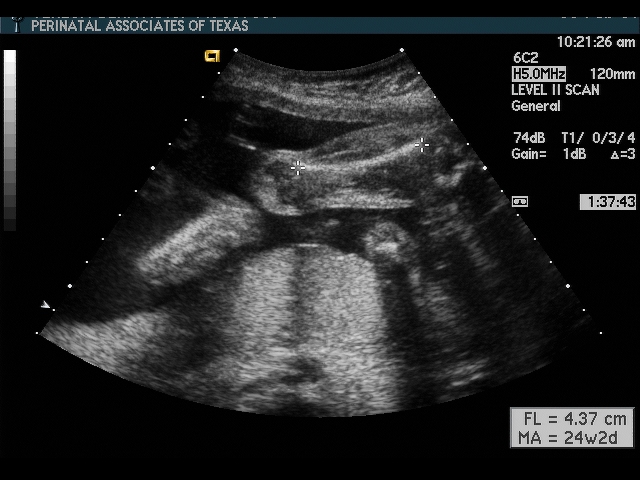
Femur Length (FL)
Fetal Anatomy
Scan fetal structural anatomy in an organized fashion. I begin with CNS and scan from head to coccyx, then scan fetal organs from perineum back up to face. Think of the fetal scan like a CT scan—a series of cuts (usually transverse through the fetal body). By scanning in a sequential manner you are less likely to forget to image a specific structure
Amniotic Fluid
Amniotic fluid is usually assessed by visual (subjective) assessment up to 22–24 weeks.
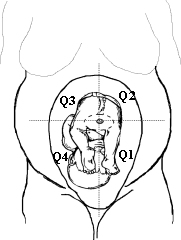
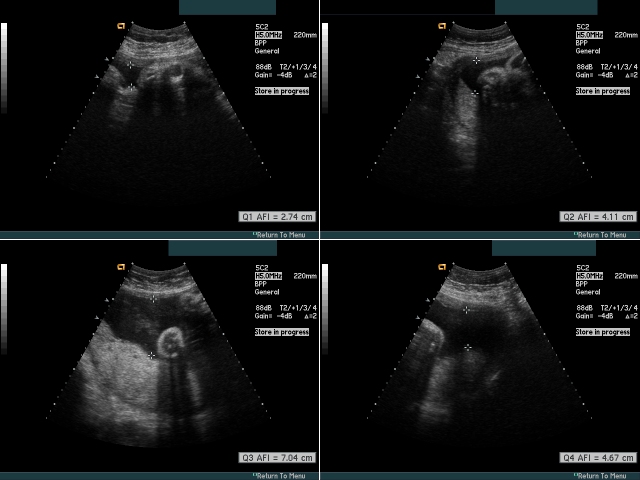
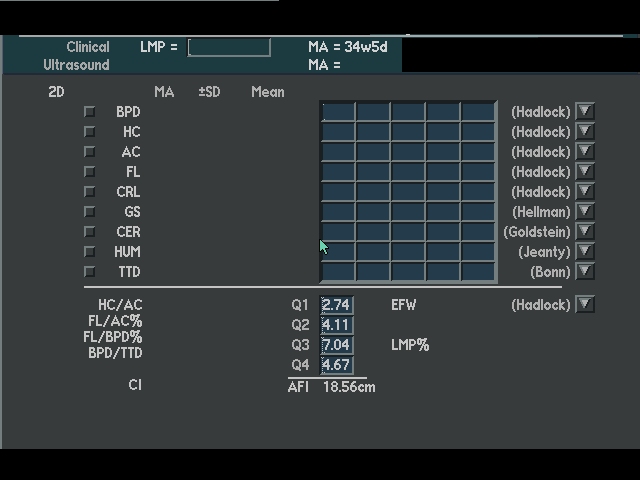
After 24 weeks, amniotic fluid should be specifically measured by the four-quadrant AFI technique.
