Epidural hematoma
- Location
- Cause
- Demographics
- Clinical presentation
- Imaging
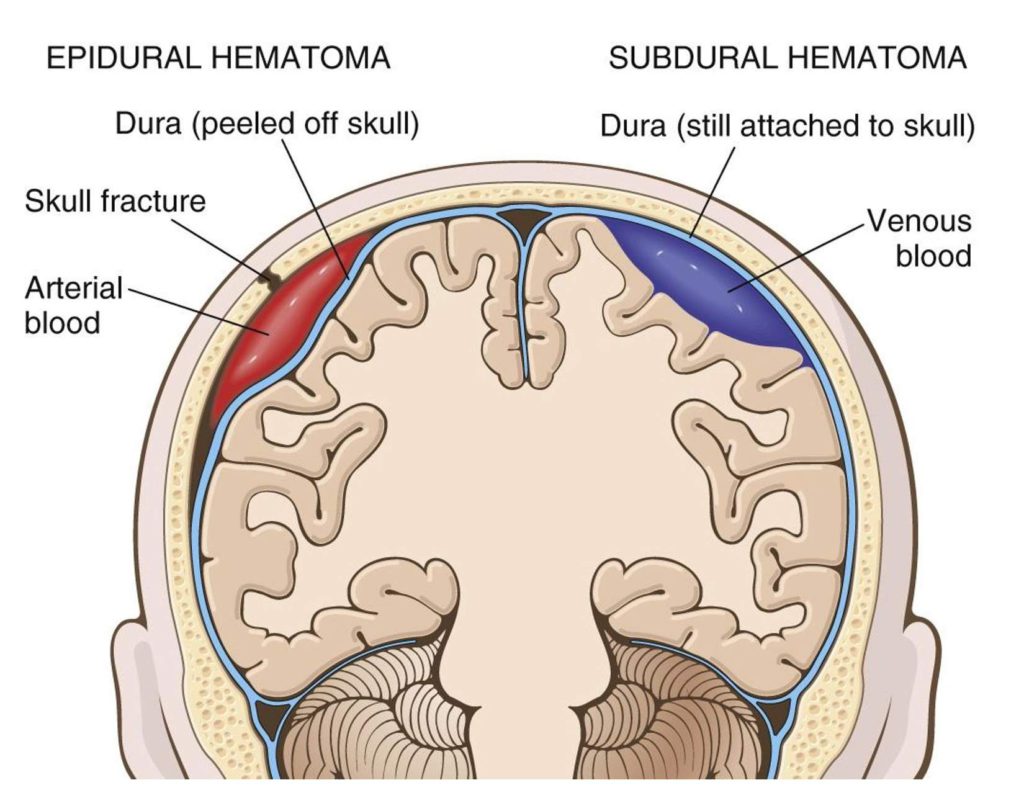
Extra-axial; between dura and skull (often temporal bone), or dura and vertebrae if spinal.
Most commonly traumatic; frequently involves skull fracture. Typically an arterial bleed (middle meningeal artery), but can also be venous.
-
-
Arterial source → rapid bleed.
-
More commonly seen in younger patients; attributed to traumatic nature as well as increased adherence of dura to skull in older individuals.
-
Lucid interval common.
-
Ipsilateral blown pupil → due to increased ICP and resulting uncal herniation/CN3 compression.
-
+/– vasopressor response (widened pulse pressure and decreased HR response to increased intracranial pressure)
-
Widened pulse pressure (increased systolic, decreased diastolic)
-
Bradycardia
-
Irregular respirations
-
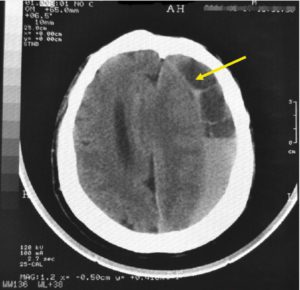
Usually does not cross suture lines.
Often see associated bony abnormality due to fracture.
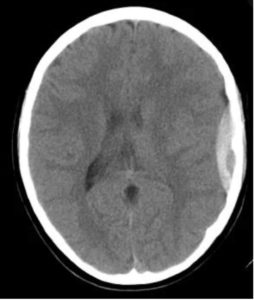
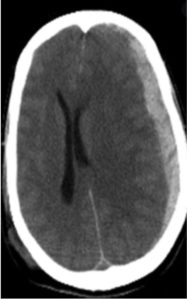
CT
-
Characteristic lentiform (biconcave) shape.
-
-
If continued bleeding during CT, may see swirl sign.
-
+/– midline shift and compression of ventricles.
-
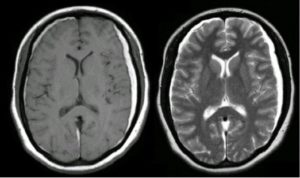
MRI
May see displaced dura as a hypo-intense line on T1 and T2 sequences.
-
-
Can help to differentiate from subdural origin.
-
Traumatic epidural hematoma
Neurosurgical Intervention
Epidural vs. subdural hematoma
Subdural hematoma
- Location
- Cause
- Demographics
- Clinical presentation
- Imaging
Between dura and arachnoid mater [potential space].
Rupture of bridging veins between the brain and major venous sinuses.
-
- Brain demonstrates some degree of movement within skull, while bridging veins are fixed → creates shearing forces that can tear veins.
- Infants: Non-accidental injury (child abuse)
- Young adults: Trauma (especially MVCs); vascular compromise (AVMs, infection, autoimmune disease, connective tissue disorders)
- Elderly/frail: Falls
Can be acute or chronic:
-
- Acute: Most patients present with some degree of altered consciousness or mentation. Can see focal neurologic deficits, especially pupillary abnormalities and slurred speech. Headache, nausea, and vomiting also very common.
