- Optional Reading
The Developing Human: Clinically Oriented Embryology, 11th ed., Development of urinary system section through Development of suprarenal glands.
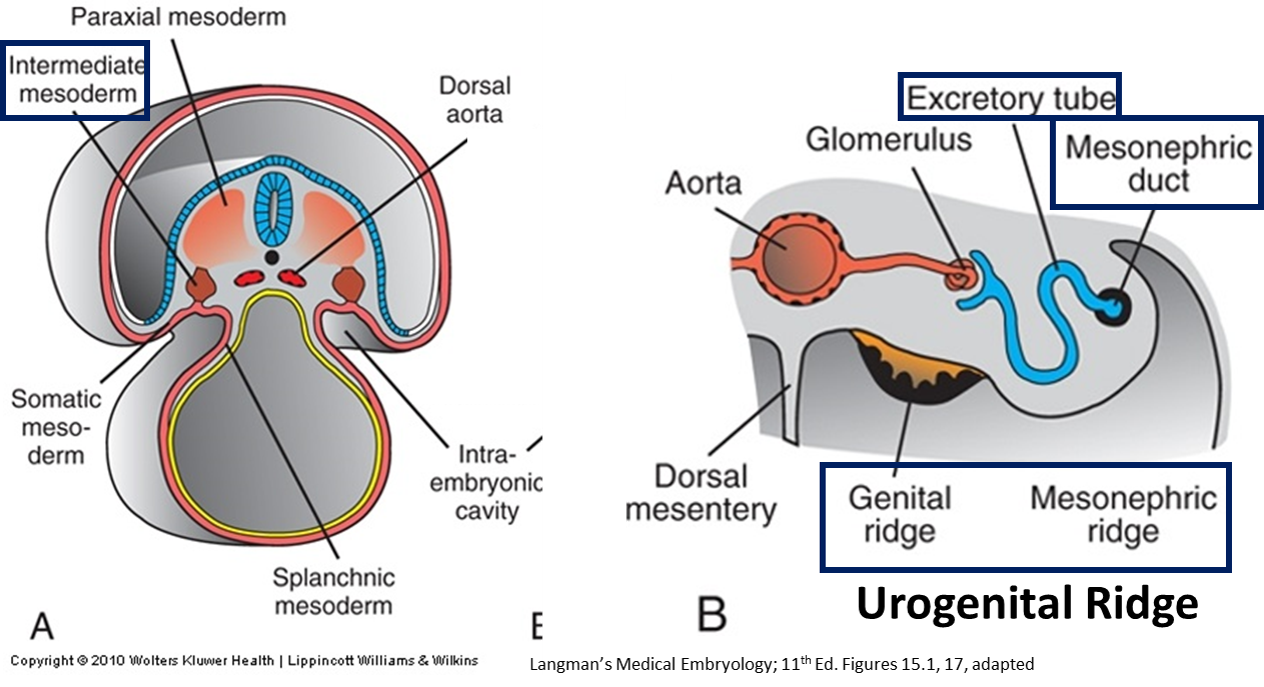
The urinary and reproductive (genital) systems have several features in common and are sometimes considered together as the uro-genital system. Most shared features are developmental in nature:
- Both the kidneys and the gonads arise from the intermediate mesoderm along the posterior abdominal wall (in urogenital ridge).
- Kidneys arise as a set of tubules in the lateral part of the ridge, the nephrogenic cord. Some of the earlier developing parts of the ducts of the urinary system (mesonephric duct and tubules) are shared with the developing gonads.
- Males: The genital system takes over some kidney ducts (for example, the ductus deferens forms as a urinary duct) and both systems’ products exit through the same tube (urethra) in the adult.
- Both systems initially empty into the cloaca (the embryonic “sewer” near the hindgut, as described later in the chapter).