Considerations:
- Polyhydramnios (especially note the presence, or absence, of stomach bubble)
- Excess production
- Diabetes
- Macrosomia
- Decreased swallowing
- CNS abnormality (aneuploidy, hydrocephalus, viral infection)
- Esophageal atresia
- T-E fistula
- Excess production
- Oligohydramnios
- Loss (PROM)
- Decreased Urination
- Decreased urine production
- IUGR
- Renal disease/anomaly
- Obstruction
- Kidney
- Ureter
- Bladder
- Absent kidneys (renal agenesis)
- Decreased urine production
Head
Considerations:
- Absent cranium
- Defect in cranium
- Absent cavum septum pellucidum
- Abnormal ventricles
- Abnormal cerebellum
- Other abnormalities
- porencephaly
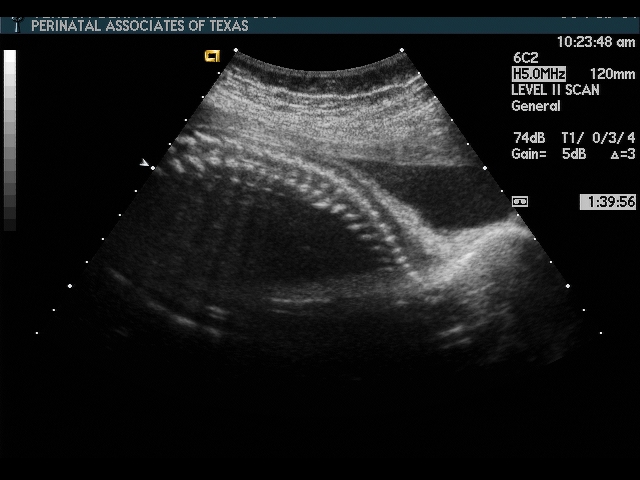
Spine
Considerations:
- Neural tube defect (spina bifida)
- Mass
- sacrococcygeal teratoma
- Abnormal angulation
- limb-body wall complex
- Other abnormalities
- caudal regression
Gender
Considerations:
- If known gender (i.e., genetic amniocentesis):
check U/S gender against amnio report—consider laboratory error or sexual differentiation error (e.g., testicular feminization) - Ambiguous genitalia
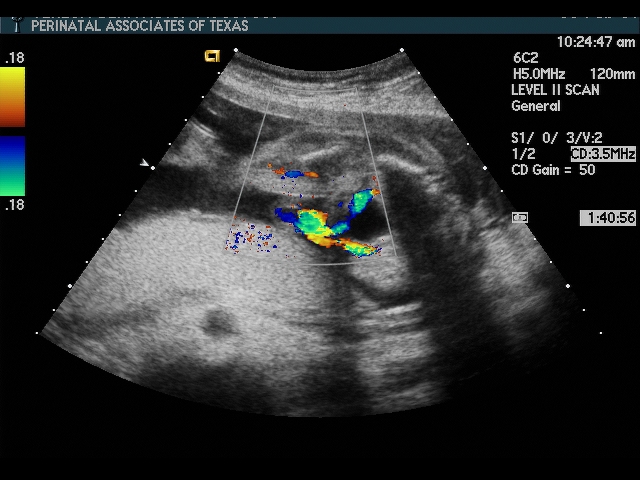
Bladder
Considerations:
- Bladder outlet obstruction
- Absent bladder—confirm expected bladder position by identifying umbilical arteries with color flow doppler
- renal agenesis
- infantile polycystic kidney disease
- Other
- ectopic ureterocele
Umbilical Cord
Considerations:
- Abdominal wall defect
- omphalocele
- gastroschisis
- pentalogy of Cantrell (includes ectopia cordis)
- Two vessel cord—associated with increased risk of cardiac or renal anomalies
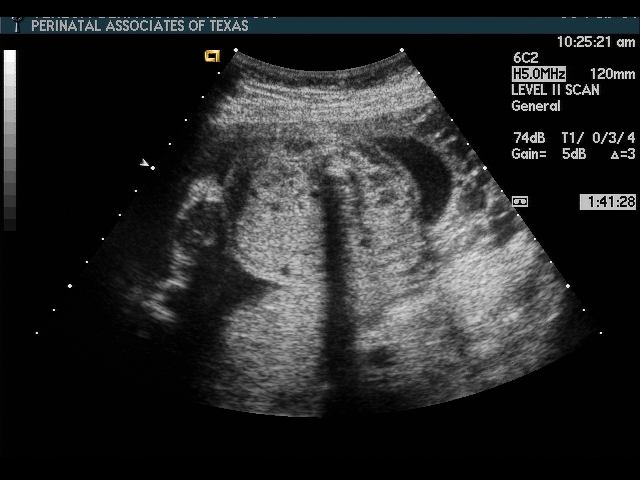