- Chronic: Major cause of (potentially reversible) pseudodementia in the elderly.
Findings depend on age of bleed (hyperacute, acute, subacute, or chronic).
Hyperacute
- (<1 hour) Less-common scenario than acute/chronic.
- May note swirl sign on CT, representing a mixture of clot, serum and unclotted active bleeding.
Acute
- Classically seen as a hyperintense, crescent-shaped extra-axial collection.
- May rarely appear isodense in the setting of clotting disorders, anticoagulation, or severe anemia.
Subacute
- May be difficult to appreciate, due to tendency of aging clot toward isodensity with surrounding tissue.
- May see effacement of sulci or midline shift.
- Sulci may appear to “fade” into the subdural at the edges.
Chronic ( > 3 weeks old)
- Neomembrane formation: Composed of two layers (inner/outer), which secrete enzymes preventing clot formation. Seen exclusively in chronic SDH.
- Chronic subdural content is more liquid in consistency than that of a subacute bleed.
- The SDH becomes more hypodense on imaging over time, making the chronic bleed easier to appreciate than an isodensesubacute bleed.
- If bilateral, may not have significant midline shift.
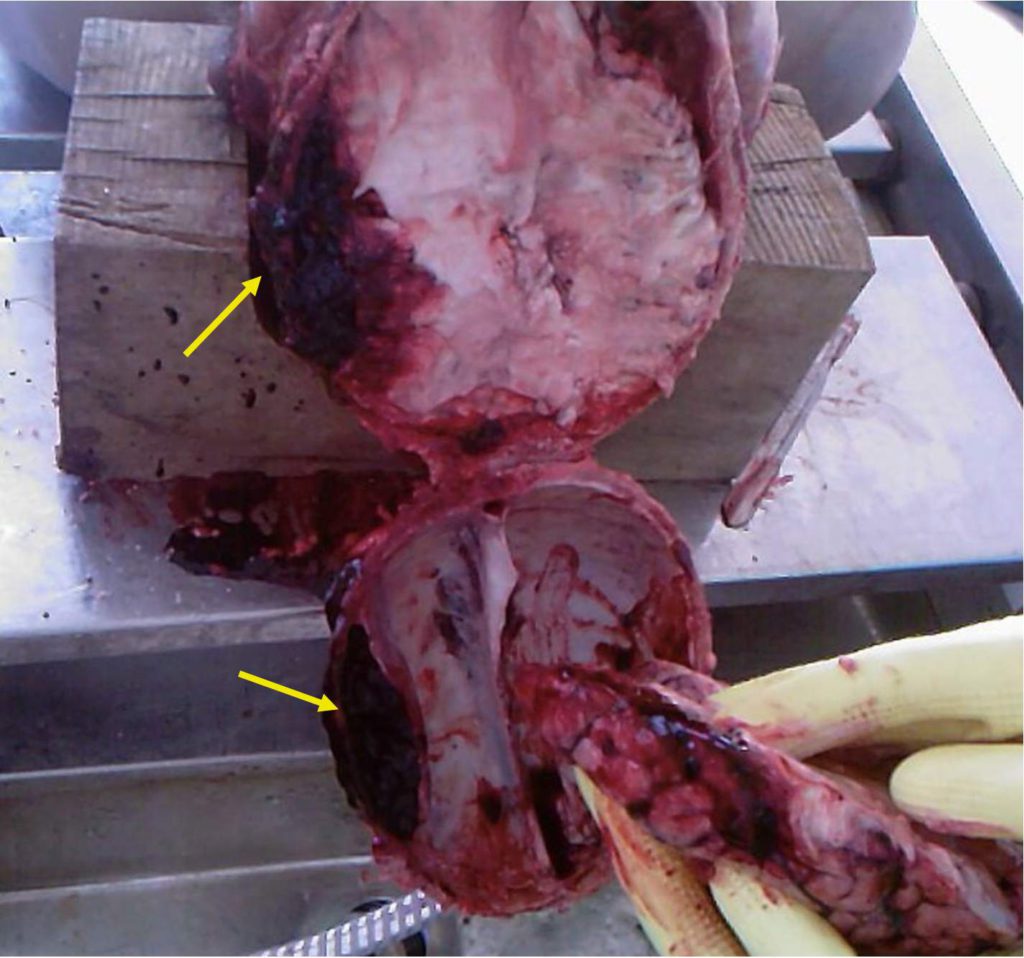
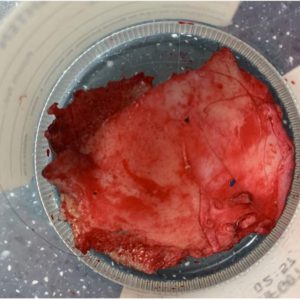
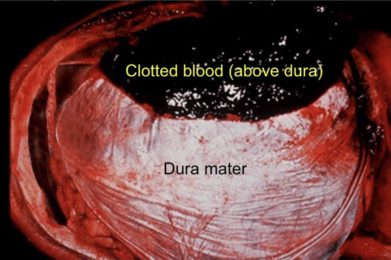
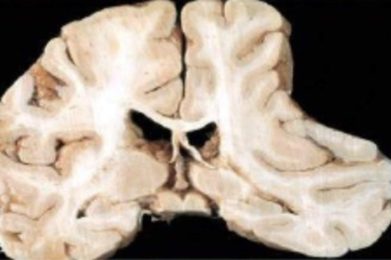
Gross (autopsy) findings

-
Blood between arachnoid and dura mater in crescentic shape. Radiopaedia.
-
Examination of dura for presence of neomembrane or focal thickening can help differentiate acute vs. chronic bleed.