A brief intro to microscopic anatomy
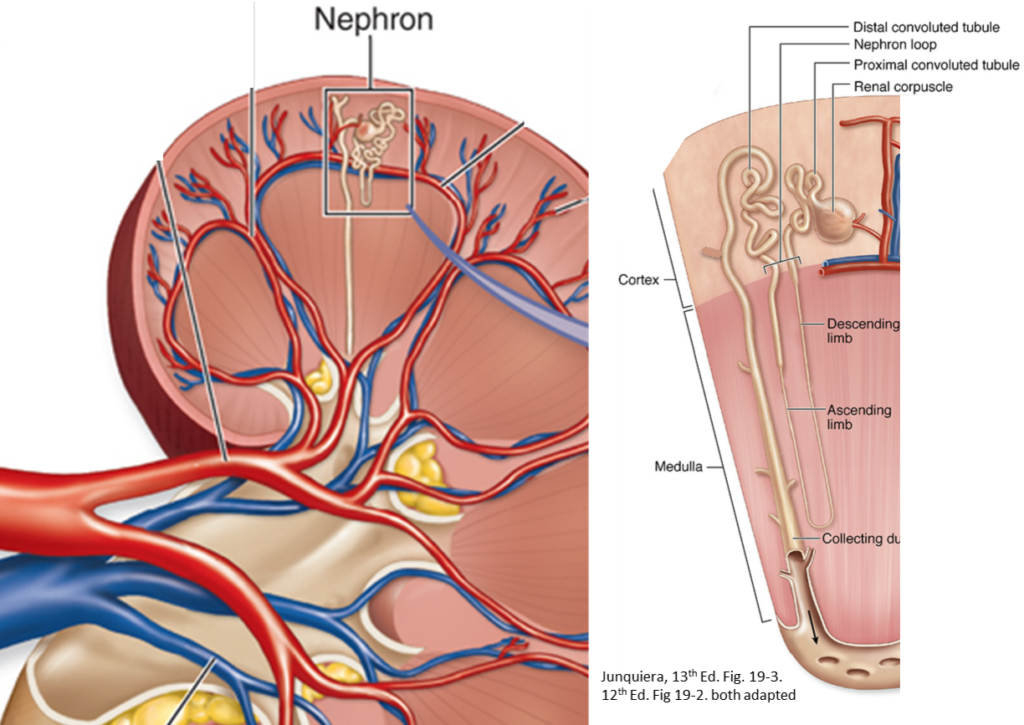
The internal gross features of the kidney correlate with its microscopic organization.
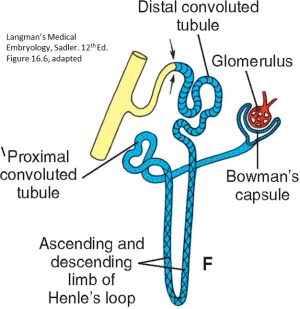
The basic functional unit; has different specialized regions for filtering the blood and reabsorption of fluids and electrolytes.
- Glomerulus (L., little ball of thread): A tuft of capillaries invaginating Bowman’s capsule
- Bowman’s capsule (BC): Cup-like sac at the proximal end of nephron
- Proximal convoluted tubule (PCT): Extends from Bowman’s capsule
- Ascending and descending limbs of the loop of Henle
- Distal convoluted tubule
Not part of the nephron different embryological origin (note change in color)!
Renal cortex and cortical columns
Contain all of the glomeruli, and all parts of the renal tubules except for the loops of Henle.
Contains structural specializations involved in water reabsorption and salt balance performed by the loops of Henle (more in histology).
Urine is transported by the collecting ducts to the calyces, renal pelvis, ureter, and then the urinary bladder.
Origins: Kidneys, ureters, urinary bladder, and urethra
-
Know this!
Different parts of the urinary tract come from different embryologic sources:
-
Nephrons
The excretory units of the kidneys (from intermediate mesoderm)
-
Collecting system
Collecting ducts through ureters (from mesonephric duct)
-
Urinary bladder and urethra
(From primitive urogenital sinus)
Kidney forms from intermediate mesoderm
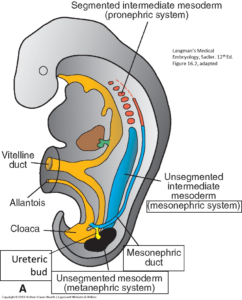
At about 21 days of development, the intermediate mesoderm forms between the somites and the lateral plate mesoderm. Intermediate mesoderm forms the kidneys and the gonads.
Kidney
- Tubules (nephrons) form at 4 weeks in cervical region, 1 per body segment
- Degenerates! THE END.
- Forms interim kidney in thoracic region
- S-shaped mesonephric/excretory tubules, 3–4 per body segment connect temporary mesonephric kidney to a longitudinal collecting duct: the mesonephric duct.