Kidneys
Considerations:
- Absence (renal agenesis)—bilateral or unilateral
- Obstruction
- uretero-pelvic junction (UPJ)
- ureteral
- ectopic ureterocele
- bladder outlet obstruction (posterior urethral valve in male)
- Pyelectasis (dilated renal pelvis)
- aneuploidy
- obstruction
- Abnormal morphology
- multicystic dysplastic kidney
- polycystic kidney disease
- Prune-belly syndrome
Stomach
Considerations:
- Absent stomach (especially if associated with polyhydramnios)
- esophageal atresia or T-E fistula
- Excessively large stomach (“double-bubble”) (possibly associated with polyhydramnios)
- duodenal atresia
- Abnormal location
- diaphragmatic hernia
- situs inversus
- polysplenia/asplenia (laterality sequence)
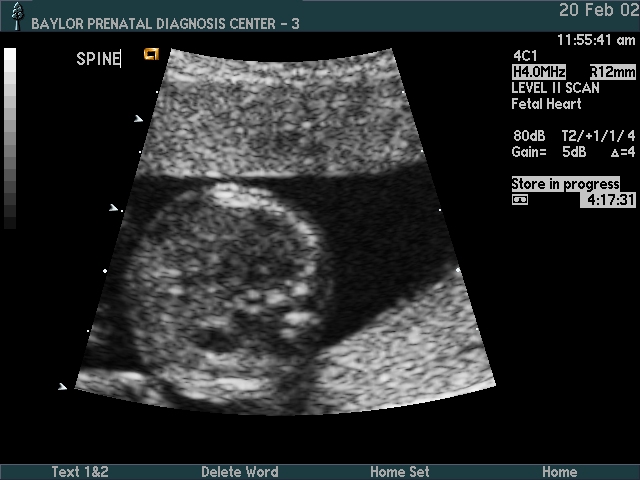
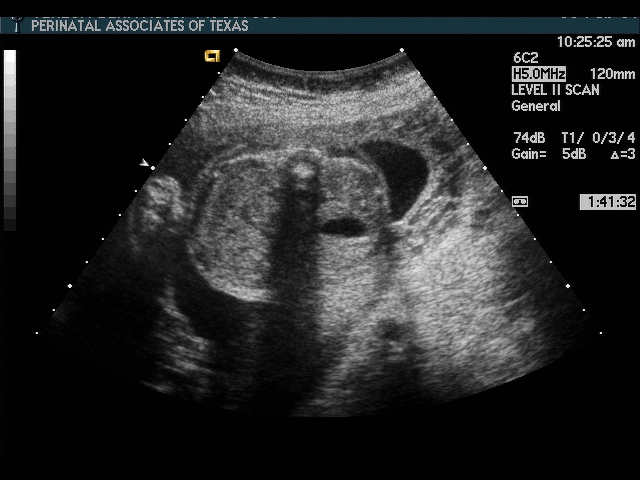
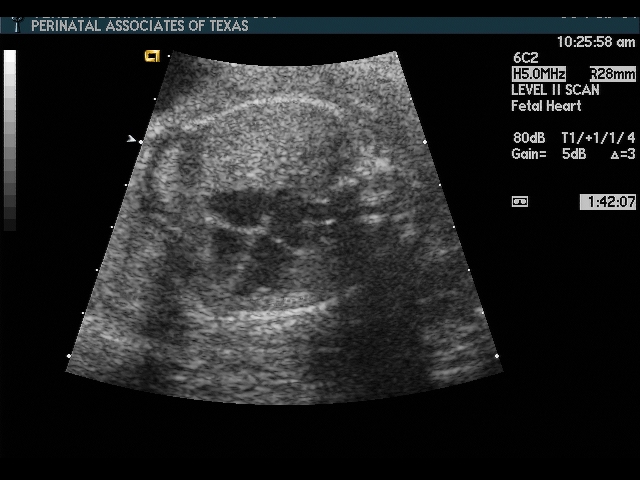
Heart
Considerations:
- Abnormal position
- pleural effusion
- pulmonary mass effect
- diaphragmatic hernia
- cystic adenomatoid malformation (CAM)
- eventration
- ectopia cordis (also found in pentalogy of Cantrell)
- Abnormal axis
- dextrocardia, situs inversus
- Abnormal 4 chamber view
- Abnormal outflow tracts
- Abnormal rhythm
- premature atrial contractions
- tachycardia
- bradycardia
- Pericardial effusion (component of hydrops)
- isoimmunization
- viral infection
Face
Considerations:
- Cleft lip
- Hypertelorism
- Hypotelorism
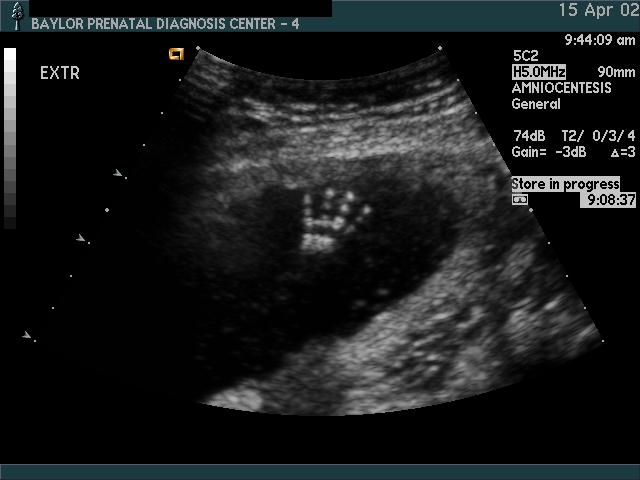
Extremities
Considerations:
- Skeletal dysplasia
- Screening for aneuploidy
- Polydactyly (rarely seen unless specific evaluation is undertaken)
- Syndactyly
- Clubfoot
Incidental Anatomy
Some anatomic features may be seen on occasion, but are not a part of a “routine” fetal anatomy survey. In some cases, these findings may be mistaken for abnormalities or confused with other fetal structures. For example, the fetal adrenals may be mistaken for fetal kidneys. These features are also included here because they do not fit well in any of the previous categories.
Some examples include:
- Fetal adrenals
- Fetal ear
Screening for Aneuploidy
It is common for ultrasound to be requested to screen for the risk of aneuploidy. In some cases a patient at increased risk of aneuploidy (e.g., age >= 35 y/o or an abnormal trisomy screen) wants to avoid amniocentesis, but expects that an ultrasound examination will provide additional information about her risk. It is important that the patient be aware that ultrasound cannot positively identify aneuploidy, and ultrasound cannot absolutely exclude the risk of aneuploidy.
The absence of identifiable anomalies may slightly decrease the baseline risk (that is, the age related risk) of aneuploidy, but it does not guarantee normal chromosomes. The presence of two or more anomalies, or a cardiac anomaly, or a number of specific single anomalies discussed elsewhere in this series, should alert the physician to the possibility of chromosome aneuploidy.
Some sonologists refer to a “genetic sonogram” that specifically looks for indicators of aneuploidy. These markers of chromosome abnormalities are not all actual anomalies, but are findings that point to an increased risk of aneuploidy. Conversely, if all markers are absent (or are within normal range) the risk of aneuploidy is reduced.