- Most of the mesonephric kidney degenerates by the end of the second month of development
- Mesonephric (Wolffian) duct persists in the adult, becoming sperm-carrying tubes of male reproductive tract (ductus deferens, ejaculatory ducts, epididymis, and efferent ductules); is vestigial in females
The functional fetal and adult kidney
-
- Develops from intermediate mesoderm in pelvic region, begins development around Week 5
- Collecting ducts develop from ureteric bud
- Buds off of mesonephric duct into the metanephric mesenchyme/mesoderm
- Divides into smaller branches (12 orders): Major and minor calyces, and collecting ducts
- Excretory units (nephrons) develop from metanephric mesoderm by forming caps over the collecting ducts
- Glomerular capillaries associate with these nephrons medially; distally, the tubules link the Bowman’s capsule to the collecting unit, establishing the proximal and distal convoluted tubules and the Loop of Henle
- About 1 in 750 people lack one kidney because the ureteric bud has degenerated early on one side, failing to induce the formation of nephrons in the nephrogenic cord.
- During the second half of development (10th week to 9th month), the metanephros is functional and the fetus produces urine. The fetus urinates this into the amniotic sac.
- Then, the fetus drinks the amniotic fluid, reabsorbing the contained urea through the intestine into the blood and excreting it across the placenta.
- By urinating into the amniotic sac and then drinking, the fetus can continually renew the amniotic fluid and regulate the volume of this fluid. The fetus controls the volume of the amniotic fluid.
- At birth, too little amniotic fluid in the amniotic sac (oligohydramnios) can indicate non-functioning kidneys, whereas too much amniotic fluid (polyhydramnios) can signify brain damage or a blocked esophagus.
- The kidneys are markedly lobed at birth, being covered externally with bulges. Each lobe represents the renal tissue around a single minor calyx and its branches. The lobes disappear during infancy as the nephrons grow bigger, but not in number.

Ascent of the kidneys
Video 31.1. Ascent of kidneys and development of renal arteries. Embryology, University of New South Wales.
- Metanephric kidney gradually moves cranially out of the pelvis.
- Reach their final lumbar location by the 9th week
- Possibly due to differential rates of growth of the pelvic versus the lumbar parts of the body (pelvis grows caudally fast).
- As it slowly “ascends,” the kidney receives progressively higher paired blood vessels from the aorta and inferior vena cava.
- If the lower vessels fail to degenerate, accessory renal arteries or veins will be present after birth. About 30% of all kidneys have such extra renal arteries.
- The ascending kidney must pass up through the pelvic brim, through an arterial fork formed by the right and left umbilical arteries.
- Difficulty in traversing the fork can lead to a symptomatic, essentially harmless, developmental anomalies:
- Pelvic kidney: Kidney remains down in the true pelvis
- Horseshoe kidney (1 in 600): Caudal poles of both kidneys fuse; such kidneys make it up into the abdomen, but get stuck at the root of the inferior mesenteric artery at L-3.
- Difficulty in traversing the fork can lead to a symptomatic, essentially harmless, developmental anomalies:
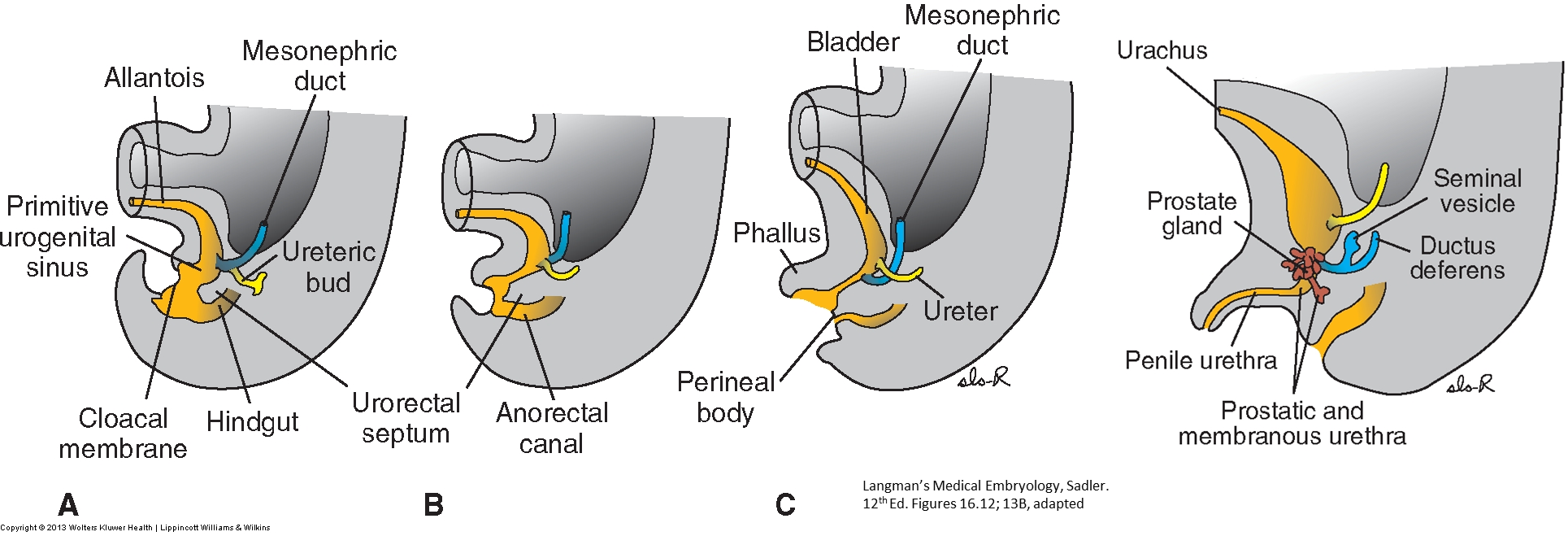