Some markers of aneuploidy include:
- Nuchal thickening
- Choroid plexus cysts
- Cardiac anomalies
- Echogenic intracardiac focus
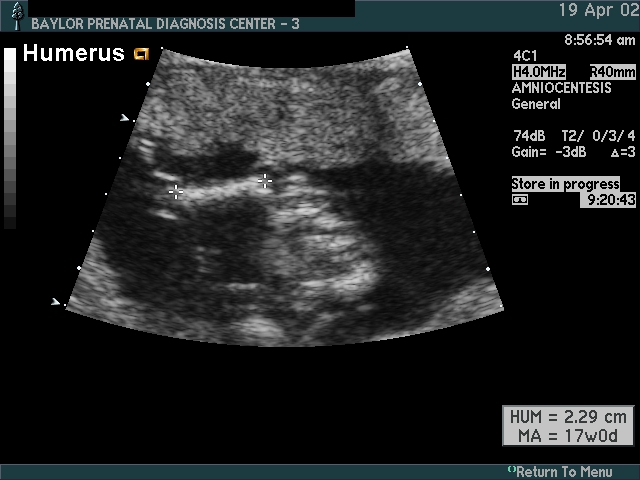
- Femur length
- Humerus length
- Echogenic bowel
- Renal pyelectasis
- Clinodactyly
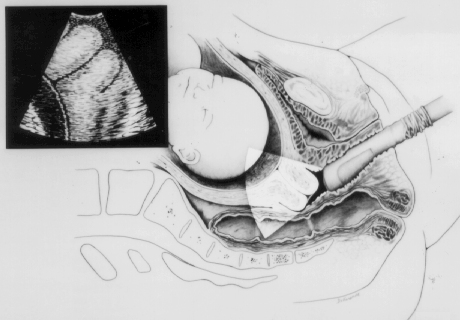
Cervix: Endovaginal and Perineal Evaluation
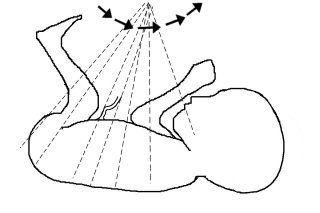
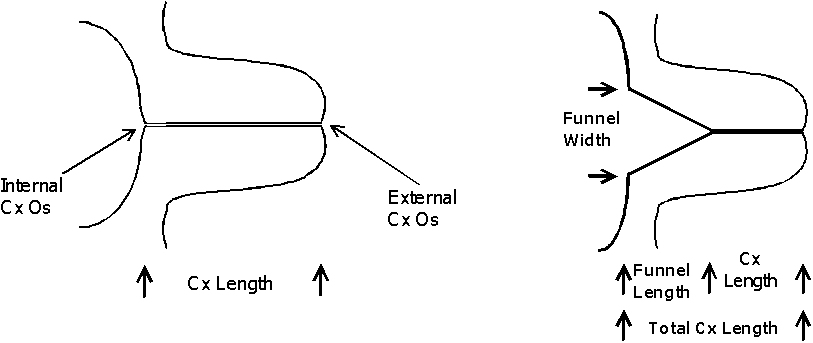
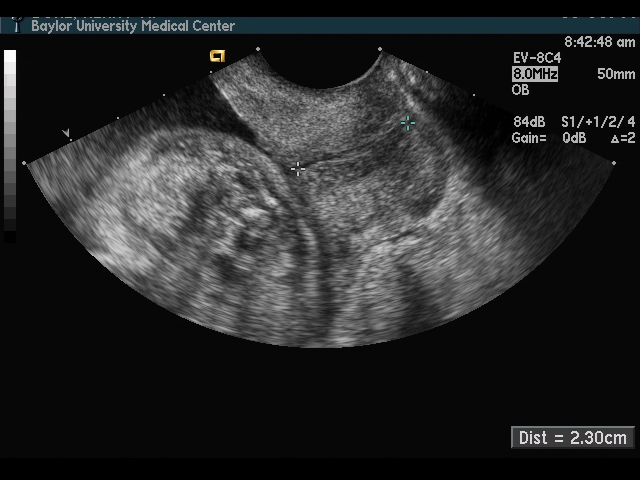
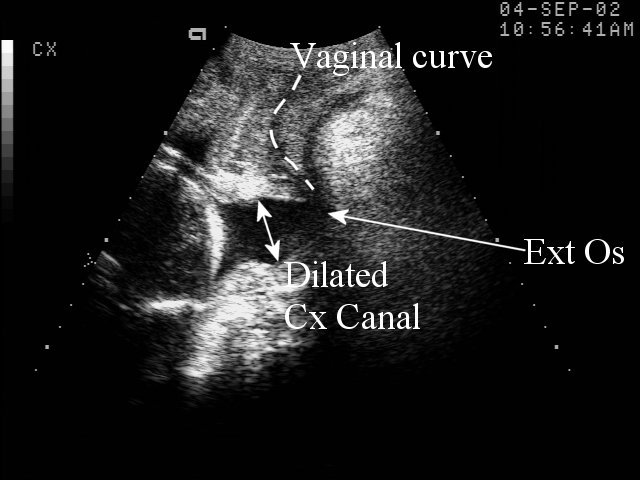
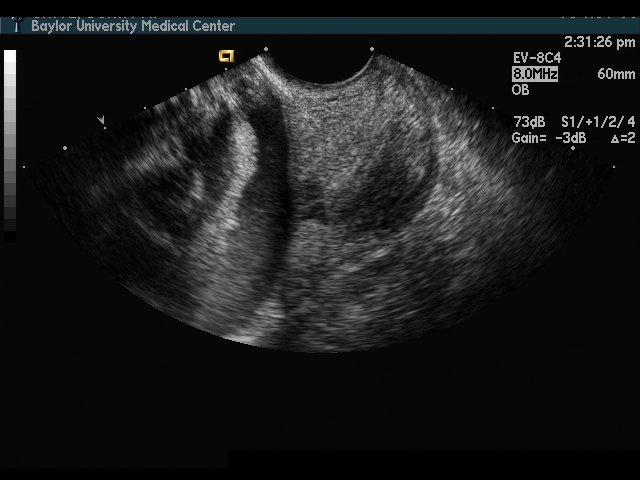
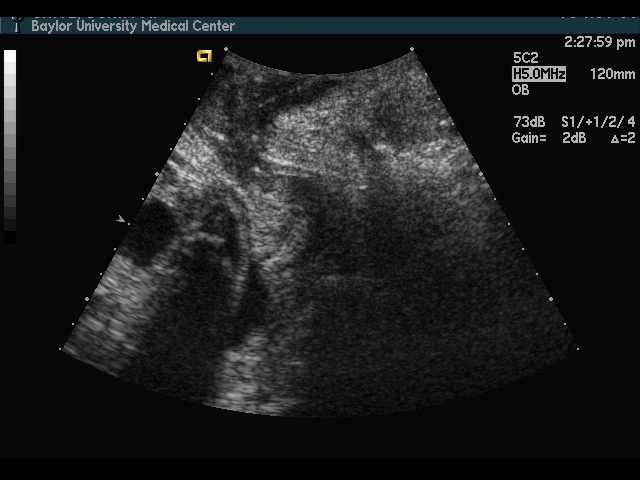
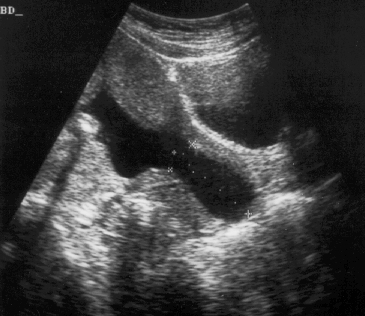
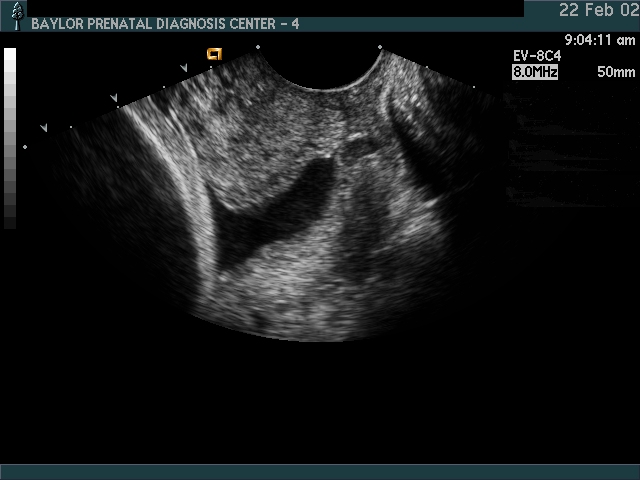
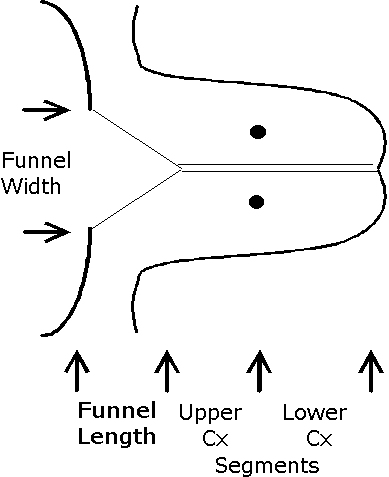
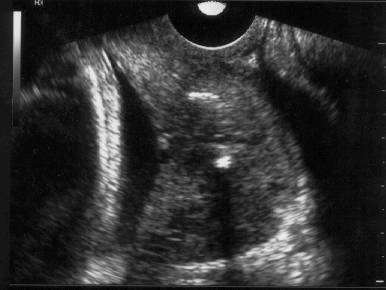
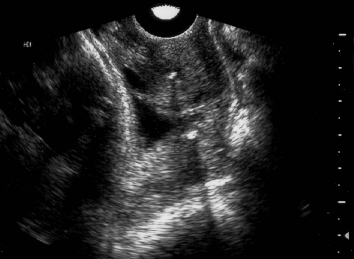
Endovaginal and perineal ultrasound are usually performed with an empty bladder. Visualize the cervix in a sagittal plan. It is usually easiest to first identify the internal cervical os, then adjust the probe until the entire cervical canal is visualized. The external os may be difficult to see, but it can be identified by following the curve of the posterior lip of the cervix to its intrsection with the cervical canal. Gradually relax pressure on the transducer until the image becomes slightly blurred. Reapply gentle pressure sufficient to establish a sharp cervical image. The length of the closed cervical canal is measured. Funneling of the upper cervical canal, if present is not included in the measurement of cervical length. Funneling may indicate incompetent cervix (depending on gestational age, obstetric history, and clinical circumstances).
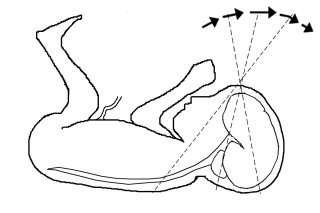
Perineal scanning is performed with a standard curvilinear probe, covered with a glove and applied to the perineum using a large amount of gel. Place the probe gently between the labia and adjust to get a clear image of the cervix. Perineal scanning is more difficult to learn than endovaginal scanning. The vagina curves, and there is frequently shadowing from the pubic bone and from stool in the rectum. Moving the probe slightly to the side or up or down may improve the visualization.
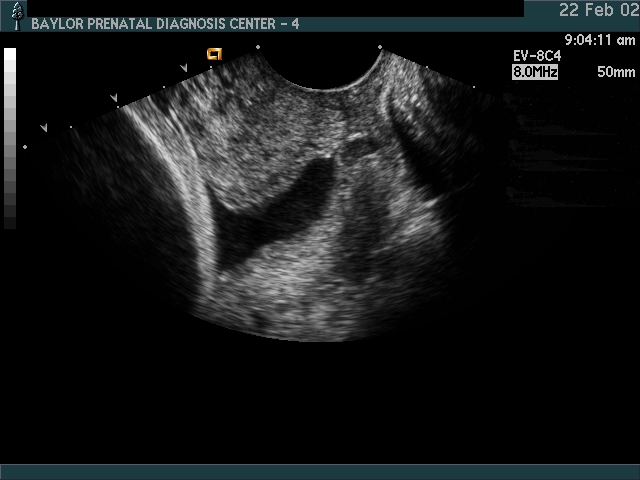
Cervical Incompetence and Cerclage
In my opinion, funneling of the upper cervical canal is the most important diagnositic criterion for cervical incompetence. Funneling necessarily results in a shorter cervical length (since the cervical length measurement includes only the closed portion of the cervix). In some cases, the cervix may be very short, due to loss of the external portion of the cervix, yet the internal os remains competent. Evaluation of patients at risk of incompetent cervix may require serial scanning to identify developing cervical incompetence. Incompetent cervix can develop rapidly, as is demonstrated by the first two scans (even though these are abdominal). Obstetric history is extremely important. In some patients, I believe cerclage is indicated even with a normal cervical ultrasound if the obstetric history is strongly suggestive of cervical incompetence.