Bladder and urethra
- Derive from the cloaca, the caudal expanded portion of the hindgut.
- From the 4th to the 7th week of development, the uro-rectal septum grows caudally to subdivide the cloaca into two parts:
- Primitive urogenital sinus: Spindle-shaped ventral subdivision.
- Anorectal canal: Dorsal subdivision, tube-shaped continuation of the hindgut.
- Primitive urogenital sinus: Becomes bladder, urethra, vestibule of vagina, and a vestigal structure called allantois.
- Distal part of allantois: Remains attached to primitive urogenital sinus and, after birth, becomes the urachus in the anterior abdominal wall.
- Meanwhile: Mesonephric duct is attached to the cranial and dorsal side of the primitive urogenital sinus (A, Figure 31.7).
- Ureteric bud/ureter: Grows off the mesonephric duct near here. Recall: mesonephric duct will become the sperm-carrying ductus deferens in the male . . .
- If this were retained, sperm would ejaculate into the bladder, and the ureter would not empty directly into the bladder—rendering reproduction and the storage of urine impossible.
- To avoid this, the proximal part of the mesonephric duct is absorbed (intussusception—remember this term from heart development?) into the posterior wall of the bladder up to the point where the ureteric bud branches (B, Figure 31.7).
- Ureter then empties directly into the bladder; mesonephric duct is now separate from ureteric bud
- Ureteric orifices move farther cranially because the kidney ascends
- Mesonephric duct migrates caudally to attach to urethra just below the bladder (indeed, why the ductus deferens empties into the urethra).
- This also occurs in female embryos as in the male; however, the female mesonephric duct subsequently degenerates.
- The portion of the bladder wall formed by absorption of the mesonephric ducts is called the trigone. The three corners of the trigone contain the two ureteric orifices (above) and the internal urethral orifice (below).
Epithelium
- Most of the bladder is derived from the hindgut, so its inner epithelium is derived from endoderm.
- Both the mesonephric ducts and ureters come from mesoderm: mucosa of the bladder formed by incorporation of the ducts (trigone) is also mesoderm.With time, it is replaced by endodermal epithelium.
- Epithelium of urethra in both sexes comes from endoderm; the surrounding connective tissue and smooth muscle are from splanchnic mesoderm.
- At the end of the 3rd month, the epithelium of the proximal urethra begins to proliferate and forms a number of outgrowths that penetrate the surrounding mesenchyme.
- In males, these buds form the prostate gland.
- In females, these become urethral and paraurethral glands.
Development of suprarenal (adrenal) glands
- The development of this organ is NOT related to kidney development—but is discussed in this chapter for topographic convenience. (See here for review.)
- The cortex of the suprarenal gland is derived from mesoderm—specifically from proliferation of the mesothelium lining the coelom between the root of the gut’s dorsal mesentery and the intermediate mesoderm.
- The medulla of the suprarenal glad is derived from neural crest that migrates from the primitive neural tube. Thus, the suprarenal medulla is a modified sympathetic ganglion.
- The two parts of the suprarenal gland have different functions and different embryonic origins. Boo-yah!