Cervical ultrasound measurement after cerclage is predictive of outcome. The cervical canal is measured above and below the cerclage (I usually designate these measurements as “Upper segment length” and “Cerclage to external os length”). The upper segment length is most predictive of outcome.
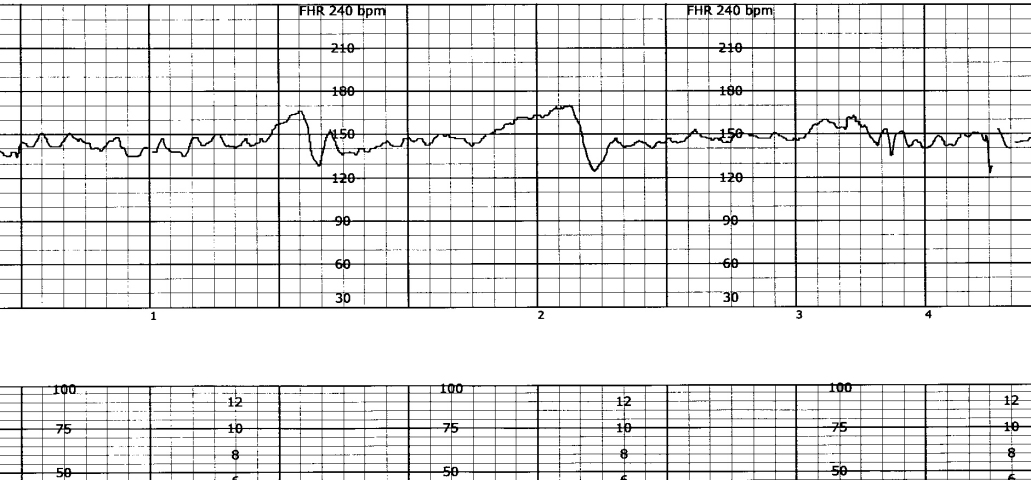
Biophysical Profile Testing fetal well-being
A Biophysical Profile (BPP) is a test of fetal well-being. It addresses the question, “Is this fetus healthy, or is it possibly showing signs of stress or distress that necessitate delivery?” A BPP has 5 components that are each scored 0 or 2. A BPP score of 8 or 10 is considered reassuring. A BPP score of 6 or less is not reassuring; further intervention will depend on clinical factors such as existing complications of the pregnancy, gestational age, etc.
The components of a BPP are:
If the finding (component) is positive score 2 points, otherwise score zero.
- NST: At least 2 accelerations (15 bpm x 15 seconds) in 20 minute window with normal baseline variability
- Fetal movement: At least 3 gross body movements in a 30-minute window
- Fetal tone: At least 1 flexion / extension movement in a 30-minute window
- Fetal breathing: At least 30 seconds of sustained fetal breathing in a 30-minute window
- Amniotic fluid: At least one pocket of fluid measuirng >2 x 2 cm, OR an AFI > 5 cm
Some comments about BPP:
- Although a full BPP includes an NST, sometimes we do an “ultrasound only” BPP, scoring 8/8 if all four ultrasound components are positive
- BPP scores are always even numbers (0, 2, 4, 6, 8, 10)—there are no odd-numbered BPP scores
- Oligohydramnios predicts an increased risk of adverse fetal outcome. Thus a BPP of 8/10 may be abnormal if the 2 points are taken off for amniotic fluid